Laparoscopic splenectomy is the method of choice for the treatment of multiple splenic diseases, with the well-known benefits of minimally invasive treatment.1–3 Laparoscopic partial splenectomy avoids the consequences of asplenia, although its use is uncommon.2,3 We present a patient with a splenic epidermoid cyst treated by laparoscopic partial splenectomy (LPS), and we will discuss its indications and technical aspects.
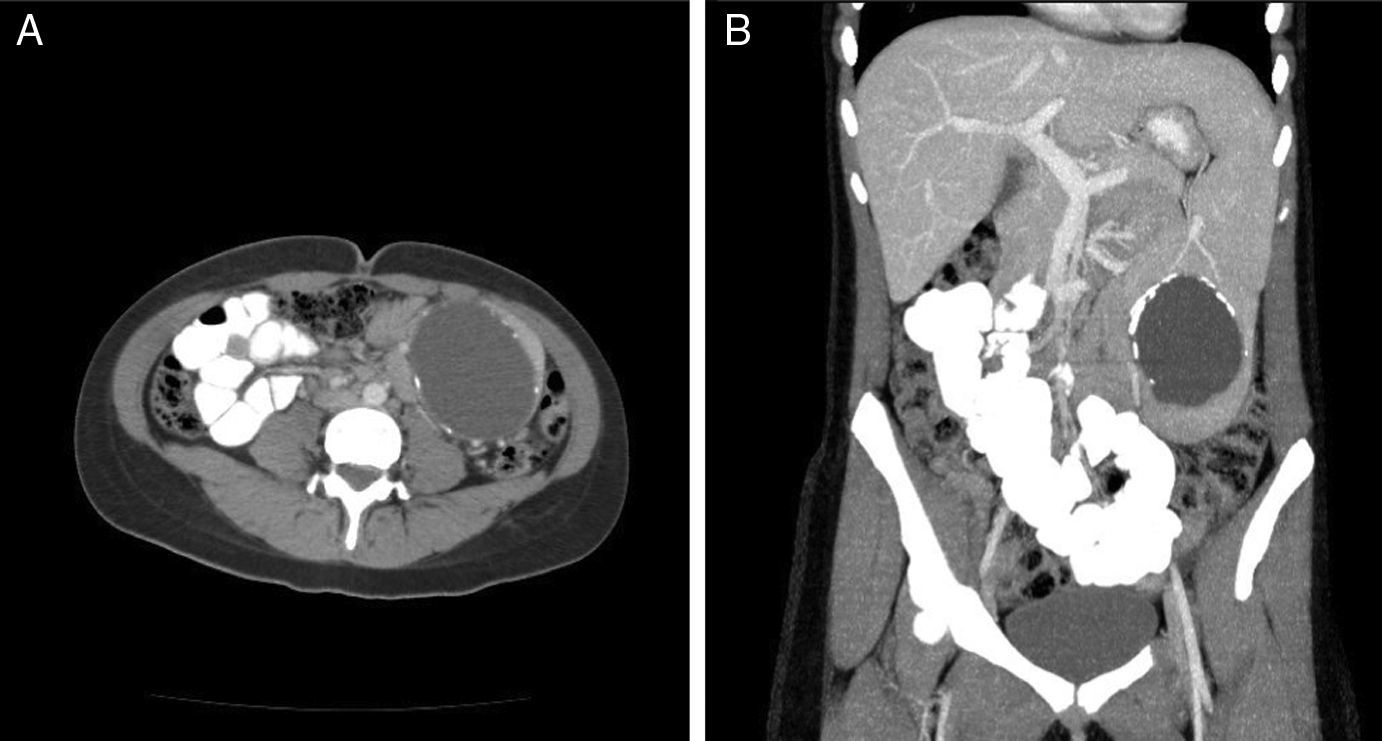
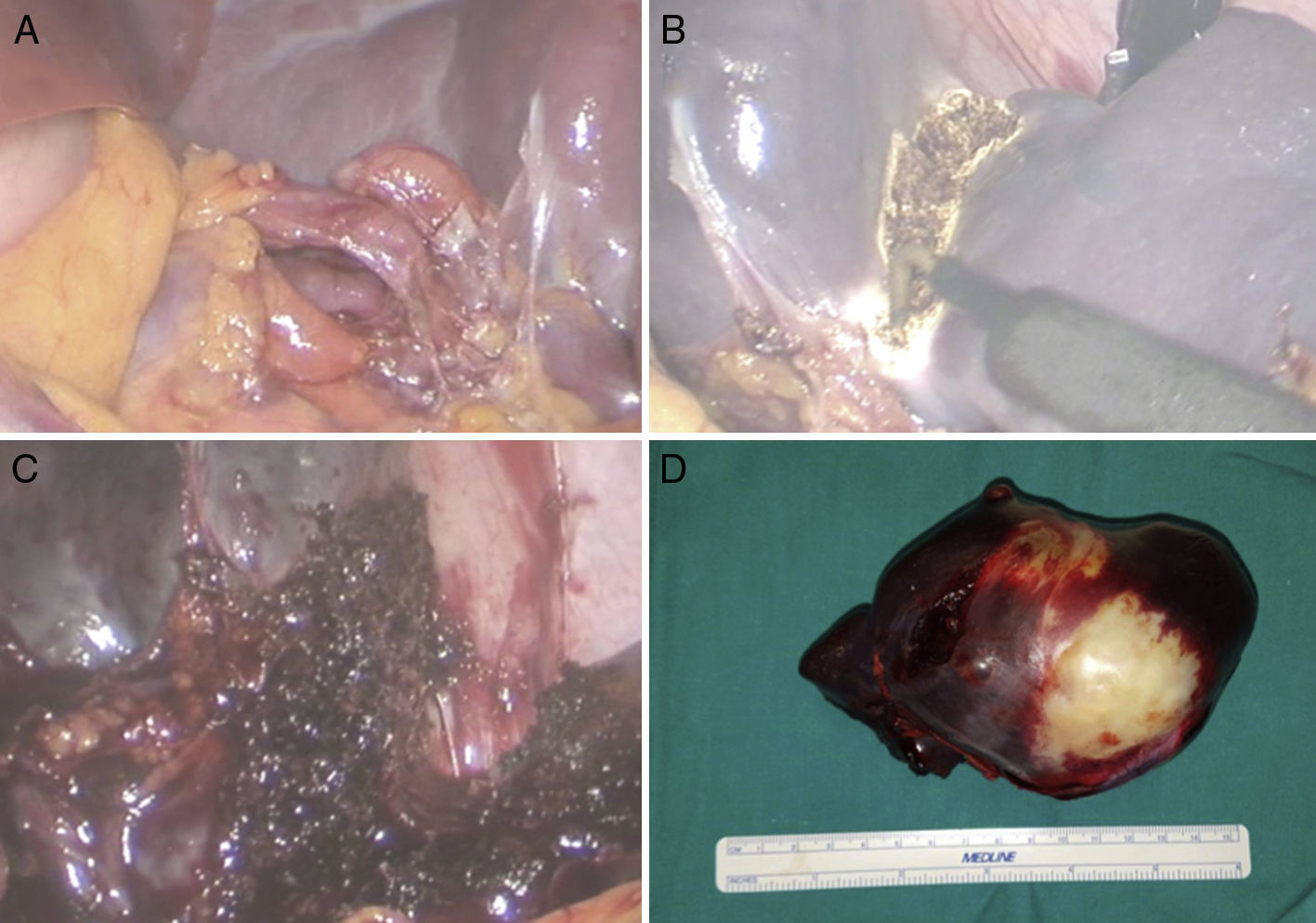
The patient is a 16-year-old female with a history of pneumonia due to Mycoplasma pneumoniae and infectious mononucleosis. The patient reported a self-palpated tumor in the left flank. On examination, a non-painful, mobile mass was palpable in the left hypochondrium and flank. Lab work showed no significant alterations: CA19-9 5.0IU/mL (normal range: 0–37). An abdominal CT was performed, which detected an 8-cm cystic lesion with calcified walls in the inferior pole of the spleen and splenomegaly (Fig. 1A and B). Hydatid serology was requested, which was negative. The surgical technique consisted of: supine position with abduction of lower limbs, induction of pneumoperitoneum with a Veress needle, placement of 4 trocars (2 infraumbilical and left flank [11mm] and 2 more in the right flank and subxiphoid [5mm]), clamping of the blood supply vessels of the lower pole, dissection of the parenchyma with monopolar coagulation and bipolar vessel sealing system, non-anatomical resection without release of the superior pole of the spleen, and removal of the specimen using a Pfannenstiel incision (Fig. 2A–D). Drains were not used. No hemostatic agents were used; blood loss was 130cc. The postoperative period transpired without incident, and the patient was discharged after 24h. The histological study identified the specimen as a splenic epidermoid cyst. Eight months later, the patient is asymptomatic and has had no recurrence. Informed consent was provided for the publication of images and hospital protocol.
Cystic lesions of the spleen are either parasitic (usually caused by Echinococcus granulosus) or non-parasitic, which are subdivided into primary and secondary lesions.4,5 Epidermoid cysts are considered primary congenital lesions. They account for 10% of all non-parasitic cysts and are the most frequent splenic cysts in children and adolescents.4,6 They present an incidence of 0.07% in the general population and are more frequent in women. Although the etiology is not clear, the most widely accepted theory is the inclusion of peritoneal mesothelial cells in the splenic parenchyma. These cysts are usually asymptomatic but can cause symptoms of compression (pain, digestive symptoms) if large, or they can become complicated (rupture or hemorrhage).4,7 The cysts are usually unilocular and may have wall calcifications. The differential diagnosis should basically include pseudocyst and splenic echinococcosis. There are several therapeutic options for epidermoid cysts, but surgical resection is the most cost-efficient and is recommended in symptomatic patients, complicated cysts or lesions larger than 5cm. The advantages of a complete resection of the cyst include no recurrence and avoiding complications related with the residual cavity.4–6
The first laparotomic partial splenectomy was performed by Morgenstern in 1980, and Uranüs performed the first LPS in 1995.1,2,5,8,9 Initial indications for partial splenectomy in the literature were: age younger than 60 years, grade II and III splenic trauma and benign disease.9 Currently, it is also performed in malignant disease.7 Although LPS is known to be feasible and safe, this is a technique that is not frequently performed.1,6–9 Most LPS have been performed as elective surgery, although they have also been occasionally used in splenic trauma.8 The most frequent indication is benign cysts,1,7 although LPS has been used in multiple benign and malignant splenic lesions: hemangioma, lymphangioma, hamartoma, angiomyolipoma, epidermoid cyst, hydatid cyst, trauma, spherocytosis, abscesses and infarctions, as well as in malignant primary and secondary tumors.1,8,10
The theoretical advantages of LPS are: those inherent to any laparoscopic procedure; preservation of immunological function, requiring a postoperative splenic remnant greater than 25% to avoid post-splenectomy sepsis, which presents a mortality of 2.1%3,5–9; and decrease in immediate postoperative morbidity.2,7,9 The disadvantages include: the technical difficulty, especially the transection of the splenic parenchyma; its non-applicability in central cysts with hilar involvement or those that are very large; the risk of recurrence in hematological diseases; and higher theoretical morbidity due to intraoperative complications, especially hemorrhage. To avoid the latter, we believe it is fundamental to clamp the polar arteries of the splenic segment that is going to be resected and to achieve perfect hemostasis of the splenic parenchyma.5,10
Splenectomy can be anatomical (when the distribution of splenic vascular structures is followed)3 or non-anatomical/irregular (when we adapt it to the splenic lesion, as in our patient). It is not necessary to mobilize the entire spleen to perform LPS; in fact, this may favor torsion.1,6,7 Splenic dissection is usually completed with sealants and/or staples. The use of radiofrequency can cause a wider area of necrotic parenchyma.2,6
The systematic review of the literature on LPS by Balaphas et al. in 2015 included 33 articles describing 187 LPS (168 laparoscopic, one single-port and 18 robotic).1 Forty-six patients were treated surgically for non-parasitic cysts. Morbidity was 5.4% and the average hospital stay ranged from 1 to 8 days.1 The overall conversion rate to laparotomy was less than 10%.1,3,5,7 When LPS is compared with total splenectomy, it is observed that there are no significant differences in operative time, bleeding and blood transfusion, but LPS presents lower morbidity, especially splenic thrombosis, pleural effusion and incisional hernias, and a certain decrease in hospital stay.1,2
In conclusion, LPS is a demanding but valid technique that is feasible in the treatment of splenic lesions, especially those located in the poles of the spleen, that reduces certain postoperative complications and maintains splenic immunological function.
Please cite this article as: Ramia JM, de la Plaza Llamas R, López-Marcano AJ, Valenzuela Torres JC, García Gil JM. Esplenectomía parcial laparoscópica por quiste epidermoide esplénico. Cir Esp. 2017;95:613–615.