Mantle cell lymphoma (MCL) represents 4% of lymphomas in the United States and 7%–9% in Europe. This lymphoma is diagnosed in patients with an average age of 60, and most frequently affect males (ratio 2:1).1 In spite of its extralymphatic involvement (digestive tract, stomach, colon, liver, skin, lacrimal glands and central nervous system),1 MCL located in the breasts is uncommon.2 We present the clinical case of a male patient with MCL of the breast, in whom surgery provided adequate local control.
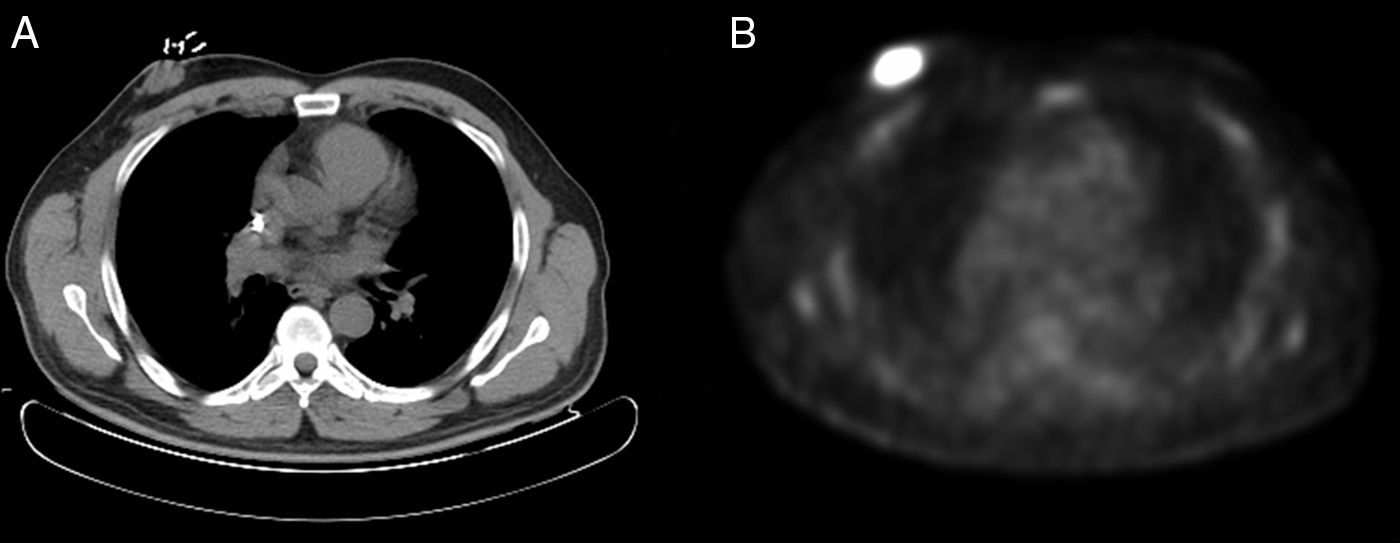
The patient is a 56-year-old man diagnosed with stage IIA blastoid MCL, diagnosed by cervical and right axillary lymphadenopathies. He was initially treated with radiotherapy of the affected field (total dose 47Gy) and rituximab (4 doses), as he refused treatment with polychemotherapy. Complete remission was reached, but 2 months after finalizing treatment he presented a relapse with supradiaphragmatic lymphadenopathies and a retroareolar mass in the right breast, with a biopsy that was compatible with blastoid MCL (Ki-67: 75%). For this reason, a second line of treatment was initiated with alternating R-CHOP/R-DHAP chemotherapy (4 cycles). When the response was evaluated after one month, evidence of partial response was observed, and PET/CT showed persistence of the right retroareolar mass (Fig. 1).
Given the partial response to treatment and due to the solitary location of the lymphoma in the right breast, we decided to resect the mass. Using a Stewart incision, we found a mass causing nipple retraction and conducted a simple mastectomy. The pathology study reported a mass measuring 4×2.5×3.7cm, proximal to the deep resection margin, identified as an MCL (aggressive or blastoid), with 20–22 mitoses per 10 high-power fields. In the immunohistochemistry analysis, the mass expressed CD20, CD79a, Bcl-2, PAX5 and CD5 with intense cyclin D1 overexpression and showed lambda light chain restriction; the proliferative index (Ki-67) was 70%, and a moderate expression of p53 was identified.
After another evaluation of the disease one month after surgery, complete remission was observed, at which time an autologous peripheral blood transplantation was performed. Eleven months after the transplantation, a new systemic recurrence was observed, and the patient died due to an invasive fungal infection after neutropenic fever two months later.
Primary breast lymphoma is rare, comprising 1% of non-Hodgkin's lymphomas and less than 3% of extranodal lymphomas.2 The definition of primary breast lymphoma provided by Wiseman and Liao3 and modified by Hugh et al.4 requires the presence of breast tissue very close to the lymphoma, the absence of a personal history of lymphoma and no extramammary dissemination except for the ipsilateral lymph nodes. Secondary breast lymphoma, which is more frequent, is defined as the presence of systemic lymphoma with simultaneous or subsequent breast involvement. In clinical practice, it is difficult to distinguish between primary mammary involvement with secondary dissemination and primary involvement in another area with secondary mammary involvement.2 In the case presented, the lymphoma was secondary.
MCL is a non-Hodgkin's lymphoma characterized by the involvement of lymph nodes, spleen, blood and bone marrow, with a short period of remission following conventional therapies.1 There are 3 histological growth patterns (mantle, nodular and diffuse) and 4 cytological variations (classical, small-cell, pleomorphic and blastic).5 The t(11:14) chromosomal translocation is the distinctive molecular alteration, with overexpression of cyclin D1. According to the MCL International Prognostic Index, low-risk patients have a 5-year overall survival of 60%, moderate-risk patients have a median overall survival of 51 months, and high-risk patients have a median overall survival of 29 months.1
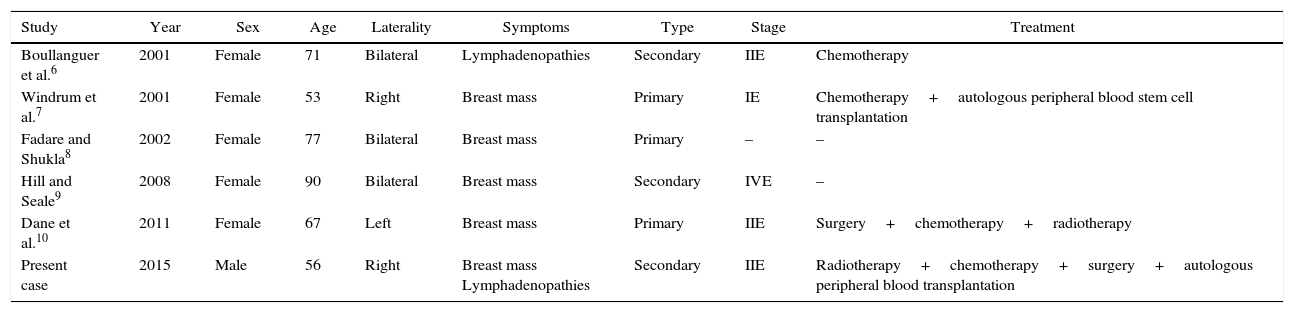
There are few case reports in the literature of MCL of the breast (Table 1),6–10 and, to our knowledge, this case is the first describing MCL of the breast in a male.
Published Cases of Mantle Cell Lymphoma in the Breast.
| Study | Year | Sex | Age | Laterality | Symptoms | Type | Stage | Treatment |
|---|---|---|---|---|---|---|---|---|
| Boullanguer et al.6 | 2001 | Female | 71 | Bilateral | Lymphadenopathies | Secondary | IIE | Chemotherapy |
| Windrum et al.7 | 2001 | Female | 53 | Right | Breast mass | Primary | IE | Chemotherapy+autologous peripheral blood stem cell transplantation |
| Fadare and Shukla8 | 2002 | Female | 77 | Bilateral | Breast mass | Primary | – | – |
| Hill and Seale9 | 2008 | Female | 90 | Bilateral | Breast mass | Secondary | IVE | – |
| Dane et al.10 | 2011 | Female | 67 | Left | Breast mass | Primary | IIE | Surgery+chemotherapy+radiotherapy |
| Present case | 2015 | Male | 56 | Right | Breast mass Lymphadenopathies | Secondary | IIE | Radiotherapy+chemotherapy+surgery+autologous peripheral blood transplantation |
Optimal therapy includes R-CHOP chemotherapy and locoregional radiotherapy, which appear to reduce the risk of local recurrence.1,2 Surgical resection of breast lymphomas has demonstrated poor local control. In patients treated with surgery alone, in stages IE and IIE the 5-year overall survival rates are 40.5 and 20.5%, respectively. Hence, surgical resection should be avoided and is indicated only to obtain biopsies.2 In the cases of breast MCL described in the literature, only one surgical resection was performed, which, combined with chemotherapy and radiotherapy, resulted in an overall survival of 73 months.10 In our case, complete remission was achieved for 11 months.
Therefore, considering the exceptional nature of this single case and even though it is in direct contrast with what is stated in the literature, in patients with MCL of the breast, surgery could be useful to prolong the period of complete remission.
Please cite this article as: Ruiz Pardo J, López López V, Blanquer Blanquer M, Cabezas Herrera J, Piñero Madrona A. Afectación mamaria por linfoma de células del manto en un varón. Cir Esp. 2017;95:170–172.