Appendiceal mucocele is a rare disease with an incidence that ranges between 0.2% and 0.4% of all appendectomies.1–4 It is generally asymptomatic and is an incidental finding. When it causes symptoms, the most common are abdominal pain or a palpable mass in the RLQ.
We report the case of a 62-year-old male patient with a history of arterial hypertension and hyperuricemia. He reported symptoms that had been developing over the past 4 months characterized by postprandial fullness and epigastric pain. These symptoms had also been associated with weight loss, jaundiced skin and mucous membranes the week prior to being treated in the Gastroenterology Department.
Laboratory tests showed: bilirubinemia 6.6mg/dl, direct bilirubin 5.03mg/dl, and other parameters (including CA 19-9 and CEA) were within normal range. A CT of the chest and abdomen revealed a lesion in the second portion of the duodenum that measured 4.9×4.1cm and was compatible with a neoplastic process. This produced dilatation of the intra- and extrahepatic biliary tract with moderate gastric distension; there was no evidence of liver or lung metastases.
Upper gastrointestinal endoscopy revealed a malignant-looking stenotic lesion in the second portion of the duodenum, suggestive of extrinsic origin. Biopsies showed no evidence of malignant disease.
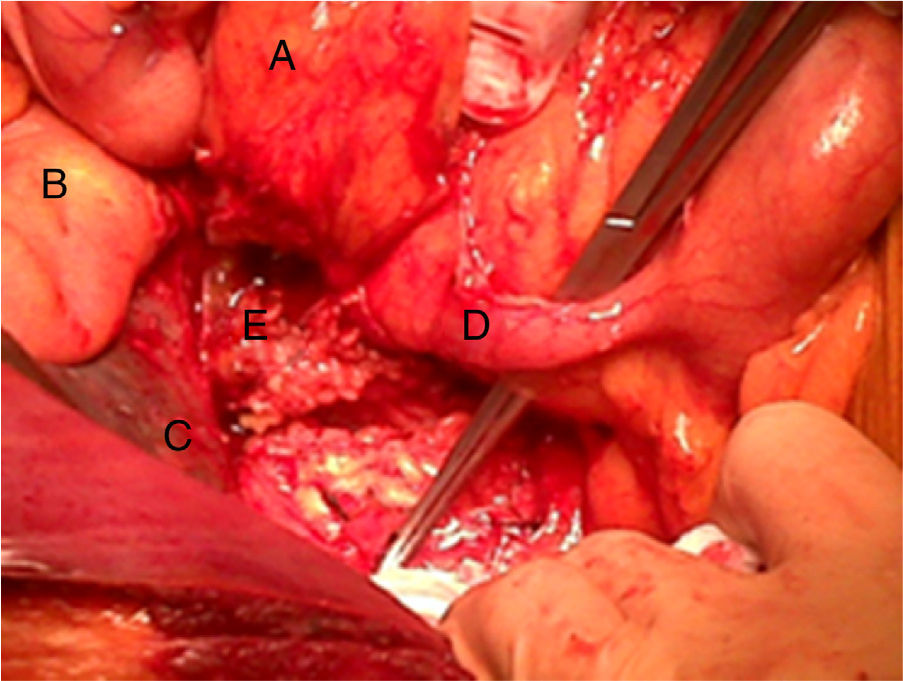
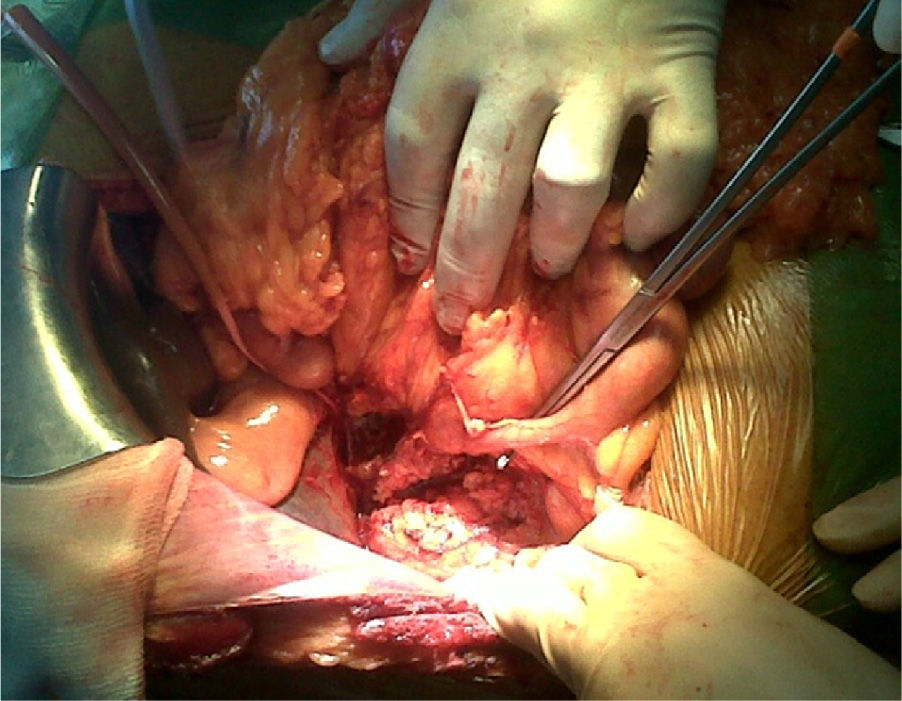
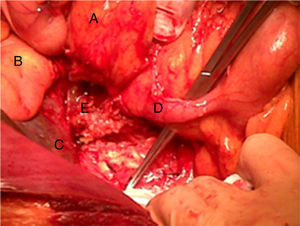
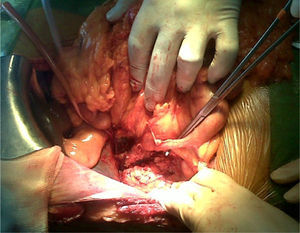
The patient was transferred to our General Surgery Department for scheduled surgery. During the procedure, we observed a retroperitoneal tumor infiltrating the duodenum and head of the pancreas. It originated at the appendix, which was in an anomalous position due to intestinal malrotation that generated retraction of the cecum. The intraoperative sample identified the mass as a mucinous adenocarcinoma, and we therefore decided to carry out total pancreaticoduodenectomy and right hemicolectomy (Fig. 1).
The final pathology study reported a colloid adenocarcinoma originating in the vermiform appendix and established on a papillary adenoma that infiltrated the colon, duodenal wall, distal common bile duct and head of pancreas.
During the postoperative period, the patient developed an intra-abdominal abscess that resolved with antibiotic therapy and percutaneous drainage.
Afterwards, the patient received chemotherapy as prescribed by the Oncology Department. To date, the patient has had no evidence of recurrence after more than 20 months of follow-up.
The incidence of appendix tumors is low. One type is appendiceal mucocele, which leads to dilatation of the appendiceal lumen caused by mucinous material in its interior. It includes several disease processes, some benign and, in other cases, malignant such as mucinous cystadenocarcinoma.
The epidemiology varies according to the series, although most do not find any differences between males and females. What the series do agree on is the age at presentation, which is most frequent between the fifth and sixth decades of life.1–8
The most frequent form of presentation is pain/discomfort in the right iliac fossa.2 Other symptoms and signs have also been described, such as weight loss, intermittent colic pain, urinary symptoms due to extrinsic ureteral compression, changes in bowel habits, lower gastrointestinal tract bleeding and even metrorrhagia.5,6 There are unusual forms of presentation, but we have found no cases in which the reason for hospitalization was obstructive jaundice and epigastric pain, because in our patient there was associated intestinal malrotation. This is caused by a congenital anomaly of intestinal fixation and rotation, comprised of a series of positional abnormalities of the intestine that occur between the 5th and 11th weeks of gestation that result in incorrect, incomplete or absent intestinal rotation. Its incidence has not been determined since some cases are diagnosed during adulthood as incidental findings.9 However, most cases (between 64% and 80%) are diagnosed in the first month of life due to volvuli or Ladd bands.
The absence of the last stage of intestinal rotation in our patient situated the appendix in the region of the right hypochondrium, retroperitoneal, with the cecum and ascending colon occupying the theoretical region of the transverse colon (Fig. 2).10
This anomalous location of the appendix, and its tumor, produced compression/infiltration of the common bile duct, causing obstructive jaundice as well as duodenal infiltration and stenosis.
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: Álvarez Seoane R, García Novoa A, Gómez Gutierrez M. Ictericia obstructiva por adenocarcinoma mucinoso de apéndice en paciente con malrotación intestinal. Cir Esp. 2014;92:131–133.