There has been an alarming worldwide increase of obese people in recent years. Currently, there is no consensus on whether patients that are scheduled to undergo bariatric surgery should lose weight before the intervention. The objective of this research is to analyse the influence of pre-surgery loss of weight in the nutritional parameters of patients.
MethodsFifty patients that were scheduled to undergo bariatric surgery followed a very low caloric diet during 4 weeks prior to the surgery. The nutritional parameters were analysed at 3 specific moments: before starting the diet, at the moment of surgery (when the diet was concluded) and one month after the surgery.
ResultsAverage values for haemoglobin, albumin and lymphocytes were kept within the range of normal values at all moments, even though the decrease of those parameters was statistically significant throughout the study (P<.05). By following the very low caloric diet, less than 9.5% of the sample suffered anaemia.
ConclusionsLoss of weight prior to surgery does not have a significant influence in the nutritional parameters of the patient. These results would support the indication of losing weight for patients that are considered candidates for bariatric surgery.
El número de personas obesas ha aumentado de forma alarmante en todo el mundo. Actualmente no existe un consenso acerca de si los pacientes que van a ser sometidos a una cirugía bariátrica deben o no perder peso antes de la misma. El objeto de la presente investigación es analizar la influencia de la pérdida de peso preoperatoria en los parámetros nutricionales de los pacientes.
MétodosSe sometió a 50 pacientes que iban a ser intervenidos de una cirugía bariátrica a una dieta de muy bajo contenido calórico durante las 4 semanas previas a la intervención. Se analizaron los parámetros nutricionales en 3 momentos específicos: antes de empezar la dieta, en el momento de la intervención (al finalizar la dieta) y un mes después.
ResultadosLa media de hemoglobina, albúmina y linfocitos se mantuvo dentro del rango de la normalidad en todo momento a pesar de que los descensos de dichos parámetros fueron estadísticamente significativos a lo largo del estudio (p<0,05). Con la dieta de muy bajo contenido calórico se anemizó menos del 9,5% de la muestra.
ConclusionesLa pérdida de peso preoperatoria no influye de manera significativa en los parámetros nutricionales analizados. Estos resultados apoyarían la indicación de una pérdida de peso preoperatoria en los pacientes candidatos a cirugía bariátrica.
Bariatric surgery is the most effective treatment to bring about and maintain long-term weight loss in the majority of patients with morbid obesity, as well as to resolve their comorbidities.1
As these patients have a large number of associated pathologies and high surgical risk, it is highly important to optimise their condition before surgery.
With the aim of achieving an uncomplicated surgery and postoperative period, it is increasingly recommended that patients lose weight before the operation, to improve their general condition and to prevent aggravation of their underlying disease.
Although this preoperative weight loss has been shown to be effective in improving certain conditions, such as fatty liver disease, reducing intra-abdominal fat and facilitating surgery,2 no study has been performed of whether this weight loss may lead to the malnutrition of these patients.
The aim of this study is to analyse the influence of preoperative weight loss on the nutritional parameters of candidate patients for bariatric surgery.
MethodsAn observational prospective study was designed to analyse whether preoperative weight loss using a very low calorie diet (VLCD) during the 4 weeks prior to bariatric surgery led to a significant alteration in nutritional parameters. This study took place in the period from 1 January 2012 to 31 October 2012.
The Optifast® range of products was used for the VLCD. Optifast® is a complete diet, given that it supplies the organism with all essential nutrients. Each sachet supplies 17.5g of protein, 201 calories and a third of the daily requirement for vitamins and minerals. The proteins are of high biological value, and each sachet of Optifast® also supplies 3.6g of prebiotic fibre (inulin) which aids intestinal transit. This is why the patients in the study exclusively consumed 3 shakes of Optifast®/day, supplemented with low calorie liquids such as water, defatted stock or infusions.
The subjects in the study were patients with a BMI>35kg/m2 and associated comorbidity or a BMI>40kg/m2. They were aged from 18 to 60 years old and were candidates for bariatric surgery using a Roux-En-Y laparoscopic gastric bypass, according to the current protocol in the Multidisciplinary Bariatric Surgery Unit of the Hospital Universitario General, Castellón. Each patient was asked to express their acceptance and sign the corresponding informed consent form. The study design was approved by the Clinical Research Commission of the hospital.
The general lineal model formerly known as ANOVA for repeated measurements was used to calculate the size of the sample. This model is useful for studying several intra- and inter-subject factors.
A total of 50 patients were operated on according to this protocol during the period of time analysed. Of these 50 patients, monitoring was not optimum in 8 cases, so that these were finally excluded. A total of 42 patients were therefore included in the study. Of these 42 patients, 13 were men and 29 were women. They were aged from 22 to 61 years old, with an average age of 43.88 years old and a median age of 48 years. The average age of the men was 44, while for the women it was 45. During diet monitoring the patients were only evaluated at the start and end of the same, to check whether they had followed it and were suitable candidates for surgery. No side effects of the diet were recorded.
Statistical analysisStatistical was based on variance analysis for variables repeated at 3 different moments. The average and standard deviation were the main descriptive statistical tools used, while the median, simple range (minimum and maximum values) and the interquartile range (quartile 25 and quartile 75) were also calculated. A box plot graph was added. The general lineal model for repeated measurements was used for inferential analysis.
The differences obtained were considered to be statistically significant when P<.05.
The statistical computer programme SPSS version 15.0 for Windows was used for data analysis.
Nutritional parameters were considered to be altered when figures were below the values that are deemed normal in the laboratory of our hospital. In the case of haemoglobin, when this was below 12g/dL, for albumin when the figure was below 4g/dL, and for lymphocytes when the value was below 900μL.
The postoperative complications which arose were one hemoperitoneum, 2 minor digestive haemorrhages, one haemorrhage of the gastrojejunal anastomosis and a postoperative seroma. All of these were resolved without incident.
ResultsDuring the period of time studied a total of 50 patients were operated on according to this protocol. Of these 50 patients, 8 did not attend the stipulated check-ups. Given that they were not followed up in an optimum way, they were excluded from the study. A total of 42 patients were therefore included in the study, and the calculations shown below refer to a value n of 42.
Of the 42 patients studied, 13 were men and 29 were women. They were aged from 22 to 61 years old, with an average age of 43.88 years old and a median age of 48 years. The average age of the men was 44 years old, while for the women it was 45 years old.
WeightIn the month before the operation, patient weights varied from a maximum of 215.8kg and a minimum of 92kg, with an average of 129.8kg, a median figure of 123.8kg and a standard deviation of 26kg. At the time of surgery these weights had fallen to a maximum of 197.2kg, a minimum of 84kg, an average of 118.7kg, and a median of 114.4kg, with a standard deviation of 23kg. In the month after surgery the maximum weight was 158kg, the minimum was 75kg, the average was 106.5kg, the median was 103.8kg and the standard deviation was 18.5kg.
The average fall in weight during the month of VLCD was from 129.8kg to 118.7kg (−11.1kg; 8.6%), while in the month following surgery it was from 118.7kg to 106.5kg (−12.2kg; 10.3%).
The evolution of the average weight in the different periods analysed shows a statistically significant fall (P<.001) during the whole time the study lasted.
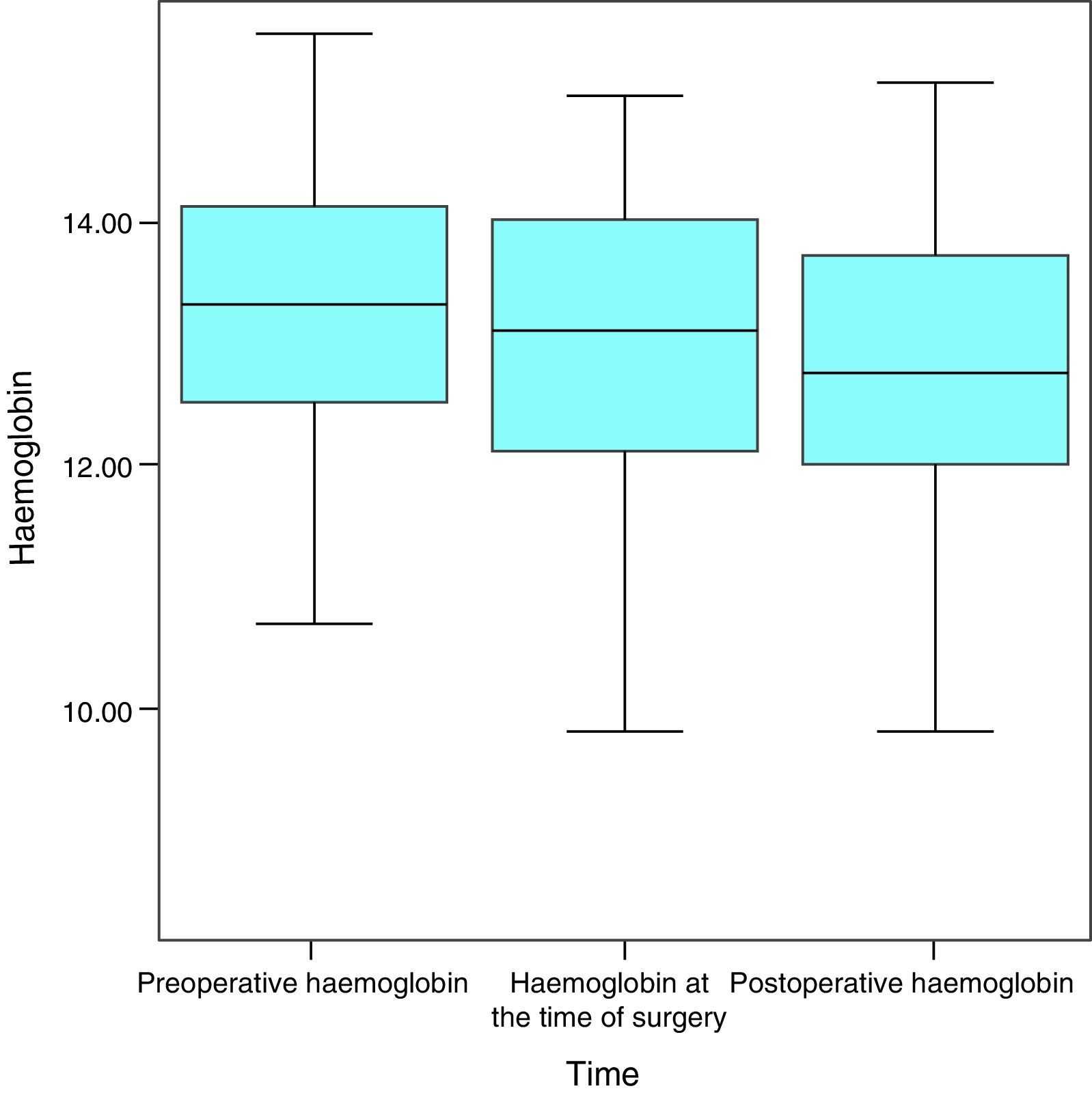
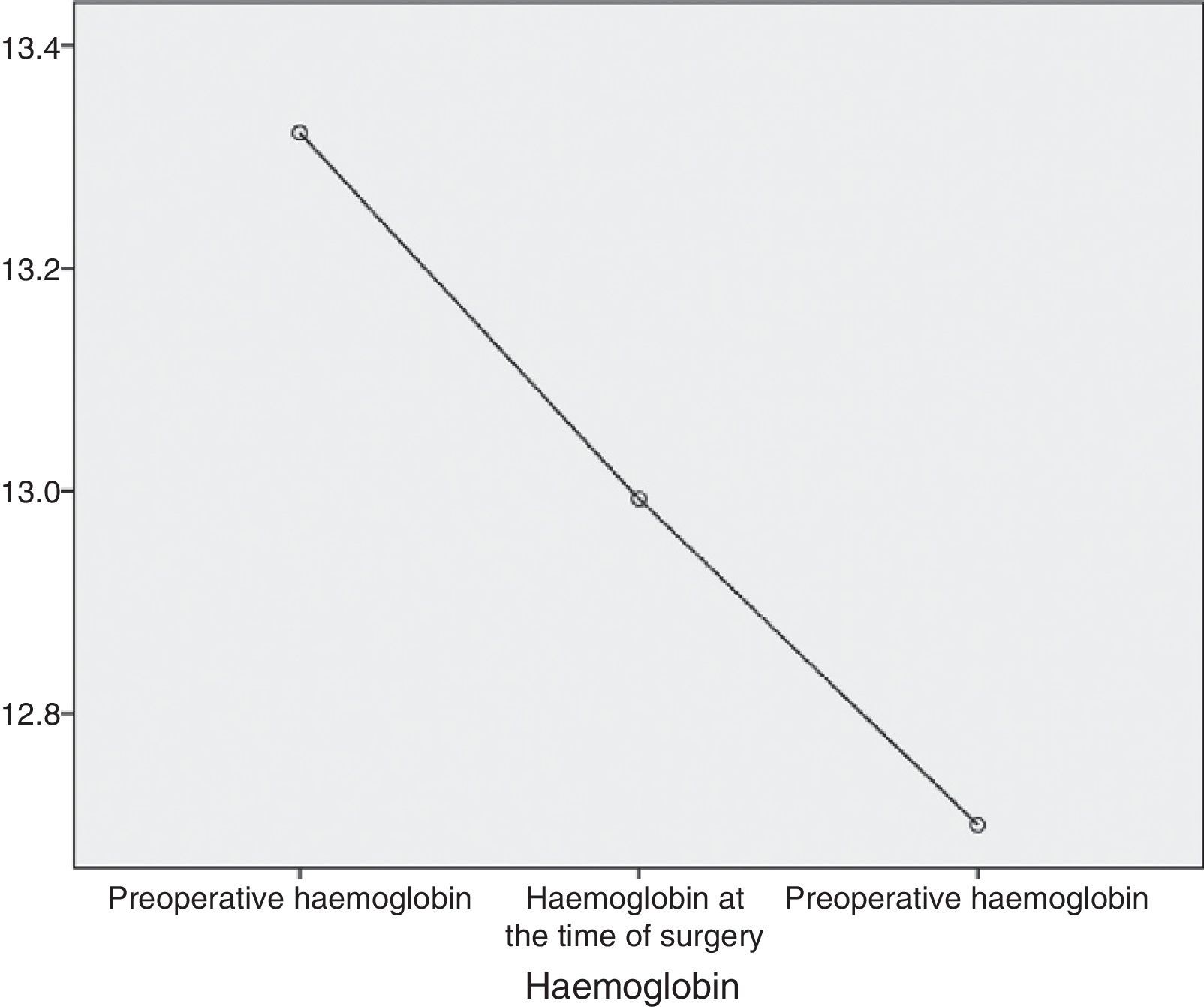
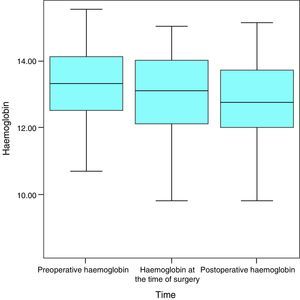
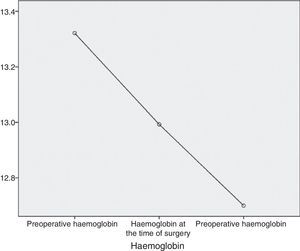
HaemoglobinAt the start of the study, this averaged 13.3g/dL, a median value of 13.3g/dL and a standard deviation of 1.2g/dL, with a maximum figure of 15.5g/dL and a minimum of 10.7g/dL. At the time of surgery and after the VLCD, the average was 13g/dL (a variation of −0.3mg/dL; 2.3%), the median figure was 13.1g/dL and the standard deviation was 1.4g/dL, with a maximum figure of 15g/dL and a minimum figure of 8.4g/dL. One month after surgery, the figures for haemoglobin were an average of 12.7g/dL (variation of −0.3mg/dL; 2.3%), a median figure of 13.1g/dL and a standard deviation of 1.4g/dL, with a maximum of 15.1g/dL and a minimum of 9.8g/dL (Fig. 1).
As normal figures for haemoglobin are from 12 to 18g/dL, it can be seen that the average remained within the normal range throughout the study.
With the VLCD 9.5% of the sample became anaemic (4 patients) and this occurred with surgery in 4.76% of the patients (2 patients).
When all of the patients are considered, haemoglobin levels displayed a statistically significant fall over the successive measurements (P=.006) (Fig. 2).
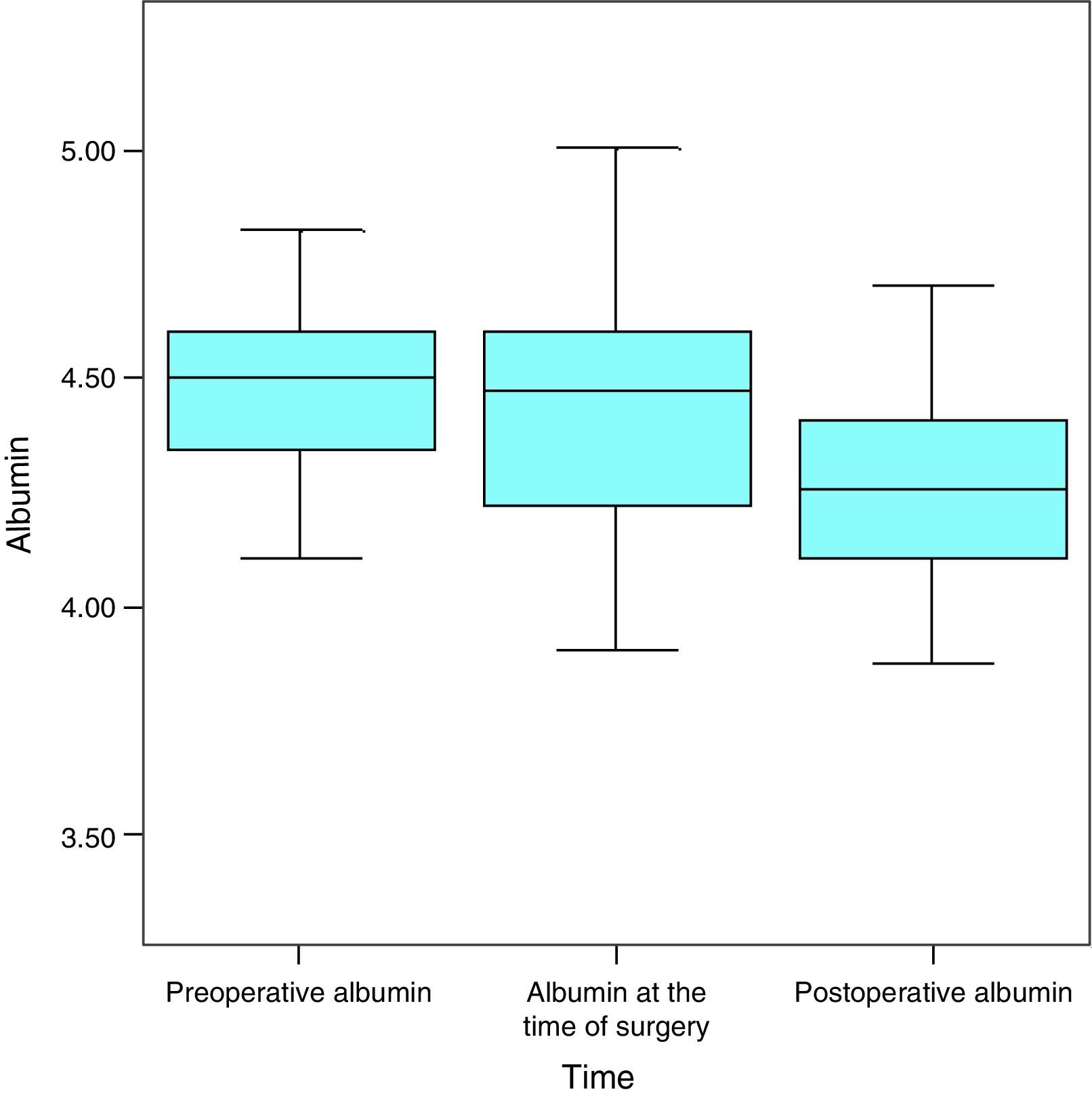
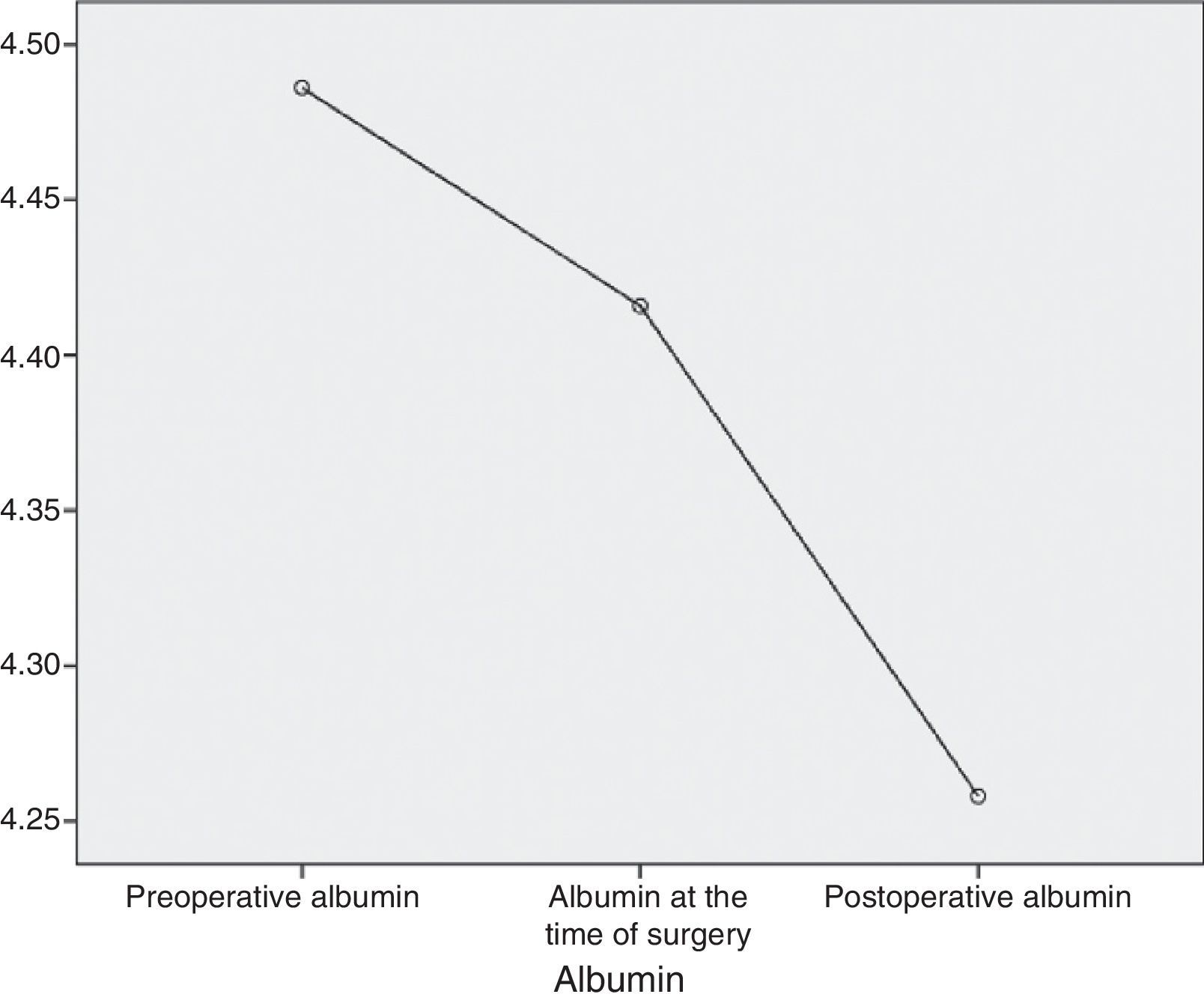
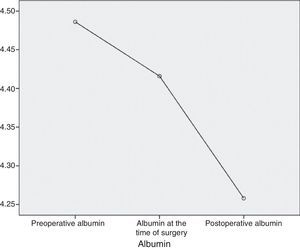
AlbuminAt the start of the study the average level of albumin in the patients was 4.5g/dL, the median level was 4.5g/dL and standard deviation was 0.2g/dL, with a maximum figure of 5g/dL and a minimum of 4.1g/dL. One month later, the average was 4.4g/dL (a variation of −0.1mg/dL; 2.2%), the median was 4.5g/dL and the standard deviation was 0.4g/dL with a maximum figure of 5.2g/dL and a minimum figure of 4.1g/dL. In the month after the operation the average albumin level was 4.3g/dL (a variation of −0.1mg/dL; 2.3%), the median level was 4.3g/dL, with a standard deviation of 0.3g/dL, a maximum of 4.9g/dL and a minimum of 3.4g/dL (Fig. 3).
With the VLCD there 9.5% of the sample had an albumin deficit (4 patients) while after surgery this occurred in 2.38% of the patients (one patient).
Considering the whole sample, albumin fell in a statistically significant degree throughout the successive measurements (P<.001) (Fig. 4).
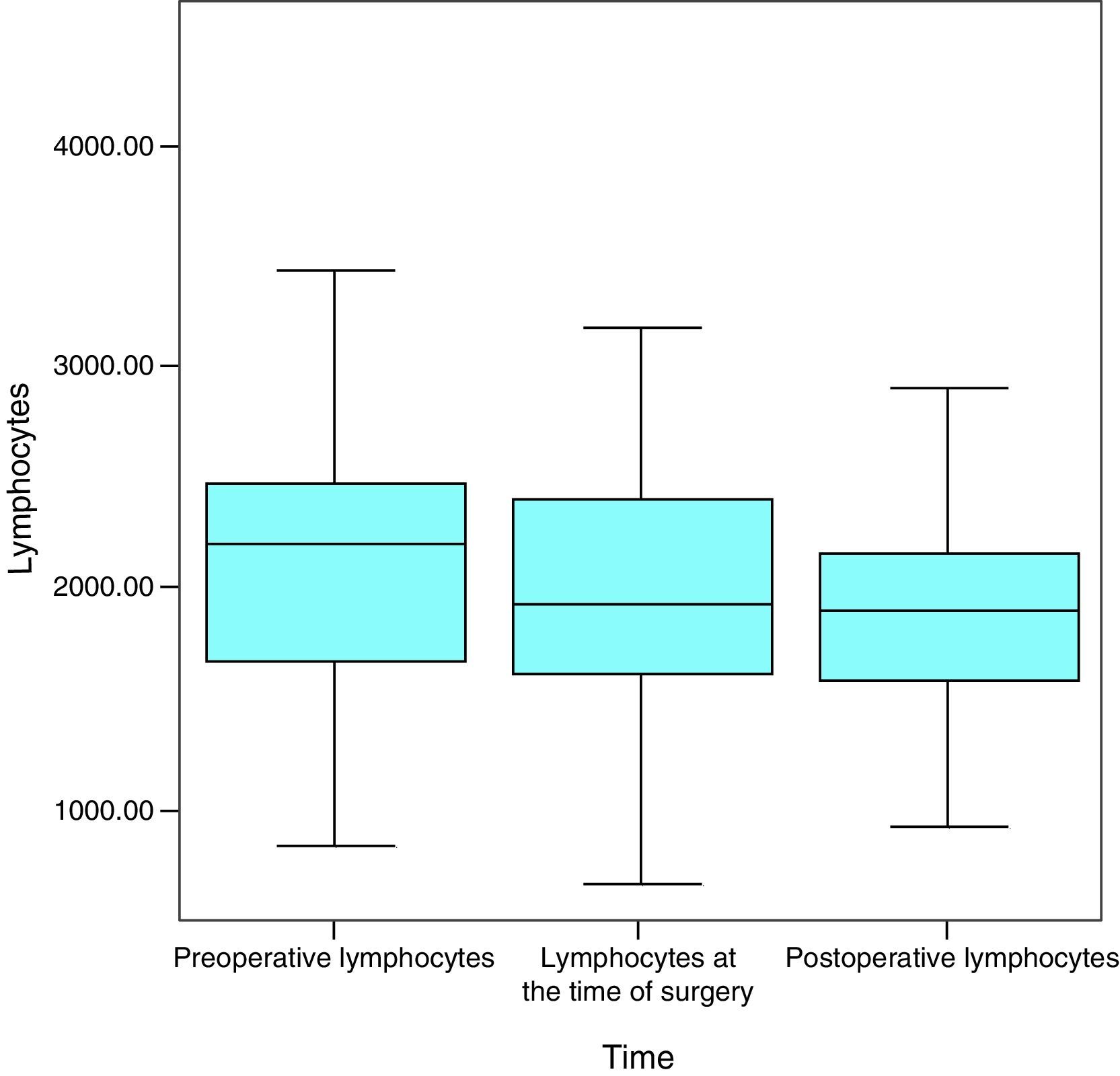
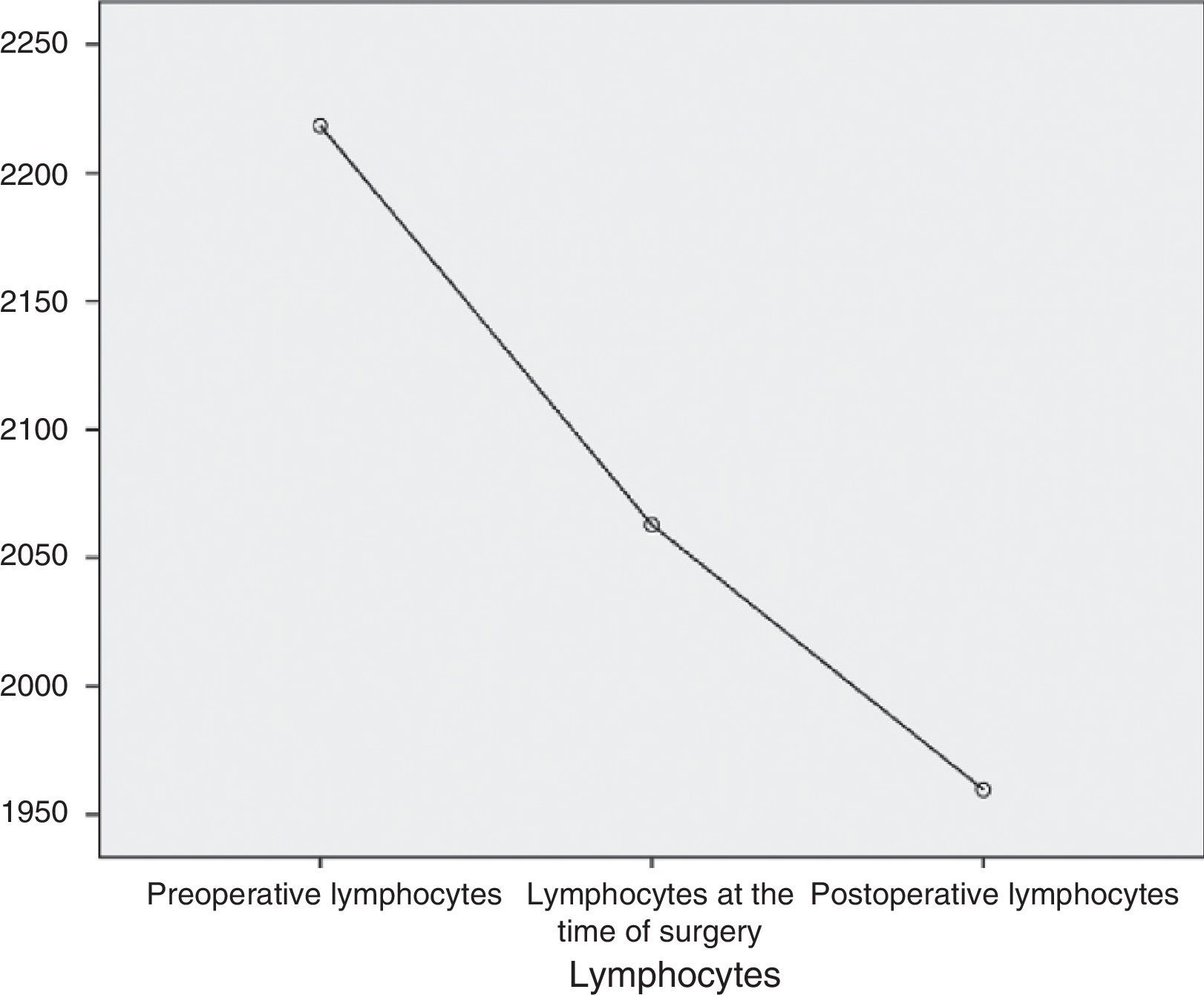
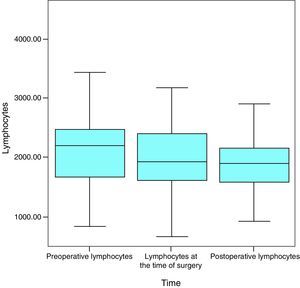
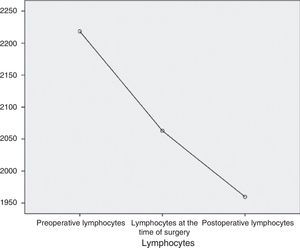
LymphocytesAt the start of the study the average figure for lymphocytes was 2218.4μL, the median was 2198.5μL and the standard deviation was 765.3μL, with a maximum figure of 4500μL and a minimum figure of 840μL. One month later the average was 2062.9μL (a variation of −155.5mg/dL; 7%), the median was 1925μL and the standard deviation was 803.5μL, with a maximum figure of 4170μL and a minimum figure of 670μL. In the month after surgery the average figure for lymphocytes was 1959.7μL (a variation of −103.2mg/dL; 5%), the median was 1900.5μL and the standard deviation was 584.2μL, with a maximum of 3920μL and a minimum of 920μL (Fig. 5).
The normal values for lymphocytes range from 900μL to 5200μL, so that, as it can be seen, the average figure for lymphocytes remained within this range at all times in this study.
With the VLCD lymphocyte levels fell to pathological levels in 4.76% of the patients (2 patients). However, they recovered from this deficit in the month after surgery, so that their values were not significant from a clinical viewpoint.
When all of the patients are considered, lymphocyte levels fell in a statistically significant way throughout the successive measurements (P=.013) (Fig. 6).
DiscussionAlthough it is unclear when the practice started of subjecting patients who were going to receive bariatric surgery to a weight loss diet beforehand, the first published information on this dates from 1995. This described the results obtained in a cohort of patients operated on by a gastric by-pass or ringed vertical gastroplasty from 1978 to 1986.2,3
Two outstanding benefits of subjecting patients to a period of weight loss before surgery are a reduction in hepatic volume and abdominal fat. These aid and facilitate surgery, reducing the number and severity of surgical complications and improving the response to postoperative dietary changes.1
On the other hand, it is fundamental that patients be well nourished if the surgery is to produce optimum results. In fact, increasing attention is being paid to this question, given that anything which negatively affects the nutritional state of a patient increases the probability of greater morbimortality after any surgical procedure (Cabrerizol et al., 1999). In this context, and given that surgical interventions may aggravate any pre-existing state of malnutrition, it is important to ensure that preoperative weight loss does not alter the nutritional condition of obese patients who will be subjected to bariatric surgery.
Different methods of achieving a suitable weight loss before surgery have been used and analysed. They include VLCD,4 hypocaloric diets,5 intragastric balloons,6 the restrictive endoscopic duodenojejunal device7 or cognitive-behavioural therapy.8
VLCD are the treatment of choice when rapid weight loss is desired, given that they have been shown to effective methods of safe weight loss. Due to this they are becoming more widespread in the context of bariatric surgery with the aim of achieving an appropriate weight loss before surgery.2
Although increasing numbers of patients who will receive bariatric surgery are first placed on a VLCD, to date no studies have examined the nutritional safety of this practice. The importance of our study should therefore be highlighted, given that its results show that weight loss using a VLCD prior to surgery is safe in nutritional terms.
Weight loss using a VLCD usually amounts to 10% of patients’ initial weight, while in some cases a loss of 15% may be achieved. Practically 100% of patients lose from 5% to 10% of absolute weight.5 In fact, in our workgroup this percentage of weight loss is an indispensable requisite to enter the bariatric surgery programme.
It has been said that up to 15% of patients placed on a VLCD may present some type of comorbidity as a result of this.9 In our study 9.5% of the patients became anaemic, while the number of lymphocytes fell to pathological levels in 4.76% of the patients and 9.5% had an albumin deficit. Additionally, these deficits were recovered during the month after surgery, so that they cannot be considered significant from a clinical point of view.
The data obtained were therefore within the expected range, given that these alterations were always less than the above-mentioned 15% complications rate. It can therefore be said that preoperative weight loss using a VLCD does not lead to a clinically significant level of malnutrition, so that this cannot be considered to be a sufficient criterion for not prescribing it.
Possible malnutrition had been one of the greatest concerns of the scientific community in connection with weight loss using a VLCD before bariatric surgery. However, this VLCD-induced weight loss does not lead to significant malnutrition, and when analytic variations occur they return to normal without complications after the operation.
Regarding the limitations of this study, one of the points that could be improved is the small number of patients who were finally included. With the aim of standardising the techniques and procedures used as far as is possible, to avoid any potential distortion that could have been caused by changes in medical and surgical practice, the study was planned to last a specific period of time rather than to cover a specific number of patients. It was also restricted to the month prior to surgery and the month after the same. Moreover, only bariatric surgery using gastric by-pass is included. This study excluded habitual bariatric procedures such as the gastric band, the sleeve gastrectomy, the duodenal switch and others. Thus given that the Hospital Universitario General de Castellón performs 1 or 2 bariatric procedures a week, except in holiday periods, and that only gastric bypass operations were included, a total of 50 patients was estimated, of which 8 were excluded due to lack of data. Nevertheless, the data analysed and the results obtained with this number of patients are sufficiently significant to infer that the results would be similar for a larger sample.
Another aspect of this work that could be improved is patient follow-up time. Nevertheless, given that the main aim was to evaluate nutritional parameters during the VLCD diet and to compare them with those corresponding to a month after surgery, this limitation is less important. However, it would be interesting to have a longer term patient follow-up of 5–10 years, opening the doors for future studies in this field.
On the other hand, this study did not include a control group who did not follow a VLCD to achieve weight loss prior to surgery, so that the results of both could have been compared. This is because the good results over years of experience mean this weight loss is now part of care protocol in the Hospital Universitario General de Castellón. Following a VLCD during the month before surgery is a condition sine qua non for the operation. Nevertheless, it may be possible within a controlled clinical trial to consider the suitability and benefits of including a control group.
Lastly, this work does not compare different ways of losing weight before surgery. These may have included longer or shorter VLCD diets, other types of hypocaloric diets or behavioural therapies, among others. Although this was not the aim of our study, here too there is a broad range of possibilities for future scientific research.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Bennasar Remolar MÁ, Martínez Ramos D, Ortega Serrano J, Salvador Sanchís JL. Alteraciones nutricionales tras dieta muy baja en calorías previa a cirugía bariátrica. Cir Esp. 2016;94:159–164.