Endosalpingiosis is the presence of ciliated tubal-type epithelium in an ectopic location other than its normal origin in the Fallopian tubes.1 There have been no studies that clarify the most prevalent signs and symptoms of endosalpingiosis. Patients may present pelvic pain or chronic pelvic inflammation, or endosalpingiosis may be found incidentally during surgery.2–4 Occasionally, they may even manifest like tumors.5 Even when benign in nature, there are case reports of malignant transformation to papillary serous adenocarcinoma.4
We present the case of a 67-year-old woman with a medical history of hypertension, dyslipidemia and hysterectomy due to symptomatic uterine fibroids with postoperative pelvic pain. She was currently being studied due to constipation for several months that could not be resolved with hygienic, dietary or pharmacological measures. In addition, the patient reported an important amount of weight loss, together with rectal and vaginal bleeding.
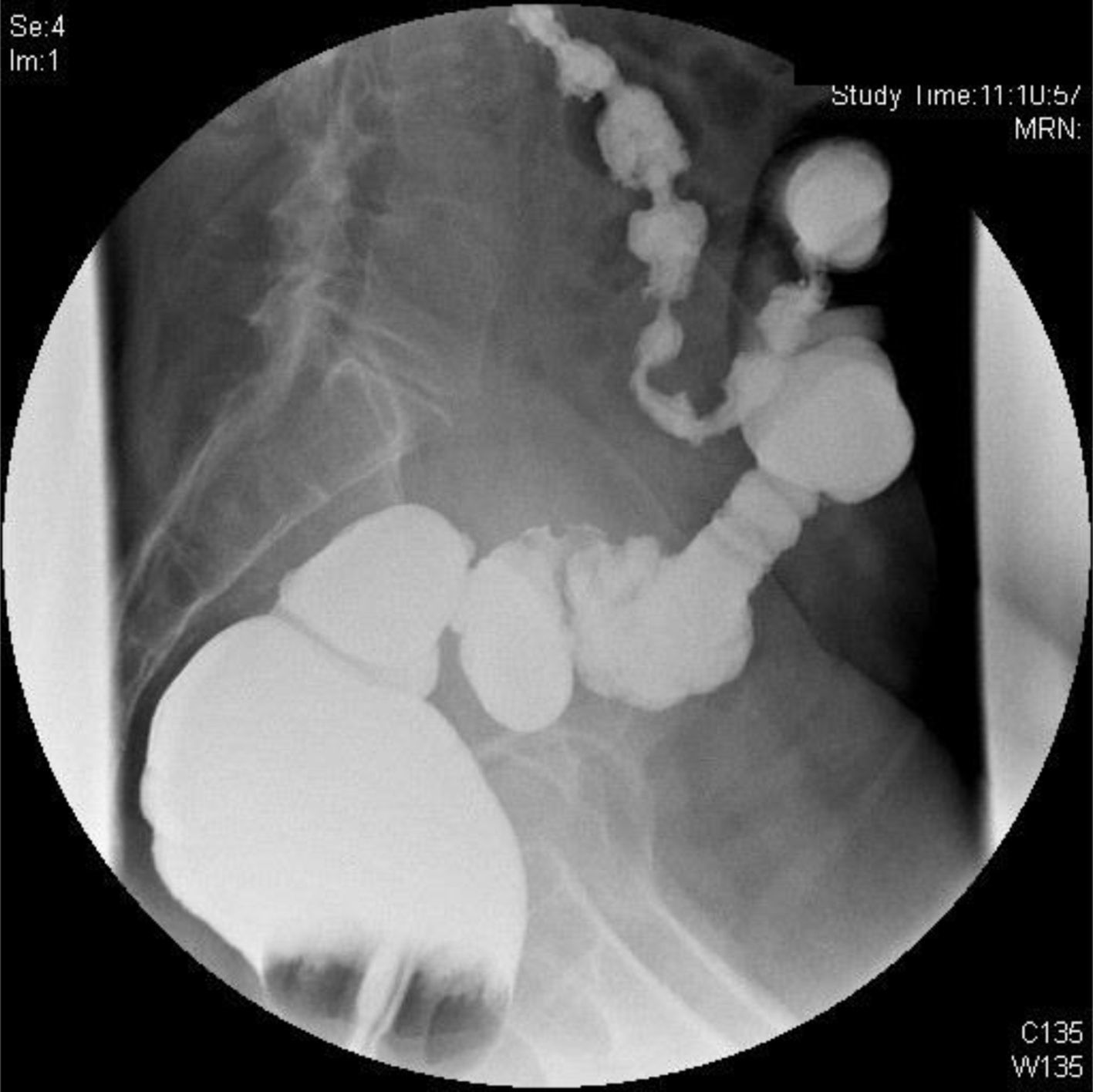
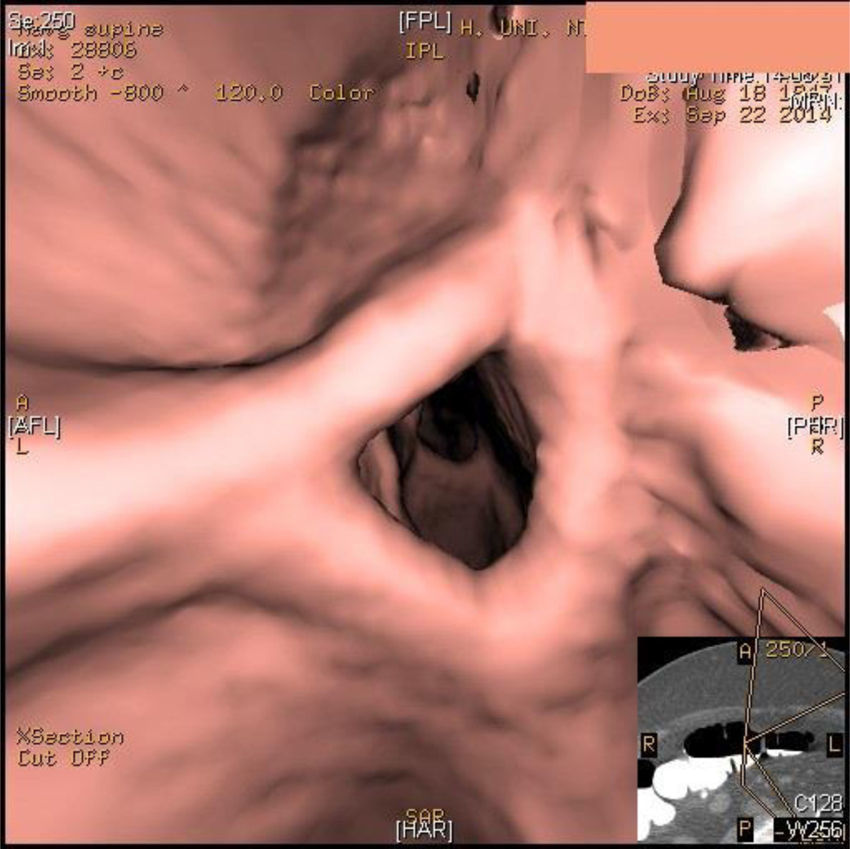
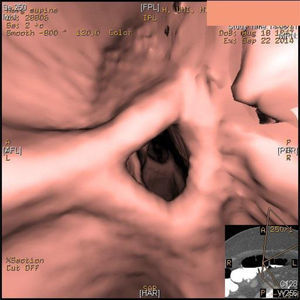
Given the suspicion of an underlying neoplastic process, a colonoscopy was performed, which demonstrated rigidity of the rectum/sigmoid colon 15cm from the anal margin, which impeded passage of the colonoscope. No neoplastic-appearing mucosal lesions were observed, so no colon biopsies were taken. A lower gastrointestinal series (Fig. 1) revealed stenosis of the sigmoid colon with no observed cause and absence of diverticula that could demonstrate chronic diverticular disease. Virtual colonoscopy (Fig. 2) showed the stenosis, which was probably inflammatory in origin.
Given the persistence of the subocclusive patient symptoms, we decided on surgery. During surgery, the lesion in the sigmoid colon was observed, which caused stenosis and was macroscopically suggestive of a tumor process with superficial implants. The remaining structures of the cavity appeared normal, so we conducted an oncological anterior resection of the upper rectum. Postoperative evolution was satisfactory, and the patient was asymptomatic at later follow-up evaluations. The histology study defined the lesion as endosalpingiosis occupying the entire muscular wall and the pericolic adipose tissue, with muscular layer hypertrophy and signs of fibrosis, but no signs of malignancy.
Endosalpingiosis is defined as the presence of Fallopian tube tissue in an ectopic location, unlike müllerianosis, which is the ectopic presence of at least 2 of the 3 components derived from Müllerian tissue (endometrium, Fallopian tube epithelium and endocervix).3 The pathogenesis is not clear, and there are currently 2 theories that attempt to clarify this anomaly: coelomic metaplasia,6 which is most widely accepted, and the theory of implantation (transplantation of the tubal mucosa to the peritoneal surface during surgical procedures or after inflammatory processes).2 In our case, the history of a previous hysterectomy could be the origin of the sigmoid endosalpingiosis based on the theory of implantation.
There are discrepancies regarding the clinical manifestations of endosalpingiosis. According to Prentice et al.,2 this entity appears more in postmenopausal women and presents less pelvic pain than patients with endometriosis or those without endosalpingiosis. However, there are studies that propose a greater association between endosalpingiosis and pelvic pain,3,7 although this usually coincides with endometriosis, which makes it difficult to identify the primary origin of pain.1 Our patient presented with prolonged pelvic pain, even after hysterectomy. The evidence between infertility and endosalpingiosis is currently not clear.2
Endosalpingiosis is a rare cause of large bowel obstruction, and few cases have been published in the literature. The longest series describes 4 cases that mimic neoplastic processes, one of which affected the colon, sigmoid colon and rectum.8 In our case, endosalpingiosis occupied the entire muscular wall and pericolic adipose tissue, with hypertrophy and fibrosis in the area, which caused the sigmoid stenosis and the patient's obstructive clinical symptoms.
The authors would like to thank the Coloproctology Division and the General Surgery and Gastrointestinal Surgery Departments at the Hospital Universitario Nuestra Señora de Candelaria for their support and collaboration in the preparation of this article.
Please cite this article as: Pérez Sánchez LE, Hernández Barroso M, Hernández Hernández G, Soto Sánchez A, Barrera Gómez MÁ. Endosalpingiosis como una entidad obstructiva simuladora de neoplasia de sigma. Cir Esp. 2017;95:172–173.