Cirugia mínimamente invasiva de pared abdominal
Más datosIn this review, the advantages of the robotic platform in rTAPP are presented and discussed. Against the background of the unchanged results of conventional TAPP for decades (approx. 10% chronic pain and approx. 3.5% recurrence), a new anatomy-guided concept for endoscopic inguinal hernia repair with the robot is presented. The focus is on the identification of Hesselbach's ligament. The current results give hope that the results of TAPP can be improved by rTAPP and that rTAPP is not just a more expensive version of conventional TAPP. To support the rationale presented here, we analyzed 132 video recordings of rTAPP's for the anatomical structures depicted therein. The main finding is, that in all cases (132/132 or 100%) Hesselbach's ligament was present and following its lateral continuity with the ileopubic tract offered a safe framework to develop all the critical anatomical structures for clearing the myopectineal orifice, repair the posterior wall of the groin and perform a flawless mesh fixation. Future studies are needed to integrate all the resources of the robotic platform into an rTAPP concept that will lead out of the stalemate of the indisputably high rate of chronic pain and recurrences.
En esta revisión se presentan y discuten las ventajas de la plataforma robótica en la rTAPP. En el contexto de los resultados sin cambios de la rTAPP convencional durante décadas (aprox. 10% de dolor crónico y aprox. 3,5% de recidiva), se presenta un nuevo concepto guiado por la anatomía para la reparación endoscópica de la hernia inguinal con el robot. La atención se centra en la identificación del ligamento de Hesselbach. Los resultados actuales permiten albergar la esperanza de que los resultados de la TAPP puedan mejorarse con la rTAPP y de que esta no sea simplemente una versión más cara de la TAPP convencional. Para respaldar los argumentos aquí expuestos, hemos analizado 132 grabaciones de vídeo de rTAPP para las estructuras anatómicas representadas en ellas. El principal hallazgo es que en todos los casos (132/132 o el 100%) el ligamento de Hesselbach estaba presente y, siguiendo su continuidad lateral con el tracto ileopúbico, ofrecía un marco seguro para desarrollar todas las estructuras anatómicas críticas para despejar el orificio miopectíneo, reparar la pared posterior de la ingle y realizar una fijación impecable de la malla. Se necesitan estudios futuros para integrar todos los recursos de la plataforma robótica en un concepto de rTAPP que permita salir del estancamiento de la tasa indiscutiblemente elevada de dolor crónico y recidivas.
Conventional laparoscopic TAPP was introduced by visionary surgeons more than 30 years ago. At that time, endoscopic inguinal hernia repair had to compete with open repair procedures with optimal clinical outcomes, such as the Bassini, the Shouldice, or the Lichtenstein techniques. Back then, skepticism by the surgical community was mainly expressed due to disbelief in that a low-cost procedure, typically done under local anesthesia (e.g., Shouldice and Lichtenstein) should now be performed minimally invasively, at greater costs and efforts. However, in retrospect, it should be admitted that minimally invasive procedures have significantly reduced the risk of chronic postoperative pain compared with open procedures, thus offering a better quality of life and postoperative course for the patients.1–3 Advancements in science will never come to an end. Nowadays, 50 years after the first landing, humanity is on the verge of repeating its journey to the moon, but this time with newer equipment replacing the older craft. Similarly in the world of science, cutting-edge technologies, with higher precision and measurement accuracy, along with capacity to process larger datasets – thanks to artificial intelligence – would bring new insights to replace old knowledge. In that perspective, robotic surgery should be given the opportunity to be evaluated in its application in inguinal hernia repair. This stance also takes birth from the rapidly increasing adoption rate of robotic surgery across different specialties, with hernia repairs benefitting from the highest growth in adoption rate (in 2021, there were over 9000 inguinal hernias and over 7000 ventral hernias in U.S. academic hospitals; public data from Intuitive).
The legacy of laparoscopic TAPP (TAPP results)In general, endoscopic procedures (both TEP and TAPP) for inguinal hernia repair (posterior approach) result in less chronic pain than open procedures (anterior approach), with comparable recurrence rates. Most complications after mesh implantation occur following anterior procedures. The eye-opening study on this fact is a randomized control trial by the Agneta Montgomery's group, in which a comparison of TEP and Lichtenstein procedure in 1512 patients showed that chronic pain occurred in 11.0% versus 21.7% respectively, at one year. This finding remained valid (p<0.001) at 5 years with 9.4% versus 18.8%, respectively.4 Similar findings were reported in the study by Reinhard Bittner and Henrik Kehlet who compared two cohorts (TAPP and Lichtenstein).5
Posterior procedures also result in lower rates of chronic pain in the management of recurrent hernias. In a meta-analysis from 2015, with a total of 647 patients, chronic pain occurred in 9.2% of endoscopically reoperated patients versus 21.5% of patients who underwent an open repair.2 Even if conventional TAPP, with a similar recurrence incidence as open procedures, causes less chronic pain than anterior procedures, it must be noted that 9.4% chronic pain after 5 years is a high rate. Hernia recurrence rate of TAPP in studies ranges between 0 and 25% (median 2.3%) with the general recurrence rate of inguinal hernia repair being estimated between 10 and 15%, all techniques included.6 With quality of life becoming an increasingly crucial component of patient care, the surgical community should not settle with the current results of conventional TAPP and current inguinal hernia repair as a whole.
Of particular importance, endoscopic inguinal hernia repair shifted the focus over the course of the 30 years from the “easy and fast” characteristic of anterior procedures to the “look closely at the anatomy and pay attention” mentality of posterior procedures. Recognition should be given to the summaries of Jorge Daes (“critical view of the myopectineal orifice”),7 Flavio Malcher (“ten golden rules for a safe MIS inguinal hernia repair”),8 and Daiki Yasukawa (“crucial anatomy for TAPP repair”).9 Although these manuscripts document this change, new aspects with robotics will be discussed below.
What can robotic technology contribute?Robotic rTAPP is the natural evolution of the conventional laparoscopic TAPP. Common to both techniques are the transabdominal access (with the advantage of diagnostic laparoscopy), three ports for entry, long instruments, and the option of different endoscopes (30° or 0°). Conventional TAPP uses thinner instruments (5mm) than rTAPP (8mm). Similarities end at this point. New features are being added to the current robotic systems to foster more precise surgery: Immersive view (no distraction, contemplative work, promotes curiosity), camera control by the surgeon, improved ergonomics (longer endurance to achieve a perfect result, with minimal workload), standardized distances to the target organ (the position of the umbilicus no longer dictates the position of the endoscope port, but the distance to the symphysis does), the angulation of the instruments’ tip (which allows 7 degrees of freedom), and the compensation for the smallest tremor by the system (which is of significant advantage in recurrences and coagulation near sensitive structures). In addition, the implementation of intraoperative checklists10 and the use of dual consoles are very efficient teaching tools. Teaching at the dual console and training of the younger generation on a simulator are of major importance to achieve the learning curve before independently operate on patients and to increase expertise with each consecutive case. The repeatedly criticized longer operative time of rTAPP compared to conventional TAPP is not due to docking: with rTAPP, the time from the beginning of the pneumoperitoneum, setting the ports, docking with targeting, and starting at the console takes about 4–5min.10 The longer operative time is essentially due to the increased attention to anatomy and preventive measures, such as identification of all sensitive structures (e.g., nerves) and reconstruction of the posterior wall of the inguinal canal. This extra investment of time would most likely pay off in the long run, in terms of better clinical outcomes (less chronic pain and fewer recurrences). A new aspect of robotics is the “lifting of the abdominal wall” by the ports attached to the cart (clutch): this feature allows to work with a lower pneumoperitoneum pressure (e.g., 8–10mmHg), while ensuring unobstructed access to the groin. This is especially beneficial for elderly patients and those with cardiopulmonary diseases. This feature enabled to extension of endoscopic inguinal hernia repair to patients with higher comorbidities and BMI. These candidates can also benefit from less chronic pain and faster return to activities daily life. A study including 304 rTAPP operations has already demonstrated that BMI has no negative influence on surgical outcomes, except for the longer operation time.11
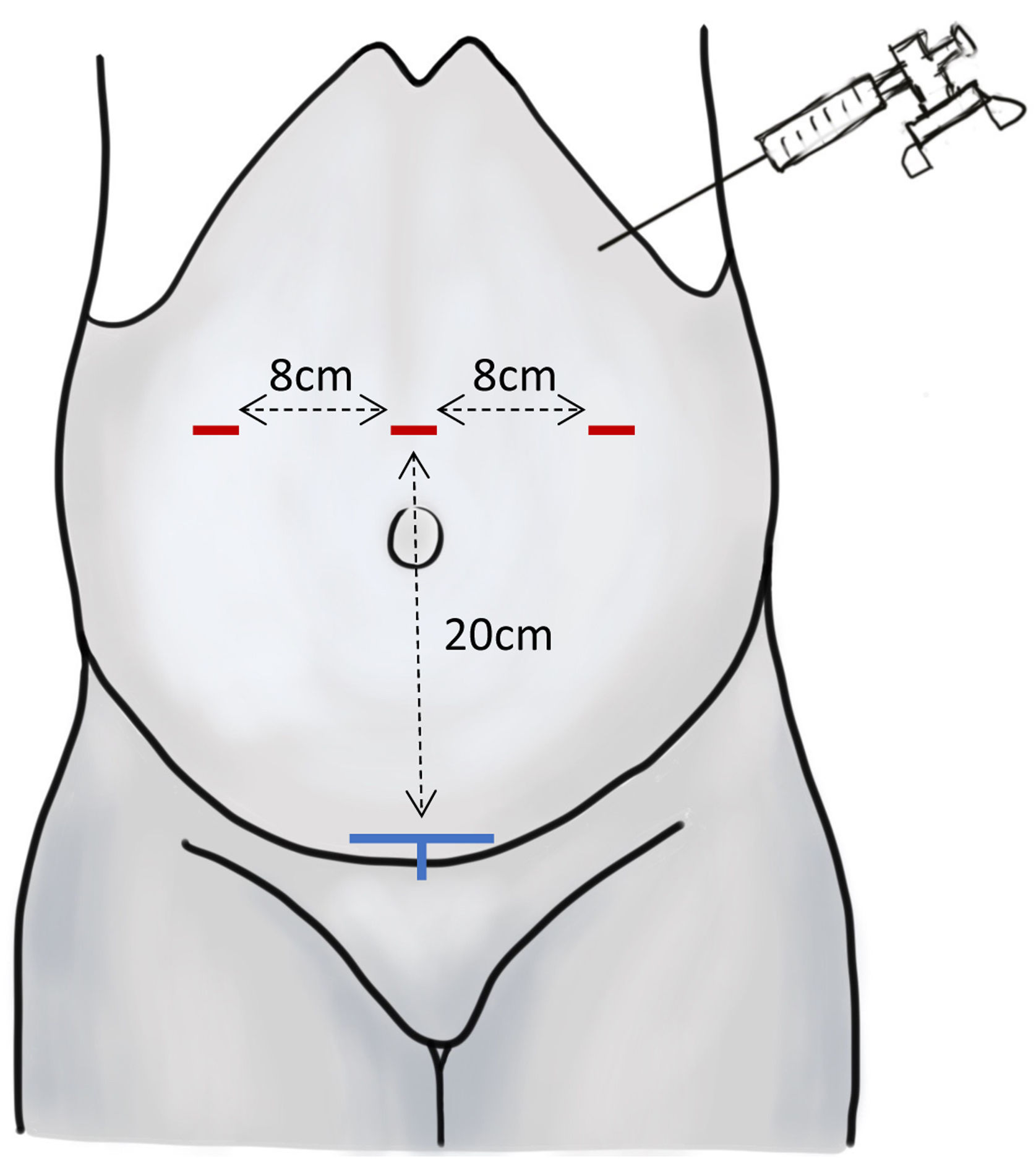
From a purely anatomical point of view, port positioning with rTAPP focuses on the optimal distance of 20cm between the port line and the target organ (e.g. symphysis), thus providing a higher degree of standardization over conventional TAPP, since the latter uses the umbilicus as an access-site. The variability in the distance between the umbilicus and the symphysis, the distensibility of the abdomen due to the pneumoperitoneum, and the angle of abdominal wall elevation between both symphysis and umbilicus, can vary greatly, generating additional technical challenges in conventional TAPP procedures. Distance between each port should be 8cm to ensure an unobstructed movement of each robotic arm (Fig. 1 – port positioning). Future anthropometric studies will need to collect more data on this aspect to quantify the influence of core anatomy on both the quality of outcome and the degree of difficulty of surgery in both laparoscopic and robotic procedures.
Port positioning for the rTAPP, after installation of the pneumoperitoneum with the Veres needle. Red markings: skin incisions; blue markings: symphysis (target organ for bilateral rTAPP).
In our own initial cohort of 302 rTAPP inguinal hernias, we have been able to specify the relevant surgical steps and their adaptation to the robotic technique.10 Our ingenious team members focused on the intraoperative standardized checklist and working with the dual console.10 In order to ensure optimal quality of outcomes and simultaneously allow the possibility for further qualification of a trainee, the individual surgical steps (called entrustable professional activities) are passed back-and-forth between surgeon and trainee in alternation: the trainee does only the specific steps that they can perform flawlessly. In order to optimize operative time, the main surgeon would take over the easier steps (which the trainee has already mastered) leaving the more challenging ones to the trainee; thus, the stress of the operation is also reduced for the trainee (Yerkes-Dodson Law).13 For example, a trainee may cut open and re-suture the peritoneum, fixate the mesh, and dissect the hernia gaps, all more than 10 times, while maintaining each time to the surgical timeline and quality of outcome: after 30 procedures, the trainee would have performed the equivalent of 10 complete surgeries (Fig. 2 – My Intuitive App). These individual steps are documented and graded in correlation with the difficulty level of the respective patient. Through targeted feedback, the trainee goes back to the simulator and practices what they still need to improve. For example, the speed of suturing and knotting, or the flawless handling of monopolar coagulation should not be practiced on the patient, but on the simulator.
Example of dual-console work. (a) The change between console 2 (senior operator) and console 1 (trainee) in the upper example (#488) occurs only at the beginning (blue arrow, opening of the peritoneum) and at the end of the operation (blue arrow, mesh fixation and suturing of the peritoneum); (b) in the example below (#487), the trainee (console 1, yellow arrow) is significantly more involved in the procedure, the senior surgeon (console 2) starts with the easiest part to gain time (opening of the peritoneum) and from then on always briefly takes over the procedure at critical steps in order not to compromise the quality of outcome for the patient. From: Senior surgeon user account, My Intuitive App.
Robotic TAPP focuses less on the structures that can be injured and more on the identification of anatomical landmarks that allow the surgeon to masterfully control the variables in all the steps of the procedure. This new preparation concept has a focus on musculoaponeurotic leading structures, as hernias are a musculoaponeurotic occurence. The following steps are systematically used:
- 1)
Creation of a large peritoneal flap from lateral to medial.
- 2)
Medial exposure of the symphysis, by opening the vesicohypogastric fascia. This corresponds to the visceral compartment of the fascia intermedia. We not deem the subperitoneal dissection required by some authors in conventional TAPP to be correct, nor is it feasible to keep this imaginary plane due to embryological reasons.14
- 3)
Lateral visualization of the fascia intermedia. The fascia intermedia divides the inguinal region into a parietal (lateral) compartment and a visceral (medial) compartment. In the parietal compartment, the fascia iliaca and the subjacent nerves (lateral cutaneofemoris nerve and genitofemoral nerve) are identified, as well as the deep circumflex iliac artery.
- 4)
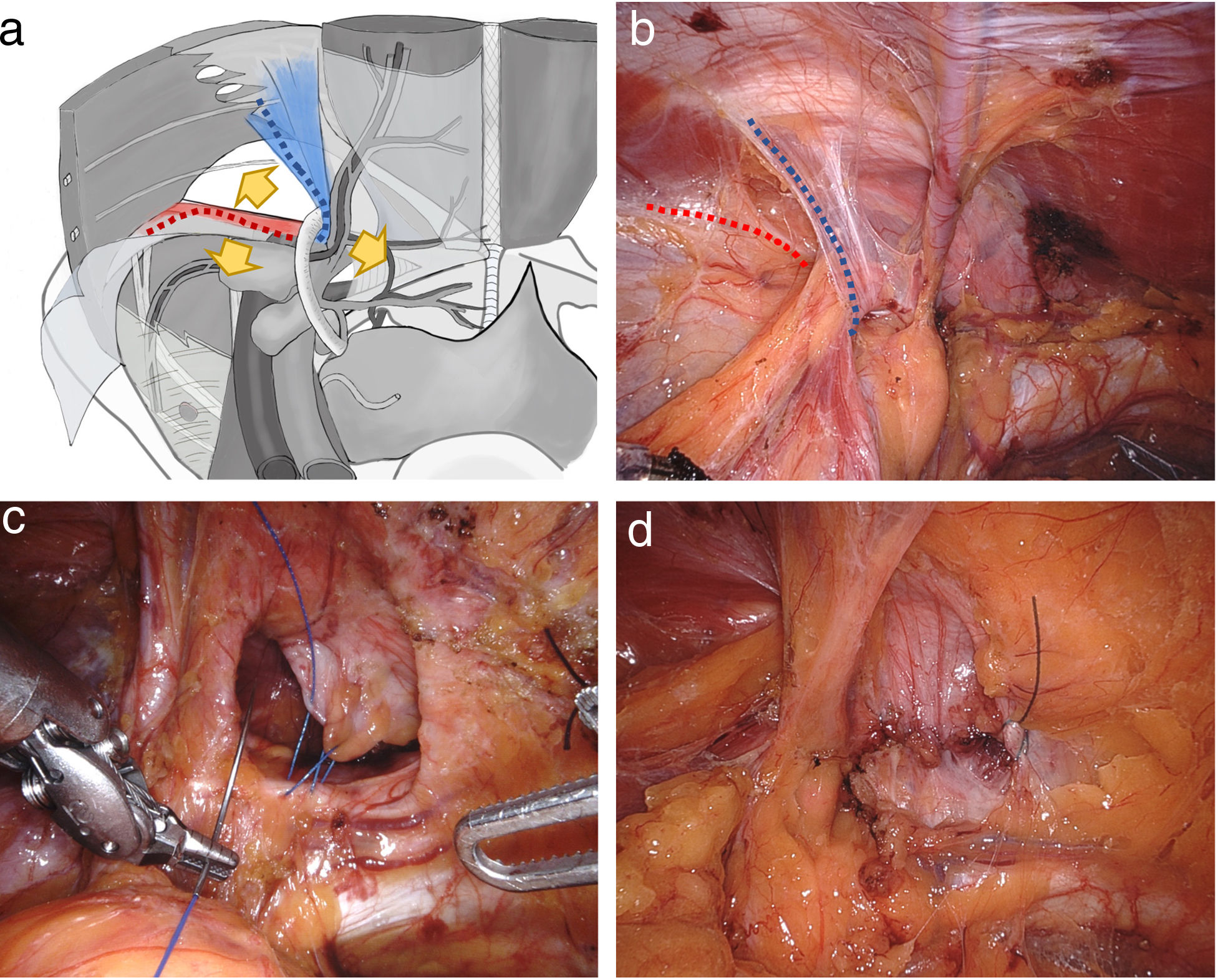
From there, the Hesselbach ligament (interfoveolar ligament) is exposed, wrapping around the funiculus spermaticus laterally into the iliopubicus tract (Fig. 3a and b). Hesselbach's ligament is usually identifiable (in our series of 132 patients it was present in 100% of the cases; see Table 1). Medial to Hesselbach's ligament, the medial and femoral hernias are found. Dorsal to the iliopubic tract run both branches of the genitofemoral nerve, the fatty tissue at this site embeds lymph nodes; these structures must be avoided.
Fig. 3.Preparation on the myopectineal orifice. (a and b) The start of the procedure fis at Hesselbach's ligament, from where all structures of the myopectineal orifice are developed (Hesselbach's ligament=blue dashed line; ileopubic tract=red dashed line); the yellow arrows show the 3 pathways for dissection; (c and d) Example of morphological reconstruction of the posterior wall of the inguinal canal in a medial hernia.
(0.53MB).3a: Modified from Kudsi et al.12.Table 1.Detected anatomical structures in the video review.
Yes % No % Structural landmarks Intermediate fascia 132 100 – – Iliac fascia 132 100 – – Rectus abdominis fascia 123 93.1 9 6.8 Hesselbach's ligament (interfoveolar ligament) 126 95.4 6 4.5 Henle's ligament 21 15.9 111 84.1 Pubic symphysis 132 100 – – Cooper's ligament 129 96.2 3 2.2 Lacunar ligament 84 63.6 48 36.3 Myopectineal orifice 132 100 – – Hesselbach's triangle 131 99.2 1 0.7 Nerves Lateral cutaneus femoral nerve 127 95.4 5 3.7 Genital branch of the genitofemoral nerve 78 59 54 40.9 Below iliopubic tract 61 78.2 Above iliopubic tract 8 10.2 Transit not visible 9 11.5 Ilioinguinal nerve 1 0.7 131 99.3 Vessels Deep circumflex iliac artery 86 65.9 46 34.1 Epigastric artery 132 100 Rectusial veins 121 91.6 11 8.33 Corona mortis 112 92.3 20 15.1 Lymphnodes Iliac lymphnodes 101 76.5 31 23.4 Femoral lymphnodes 53 40.1 79 59.8 Lipomas Lipoma with pedicle 89 67.4 Lipoma without pedicle 59 44.6 In bold: structures detected in all videos.
- 5)
Cranial to the iliopubic tract is the internal inguinal ring. Here, lateral hernia can be found with, craniolaterally to it, Spieghel hernias can be located. Three types of lipomas can be retrieved from the inguinal canal: those without a vascular pedicle, dorsally pedunculated lipomas (from the lateral abdominal wall), and cranially pedunculated ones (from a branch of the deep circumflex iliac artery).
- 6)
Next, a wide dorsal parietalization on the psoas muscle, laterally into the Bogros space and deep into the spatium Retzii is completed. At the end of the parietalization, the landing zone for the mesh is on the musculoaponeurotic substrate and without adipose tissue remaining.
- 7)
In case of a medial hernia, the transversal fascia is cut open over the inguinal ligament and suture retraction of the aponeurosis of the transversus muscle to the inguinal ligament is performed, paying close attention to avoid grasping the elements of the funiculus spermaticus that transit behind the transversal fascia with the suture (Fig. 3c and d).
- 8)
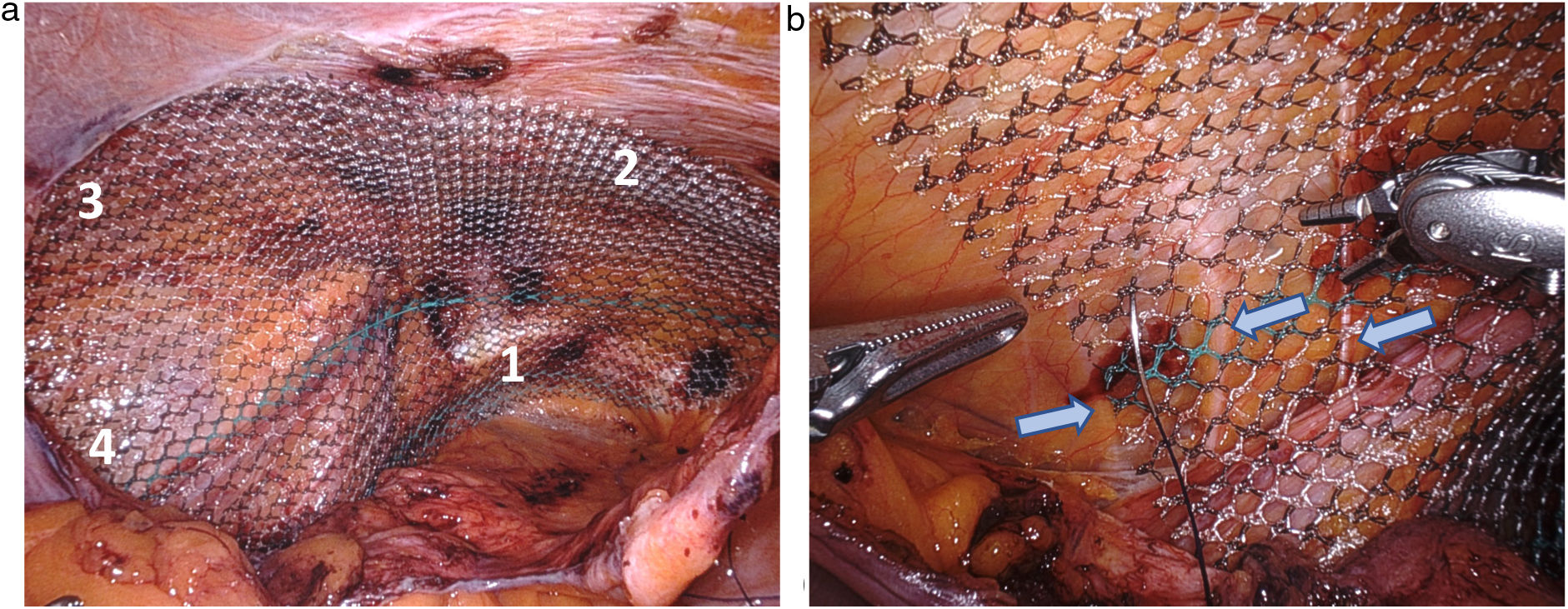
Positioning of a large mesh (at least 10cm×15cm, ideally 12cm×17cm) with coverage of the entire myopectineal orifice. Mesh fixation with 4 sutures from medial to lateral: on the Cooper's ligament, on the fascia of the rectus abdominis muscle, on the transversus abdominis muscle and on the iliac fascia (with visual exclusion of the nerves running nearby underneath) (Fig. 4).
Fig. 4.Mesh positioning and fixation. (a) Mesh is fixed from medial to lateral to (1) Cooper's ligament, (2) the fascia of the rectus abdominis muscle, (3) the transversus abdominis muscle, and (4) to the iliac fascia. (b) Detail of fixation of mesh to the iliac fascia, passing the needle with the nerves left out (blue arrows).
(0.4MB). - 9)
Suture closure of the peritoneum from lateral to medial.
Since the concept elaborated above depends on unambiguous anatomic navigation, we examined the structures surrounding the myopectineal orifice and their identification during rTAPP. We retrospectively evaluated the unedited video recordings of 132 consecutive rTAPPs (May 2020–January 2021) and annotated the 20 important anatomic landmarks and structures of the inguinal region. A surgeon who was not involved in the procedures analyzed the videos. The videos were processed according to the terms of use of the video material with patient consent and in accordance with a positive vote of the Ethics Committee (see below). 32 patients (94,7%) were male, the mean BMI was 25.1kg/m2, 83 (62,8%) were right sided hernias, 55 (41.6%) were recurrent hernias, 95 (71.9%) were teaching procedures; the mean operating time (including bilateral and recurrent hernias) was 97.8min (range 31–172min, median 95.5min). There were 199 hernias in 132 patients, 49 hernias were medial, 98 hernias were lateral (with peritoneal sac), 14 were lateral hernias with lipoma only, 28 were femoral hernias and 10 were Spighelian hernias. The most important finding is, that in all cases Hesselbach's ligament was present (Table 1) and following its lateral continuity with the ileopubic tract offered a safe framework to develop all the critical anatomical structures for clearing the myopectineal orifice, repair the posterior wall of the groin and perform a flawless mesh fixation.
Future potential of rTAPPThe results of conventional TAPP are unhindered after more than 30 years of its conception, despite the increasing expertise of a whole generation of surgeons. People have become used to the fact that recurrences and chronic pain are method-immanent. Robotic TAPP has already proven to have lower recurrence and conversion rates.15 With rTAPP, the science cycle begins anew. Perhaps the smallest but probably not insignificant advantage of rTAPP is the mesh fixation in the area of the Triangle of Pain on the iliac fascia. Mesh displacements along with the loosening of the lower edge of the mesh are – besides protrusion through Hesselbach's triangle – the most frequent causes of recurrence.16 The multiple features and capabilities of the robotic platform will generate new opportunities. Intricate observation of the organ structures will provide new perspectives for the anatomy of the myopectineal orifice. The ongoing introduction of measurement and feedback tools e.g., for testing blood flow to the funiculus spermaticus using ICG angiography (Firefly technology) will empower surgeons and improve the safety for patients (Fig. 5). The learning curve to master the robotic procedure seems to be lower than laparoscopic17–19 and the transition from laparoscopic to robotic to be smooth.20 At-risk population (obesity, inguinoscrotal findings, or anticoagulation) can benefit from the multiple advantages of minimally invasive surgery.21 Moreover, recurrent hernias, mesh explantations, and inguinal hernia repair after prostatectomy or previous laparotomy are good indications for rTAPP in the hands of experienced robotic surgeons.22 With the current trend in the United States for patients to opt for mesh-free repairs, robotic surgery also offers the opportunity to perform pure tissue repair (or ileopubic tract repair), without mesh implantation: the minimally invasive approach does not involve the ilioinguinal and iliohypogastric nerves, which are at risk for causing CPIP in anterior approach procedures.23 We understand that healthcare actors evaluate groin hernia repair from a financial point of view; but routine procedures should be performed with the best possible approach. The rTAPP technique is an important element in the training of residents who will later move on to more sophisticated visceral procedures. The fact that the work console and the simulator are the same device is an important contribution to shifting the learning curve to a preclinical setting. Moreover, with further training and establishment of efficient robotic centers, rTAPP may be performed in emergency inguinal hernia repairs.24
Example of the use of ICG angiography to confirm arterial perfusion (early phase) and venous outflow of the testis (late phase). Venous phase is shown in example (b). Yellow star=cranially pedunculated lipoma; blue arrow=genital branch of the genitofemoral nerve; monopolar scissors encompass the funiculus spermaticus proximal to the deep inguinal ring in (a) and (b).
So how should rTAPP be compared to conventional TAPP25? Does “equivalence” describe comprehensively both procedures? Is rTAPP merely an expensive version of the conventional TAPP26? This may be true in the hands of some surgeons: if the robotic platform simply aims to replicate the laparoscopic experience, then it makes little to no sense at all. If the smartphone was exclusively designed to make phone calls, how would it differ from the old landline phone, if the panoply of apps opportunities to be connected with the world were ignored. The task of future studies is to integrate all the resources of the robotic platform into an rTAPP concept that will lead out of the stalemate of the indisputably high rate of chronic pain and recurrences. It is the responsibility of surgeons to continue to improve patient outcomes, further developing the precious legacy of the past while maturing the conventional TAPP into the rTAPP. In the distant future, the whole TAPP concept may be superseded by a new approach that cannot be imagined yet. But currently, in the hands of ambitious surgeons, rTAPP is the best minimally invasive procedure available for inguinal hernia repair.
Ethics voteThe data collection of this study is based on a positive ethics vote of the Ethics Committee Northwestern Switzerland (No. 2019-02046).
FundingThe study was funded by internal hospital resources, with no third-party involvement.
Conflicts of interestThe Kantonsspital Olten is European Reference Center for DaVinci Hernia Surgery (Intuitive) since 2019; U. A. Dietz is proctor for Intuitive, the income from this activity goes in full to the KSO. OY Kudsi is proctor for Intuitive. All other authors have no conflicts of interest to disclose.