Lower limb varicose veins are often secondary to greater saphenous vein (GSV) insufficiency. Technological development has led to the appearance of new minimally invasive treatments, such as endovenous radiofrequency ablation (ERFA). This almost completely eliminates the disadvantages associated with conventional surgery (haematomas, scars, inguinal neovascularisation, and a prolonged time off work). Furthermore, it gives a better quality of life, less pain and inflammation than the endolaser. We review ERFA and present our results as a pioneering group in Spain. Between January 2006 and 2011 we have treated 153 limbs with a mean GSV diameter of 6.8mm (range 4.5–19). Tumescent anaesthesia was exclusively used in 71% of the procedures, and 98.5% without an inguinal surgical approach. Clinical and ultrasound follow-up with a prospective register was performed at 1 week, 3, 6, 12 months, and then annually.
ResultsThe occlusion rate of the treated vein was 97%, and there was a reflux rate of 6.6%. Inguinal neovascularisation was present on 0.7%. There was no neuritis, skin burns or deep vein thrombosis.
Las varices de las extremidades inferiores frecuentemente son secundarias a insuficiencia de la vena safena interna (VSI). El desarrollo tecnológico ha permitido la aparición de nuevos tratamientos mínimamente invasivos como la ablación por radiofrecuencia endovenosa (RFA). Esta elimina casi en su totalidad los inconvenientes asociados a la cirugía convencional (hematomas, cicatrices, neovascularización inguinal e incapacidad laboral prolongada). Además, confiere mejor calidad de vida, menor dolor e inflamación que el endoláser. Revisamos la RFA y presentamos nuestros resultados como grupo pionero en España. Entre enero de 2006 y 2011 hemos tratado 153 extremidades con un diámetro medio VSI 6,8mm (rango 4,5–19). El 71% de procedimientos fueron realizados exclusivamente bajo anestesia tumescente. El 98,5% sin abordaje quirúrgico inguinal. Seguimiento clínico y ecográfico con registro prospectivo 1.a semana, 3, 6, 12 meses, y anualmente.
ResultadosTasa de oclusión vena tratada 97%, tasa de reflujo 6,6%. Neovascularización inguinal 0,7%. No neuritis, quemadura cutánea, ni trombosis venosa profunda.
Chronic venous insufficiency is highly prevalent in Western society. Lower limb varicose veins are the most frequent vascular disease in humans, affecting 20%–25% of women and 10%–15% of men.1,2 Michaels et al. recently published a randomised controlled study showing that surgical treatment of uncomplicated symptomatic varicose veins was cost-effective.3
Considering the pathophysiology of chronic venous insufficiency, it is clear that in order to achieve effective and lasting results in treating varicose veins, we must eliminate the venous reflux.4,5 Information on venous haemodynamics from studies using Doppler ultrasound show that lower limb varicose veins are mostly (70% of cases) due to arch and/or truncal insufficiency of the great saphenous vein (GSV). Less frequently, other systems can be affected such as the external saphenous vein and perforating and/or tributary veins.6,7 Thus, the elimination of saphenous vein reflux has been clearly established for years as the Achilles heel of varicose vein treatment, and must therefore be considered the first therapeutic objective.4 With this, we eliminate the primary haemodynamic mechanism involved in the development and progression of varicose veins: venous hypertension caused by the hydrostatic pressure column.
Until recently, the only effective and lasting surgical treatment for truncal varicose veins was ligation of the saphenous-femoral arch and stripping of the GSV. Over the latest decade, technological progress has enabled the development and application of new minimally invasive therapies such as VNUS Closure endovenous radiofrequency ablation (RFA) and endolaser.
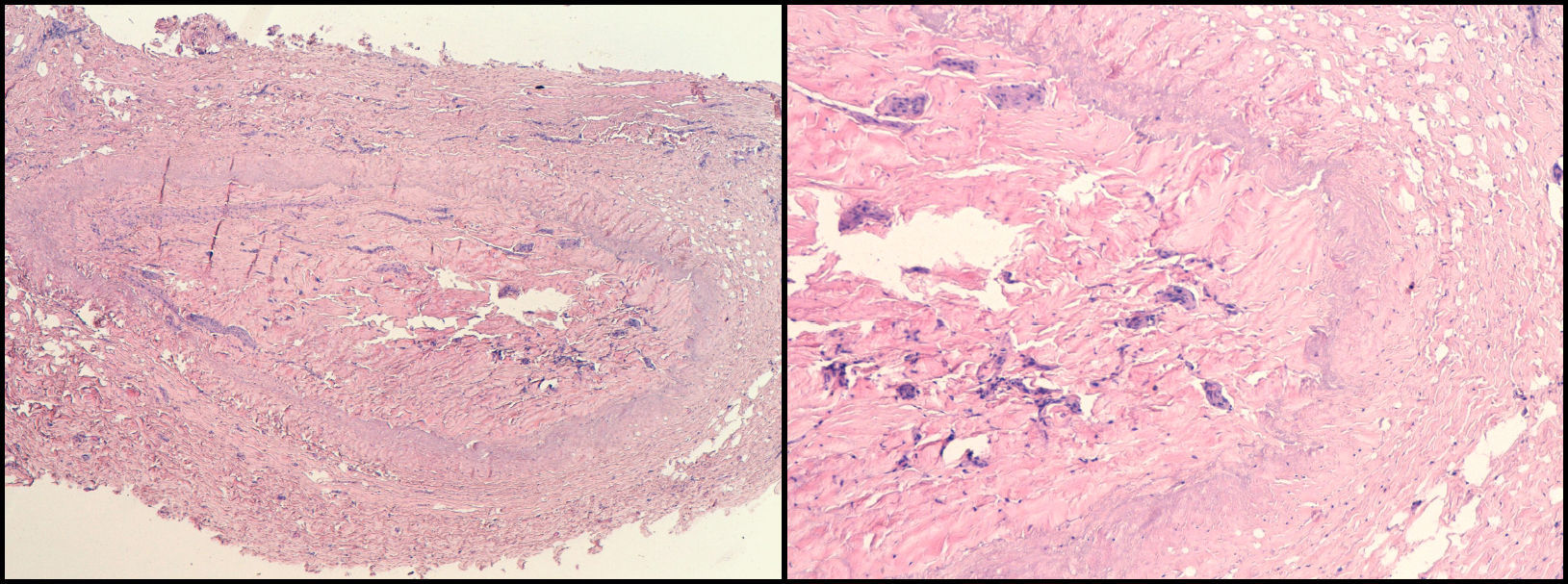
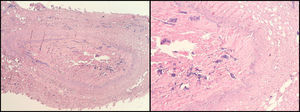
Mechanism of ActionRadiofrequency (RF) is electromagnetic energy and thus non-ionising. It is composed of electric and magnetic waves that, when in contact with tissue, cause vibration and friction of their atoms, transforming into thermal energy (ohmic or resistive heat). The increased temperature generated by RF causes a series of changes to the structure of the treated vein. Among other changes, we know that the unwinding of the collagen triple helix starts above 60°C and its molecular contractile force increases to a greater extent. However, it is very important to avoid very high temperatures so as not to cause boiling, vaporisation and carbonisation of tissue, which occurs with other energy sources such as endolaser, generating peaks of 700–1500°C.8,9 The temperature range used with RF is clearly lower (95–120°C), sufficient for inducing the following macroscopic and microscopic changes to the venous wall: (a) endothelial destruction, (b) collagen denaturation and contraction, (c) shortening and thickening of the venous wall and (d) reduction of vessel lumen. Thus, the therapeutic objective of RFA is to induce fibrotic occlusion of the treated vein and its subsequent disappearance by atrophy (Fig. 1).8,10
A little over a decade ago, development began on the VNUS Closure® endovenous radiofrequency ablation system (VNUS Medical Technologies, San Jose, CA, USA), consisting of an RF generator and a fine bipolar percutaneous catheter that is inserted and guided through the affected vein. It was first applied to clinical practice in 1998, receiving approval from the Food and Drug Administration (FDA) in 1999. In recent years, its use has been increasingly spreading throughout most of the developed world. In addition, its indications have been expanded to venous segments other than the GSV, such as the anterior saphenous vein, the external saphenous vein and the perforating veins.11
Clinical Experience and Scientific EvidenceStarting in 2000, various clinical and experimental studies were published demonstrating RFA to be safe and effective in eliminating saphenous vein reflux.12–14 One of the most important was the multicentre study published by Merchant et al.,15,16 with 1222 limbs treated and a follow-up of four years. It showed ultrasound success and patient satisfaction in more than 85% of cases.
Radiofrequency Versus StrippingOf still greater importance was the information from the publication of four prospective randomised studies comparing the gold standard of conventional surgery (femoral saphenous arch ligation and GSV stripping).17–20 The results of these studies were consistent: RFA had the same efficacy as conventional surgery, but was clearly superior in reducing postoperative pain, and provided better quality of life and a faster recovery.
The results are described in detail below. The Rautio et al. study17,21 showed less pain (visual analogue scale) at rest (P=.017), standing (P=.026) and walking (P=.036). The most significant differences were between day 5 and day 14 after surgery. The need for analgesics in the RFA group was 0.4±0.49 tablets of ibuprofen per day, compared to 1.3±1.09 tablets for the stripping group (P<.004). The time to returning to work was also clearly lower, 6.5±3.3 days for the RFA group, compared to 15.6±6.0 days for the stripping group (P<.001). Physical recovery was also much faster for the RFA group (RAND-35 quality of life questionnaire). These patients were monitored for three years and there were no differences in the recurrence of varicose veins.18 The Endovenous Obliteration vs Ligation and Vein Stripping study (EVOLVeS)19,20 was a multicentre prospective randomised study comparing conventional surgery and assessing the long-term results and efficacy of the procedure. Eighty limbs underwent surgery: 44 with RFA and 36 with stripping. During early follow-up (four months), complications, recovery time and quality of life variables were compared. The most significant differences between the groups were recovery time after surgery, with a return to normal activities time of 1.15 days for RFA versus 3.89 days for the stripping group (P=.02), and a return to work time of 4.7 days for RFA compared to 12.4 days for the stripping group (P<.05). The stripping group had greater morbidity at three weeks, especially haematomas, ecchymosis and pain. Improvement in the venous clinical severity score (VCSS) was also favourable for the RFA group at 72h and at one week. These differences went away over time, as was to be expected. The quality of life assessment (CIVIQ2) was clearly better for the RFA group, with noteworthy differences in overall and pain scale scores.
The impact on clinical and haemodynamic results was once again compared in this patient sample at one year and at two years. The RFA group achieved better quality of life scores at one and two years (P<.001). Both treatments were shown to be equally effective, with no differences at the clinical (symptoms, signs and recurrence of varicose veins) or haemodynamic levels measured using Doppler ultrasound (absence of reflux: 91.7% for the RFA vs 89.7% in the stripping group). Using RFA, 41% of saphenous veins were undetectable at the two-year follow-up study. The rate of recurrence was lower for the RF group (14% vs 21%), although this was not statistically significant. The situation with neovascularisation was similar, being lower for the RFA group (2.8%) than for the stripping group (13.8%).
Stotter et al.22 published a randomised prospective study in 2005, which compared three techniques: VNUS Closure (n=20), stripping (n=20) and cryostripping (n=20). After six weeks of follow-up, the RFA group achieved better quality of life scores (CIVIQ-2) (P=.012). It was also shown to be the least painful technique (P=.014). Time to returning to work for the RFA group (7 days) was also favourable when compared to the stripping group (14 days) and the cryostripping group (12 days) (P=.007).
Hinchcliffe et al.23 compared RFA (n=16) to conventional surgery (n=16) in the treatment of bilateral, recurrent varicose great saphenous veins. The results demonstrated the superiority of RFA for the majority of studied variables: shorter surgical time (25.5min vs 40min, P=.02), less pain in the visual analogue scale (1.7 vs 3.8, P=.02), less ecchymosis assessed by digital imaging analysis (11.9 vs 21.8, P=.02) and a more rapid return to work.
Radiofrequency Versus EndolaserFrom the technical and technological standpoint, there are significant differences between them that have been shown at the experimental level in two studies by Schmedt et al.8,10 whose results are consistent with those of Weiss.14 We can conclude therefore that RFA shows a circular, homogeneous lesion without perforation of the venous wall or carbonisation.
From the clinical point of view, five studies have been published comparing RFA and endolaser; the first two with ClosurePLUS,24,25 two others with ClosureFAST26–28 and one with Celon RFITT (Olympus, Germany).29 The first, published by Puggioni in 2005,25 treated 77 patients with EVL and 53 with RFA consecutively. Overall technical success at one month was 93.9% (100% for EVL and 96% for RFA). When assessing the results of this study, we need to take into account a significant scientific design bias since follow-up Doppler ultrasound was performed on only 50% of patients. A greater number of complications were reported for EVL, 20.8% compared to 7.6% for RFA (P=.049). Some 2.3% of patients (3 of the 77) treated with EVL showed protrusion of the thrombus into the common femoral vein.
In 2006, Almeida24 reported a greater number of cases (819 EVL and 128 RF) and a longer follow-up (1.5 years). The recanalisation rate was somewhat greater for RFA, 5.5% versus 1.7% for EVL. The rate of extension of the thrombus into the common femoral vein was 0.2% for EVL and absent for RFA.
Gale et al.26 recently published another prospective randomised study comparing RFA ClosurePlus (obsolete) (n=46) and EVL (810nm) (n=48), reporting results at one month and at one year. Both methods were very effective in reducing symptoms (VCSS, CEAP, CIVIQ-2). RFA showed a higher rate of late recanalisation (11 for RFA and 2 for EVL, P=.002). Therefore, EVL was more effective than ClosurePlus but in exchange for a higher rate of ecchymosis and discomfort during the perioperative period.
In 2009, Almeida et al.27 published the RECOVERY study, a multicentre randomised comparative study of 87 veins in 69 patients. The groups were EVL (980nm) (n=41) and RFA ClosureFAST (n=46), with a one-month follow-up. The primary objectives were postoperative pain, ecchymosis, swelling and complications from the procedure. The secondary objectives were the venous clinical severity score and quality of life score (VCSS and QOL scores). The study concluded that: (1) RFA is significantly superior to EVL in terms of post-operative recovery and quality of life parameters and, (2) complications were significantly more prevalent in the EVL group (22.0% vs 4.4%, P=.02).
In 2010, Shepherd et al.28 published another comparative study on 131 patients using RFA ClosureFAST (n=67) and EVL (980nm) (n=64). They analysed postoperative pain and quality of life at six weeks (AVVQ, VCSS and SF12). The study showed less pain in patients undergoing RFA for the first 10 days (P=.001). Furthermore, both groups had improved quality of life after the intervention (AVVQ, VCSS and SF12) with no statistically significant differences between the two methods. The return both to daily activities and the workplace was similar for both groups, with an overall rate of return to work within the first week of 70%. In another study by the same author,29 patients with RFA returned to work sooner than those treated with EVL (5 days vs 9 days, P=.022).
The LARA study30 compared the Celon RFITT RF system (Olympus Surgical Technologies, Germany) to EVL (810nm). They treated 87 limbs in a study designed to assess the differences in short-term pain and swelling. The results were comparable to the studies described above, although it analysed separately unilateral and bilateral procedures.
In summary, with the data currently available, we can conclude that RFA achieves similar results to EVL, although with clearly less pain, ecchymosis and haematomas, as well as providing better short-term quality of life.
Radiofrequency EquipmentEndovenous radiofrequency ablation requires a generator and a bipolar catheter. Two types of catheters have been primarily used in recent years: Plus® and FAST™. The characteristics of each are listed below.
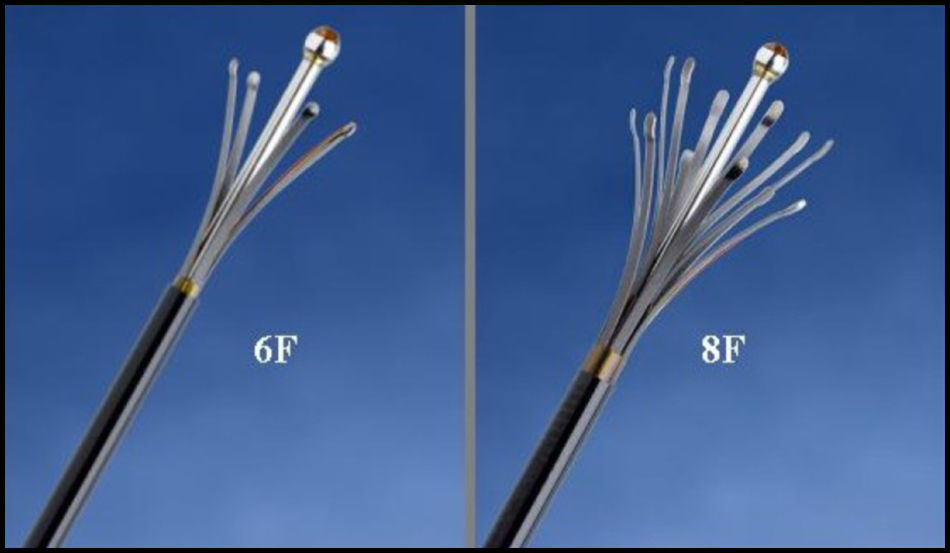
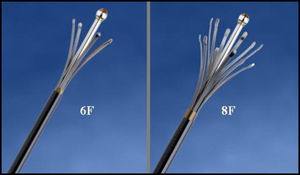
ClosurePlus CatheterThe Plus model catheter (Fig. 2) is equipped with a therapeutic tip consisting of a collapsible bipolar electrode whose opening and closing are controlled by the surgeon from the handle. In addition, it has a temperature sensor on that tip, which transmits information to the generator concerning various treatment parameters (temperature, impedance and power). The opening of the catheter allows for the transmission of RF energy from the electrodes and through the venous wall, which is known as resistive heating, that is, heat is not generated at the catheter tip but in the vein wall. Treatment temperature is 85–90°C and the catheter must be removed slowly at a constant speed of 2.5–3cm/min. The central lumen of the catheter requires continuous flushing with heparinised saline solution to minimise clotting on the tip. It allows for the passage of a 0.025in. guide through its interior in order to facilitate its movement towards the saphenous-femoral arch in winding veins. There are two catheters depending on the size of the vein: 5F (1.7mm) for veins up to 8mm in diameter and 8F, which is recommended for veins up to 12mm (Fig. 2). Despite the positive clinical results reported with the Plus system, the procedure has a number of disadvantages, mainly the slowness, and a certain degree of variability in the speed of ablation. It was also frequently necessary to extract the catheter during the procedure so as to clean the clot that formed on the electrodes.
ClosureFAST™ Catheter and RFGPlus™ Generator Model RFG2Various experimental and clinical research studies31,32 with different designs have led to the development of the new FAST catheter, which has improved the efficacy and reduced the time of ablation considerably. It won FDA approval in August 2006 and has been marketed since the first quarter of 2007. We performed the first treatment in Spain in May of the same year with the collaboration of Dr Merchant (Reno, Nevada, USA).
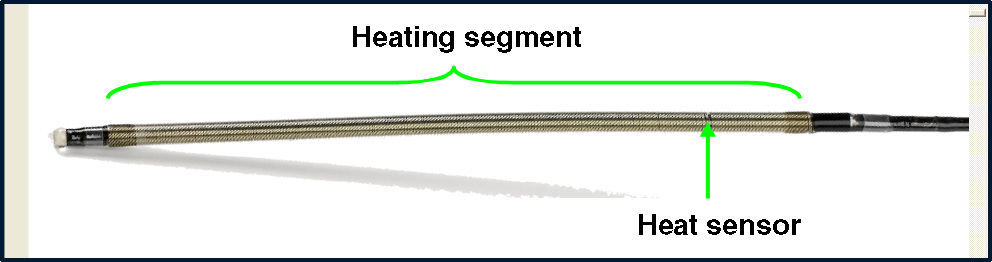
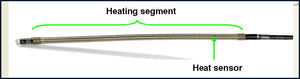
This next-generation catheter has a 7-cm long therapeutic segment on the tip and a lubricious jacket to facilitate guidance and minimise clotting on the heating segment (Fig. 3). It is a very accurate temperature control system regulated by a feedback mechanism thanks to a temperature sensor near the catheter tip. The RFG2 generator (Fig. 4) is designed for automatic adjustment, so as to provide the minimum power necessary (range 15–40W) for reaching and maintaining 120°C during 20-s cycles. It thus provides transmural heating of the venous wall while limiting the heating up of the surrounding tissue.32
The catheter has white spacing markers every 6.5cm, which indicate the pullback distance for each treatment cycle. Pullback during ablation is segmental, unlike ClosurePlus, which was continuous and therefore subject to variability. The section of vein closest to the saphenous-femoral junction requires two treatment cycles according to a well-established protocol. Like ClosurePlus, it allows for the use of a 0.025in. guide, which facilitates movement of the catheter through winding veins.
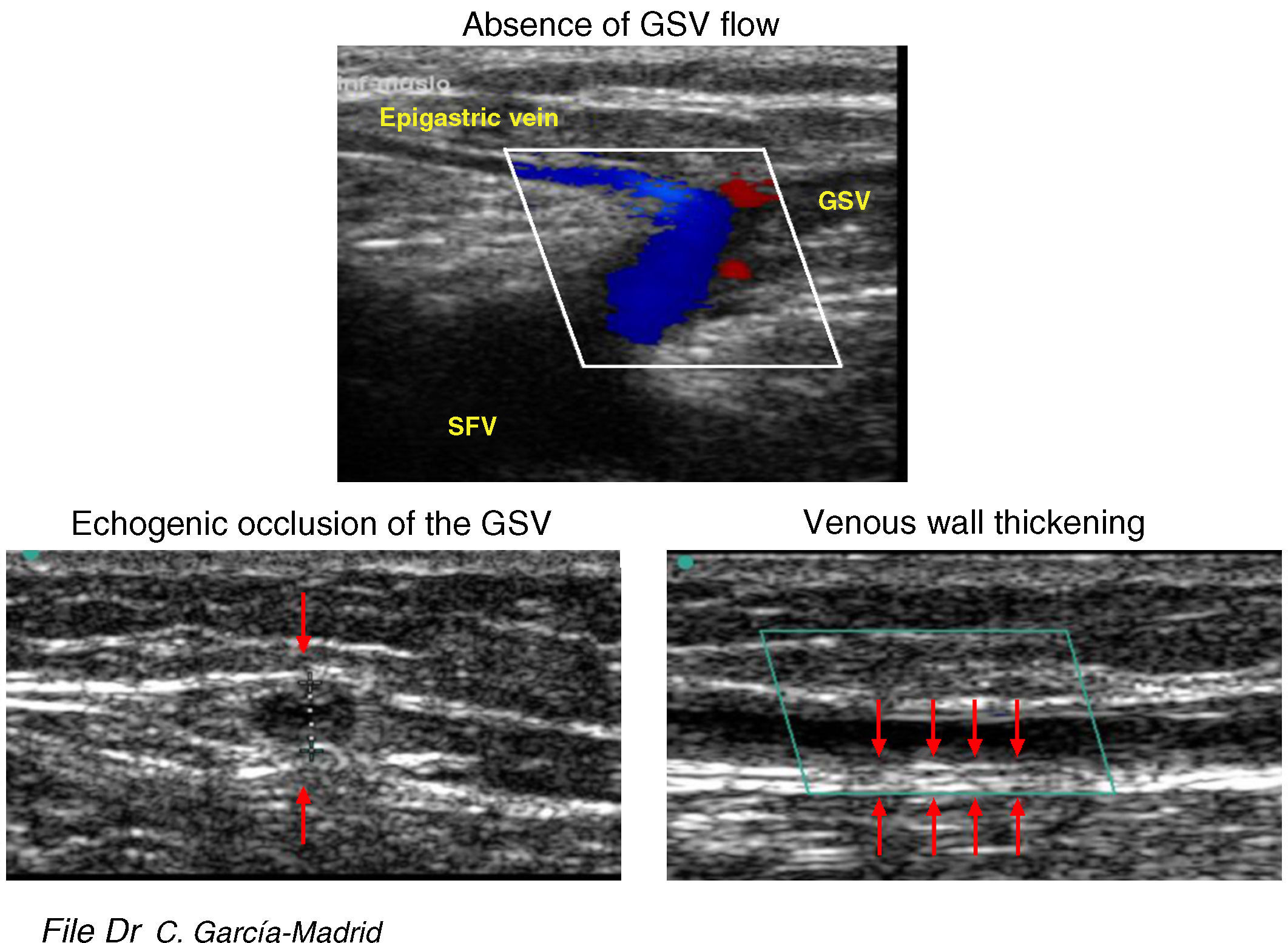
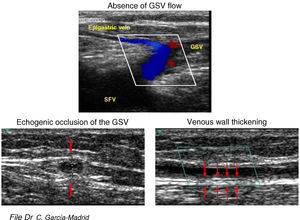
ProcedureThis is a completely ultrasound-assisted procedure. Marking should be performed before the operation using Doppler ultrasound, from groin to ankle, highlighting winding sections, ectasia areas, incompetent perforating veins and varicose packages. The procedure absolutely requires the use of tumescent local anaesthesia, that is, through an ultrasound-guided injection of Klein's Solution (lidocaine, adrenaline, bicarbonate and saline solution) at the perivenous level (in the split of the superficial aponeurosis). Tumescent anaesthesia has a threefold purpose: (1) analgesia, (2) protection for the skin and surrounding structures against heat and, (3) promotion of vein collapse. Access to the GSV varies and may be surgical through a mini-incision or percutaneous (Fig. 5). The latter is performed using the Seldinger technique. To prevent recurrence, it is essential to occlude birth of collateral veins with retrograde flow. Therefore, the tip of the catheter should be placed near the epigastric vein and never more than 2cm from the saphenous-femoral junction. During energy emission, applying external pressure on the heating segment and placing the patient in the Trendelemburg position is recommended. After completing the procedure, the treated segment should be monitored by ultrasound, as well as the correct permeability of the common femoral vein (Fig. 6). Despite its low frequency, thrombotic complication must be ruled out by monitoring via Doppler ultrasound during the first post-operative days.
First-Hand ExperienceIn our institute we implemented the programa de tratamiento mínimamente invasivo de las varices mediante radiofrecuencia endovenosa (minimally invasive treatment programme for varicose veins using endovenous radiofrequency) in January 2006. Previously, in 2005, we started theoretical training in the new VNUS Closure technique and participated in training visits in two of the most experienced centres worldwide, run by Dr Merchant (Reno Vein Clinic, Reno, Nevada, USA) and Dr Whiteley (Whiteley Clinic, Guilford, England).
From January 2006 to 2011, we treated 153 limbs in 125 patients (111 women) in CEAP clinical class 2–6 with varicose veins secondary to GSV reflux. The mean age was 57 years (range 18–84) and mean GSV diameter was 6.8mm (range 4.5–19). All data was collected prospectively. We used the ClosurePlus catheter in the first 40 cases and the new ClosureFAST catheter in the last 113 cases. Seventy-one percent of procedures were performed exclusively under tumescent anaesthesia, with immediate return to normal activity. Regional anaesthesia was provided for patients (29%) with extensive varicose veins or for bilateral procedures in a single operation. An inguinal surgical approach was not performed in 97.4% of cases (151 of 153 cases). Technical and immediate clinical success was 100%. Mean ablation time was clearly lower for the FAST catheter compared to the Plus one (2.5min vs 14min). Mean length of the treated veins was 32±8cm. None of the patients suffered burns, neuritis or deep vein thrombosis. Heat-induced thrombosis, i.e. the presence of thrombus in the saphenous-femoral junction, was detected in four patients. This is a benign condition associated with thermal ablation techniques. Clinical and ultrasound follow-up was performed on our patients during the first week and at one month, three months, six months, one year and annually. The results show a 97% rate of sustained occlusion of the treated vein, a reflux rate of 6.6% and inguinal neovascularisation of 0.7%.
Therefore, thermal ablation of GSV with the VNUS Closure system is a highly effective and lasting procedure. The next-generation catheter has enabled us to reduce ablation time to 2–3min and has greatly simplified the procedure. The ability to perform the procedure under tumescent local anaesthesia allows for an immediate return to daily activities with optimal medical and cosmetic results, as well as high patient satisfaction. Despite the fact that the optimal approach to varicose veins is complex and always requires individualised treatment, we believe that radiofrequency ablation of GSV is the first choice among therapeutic options.
ConclusionThe introduction of new minimally invasive endovenous treatments in the 21st Century has greatly stimulated interest in venous ailments. Today, the VNUS Closure endovenous radiofrequency ablation is a safe and highly effective technique for the treatment of varicose veins with high patient satisfaction, early return to normal activity and almost complete absence of pain. It has demonstrated its superiority over conventional surgery with level 1 scientific evidence17–21 (level 1 recommendation, level of evidence A, Guidelines 4,9.0 of the American Venous Forum). Additionally, since it is painless and offers better quality of life versus the endolaser, it may now be considered one of the first lines of treatment for patients affected by varicose veins.
Complications are very rare (vein thrombosis, skin burns and neuritis), but in order to prevent them appropriate training in developing the various technical skills is needed. These skills include infiltration of tumescent anaesthesia, percutaneous vein approach and catheterisation, and especially strong familiarity with the use of Doppler ultrasound. The latter is fundamental and essential for planning the optimal strategy, appropriate control of all steps of the procedure and, last but not least, the proper follow-up of patients.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: García-Madrid C, et al. Nuevos avances en el tratamiento de las varices: radiofrecuencia endovenosa VNUS Closure®. Cir Esp. 2011;89:420–6.