Outpatient treatment of uncomplicated acute diverticulitis is safe and effective. The aim of this study was to determine the impact of outpatient treatment on the reduction of healthcare costs.
Patients and methodsA retrospective cohort study comparing two groups was performed. In the outpatient treatment group, patients diagnosed with uncomplicated acute diverticulitis were treated with oral antibiotics at home. In the hospital treatment group, patients met the criteria for outpatient treatment but were admitted to hospital and received intravenous antibiotic therapy. Cost estimates have been made using the hospital cost accounting system based on total costs, the sum of all variable costs (direct costs) plus overhead expenses divided by activity (indirect costs).
ResultsA total of 136 patients were included, 90 in the outpatient treatment group and 46 in the hospital group. There were no differences in the characteristics of the patients in both groups. There were also no differences in the treatment failure rate in both groups (5.5% vs 4.3%; p=0.7). The total cost per episode was significantly lower in the outpatient treatment group (882±462 vs 2376±830 euros; p=0.0001).
ConclusionsOutpatient treatment of acute diverticulitis is not only safe and effective but also reduces healthcare costs by more than 60%.
El tratamiento ambulatorio de la diverticulitis aguda no complicada es seguro y eficaz. El objetivo de este estudio es cuantificar el impacto que el tratamiento ambulatorio tiene en la reducción de costes sanitarios.
Pacientes y métodosEstudio comparativo de cohortes retrospectivo. Grupo ambulatorio: pacientes diagnosticados de diverticulitis aguda no complicada tratados con antibióticos vía oral de forma ambulatoria. Grupo de tratamiento hospitalario: pacientes que cumplían criterios de tratamiento ambulatorio pero que fueron ingresados con tratamiento antibiótico intravenoso. La valoración de costes se ha realizado a través del sistema de contabilidad analítica del hospital, basado en costes totales: suma de todos los costes variables (costes directos) más el conjunto de costes generales repartidos por actividad (costes indirectos).
ResultadosSe incluyó a 136 pacientes, 90 en el grupo ambulatorio y 46 en el grupo de ingreso. No hubo diferencias en las características de los pacientes entre los 2 grupos. No hubo diferencias en el porcentaje de fracaso del tratamiento entre los 2 grupos (5,5 vs. 4,3%; p=0,7). El coste global por episodio fue de 882±462 euros en el grupo ambulatorio frente a 2.376±830 euros en el grupo hospitalario (p=0,0001).
ConclusionesEl tratamiento ambulatorio de la diverticulitis aguda no solo es seguro y eficaz sino que también reduce más de un 60% los costes sanitarios.
Conventional treatment of uncomplicated acute diverticulitis involves patient hospitalization with intravenous antibiotic therapy, fluid therapy and no oral intake until symptoms are resolved.1–3 In recent years, it has been proposed that selected patients could be treated on an outpatient basis with liquid diet for the first few days and oral broad-spectrum antibiotics.4 Several published papers have shown that outpatient treatment of uncomplicated acute diverticulitis is safe, effective and applicable in most patients.5–10 Between 2003 and 2005, a prospective study was carried out in our hospital with 40 patients diagnosed with uncomplicated acute diverticulitis, treated in the outpatient setting.9 That initial study already showed that outpatient treatment was applicable in more than 75% of patients and that, moreover, it was safe and effective. These results were later confirmed in a longer series of 70 patients.10
An additional advantage of outpatient treatment of uncomplicated acute diverticulitis is the reduction of healthcare costs, as is the case with most procedures performed on an outpatient basis. This is a very important point because there is a growing need to improve the economic efficiency of patient care, without compromising results. The objective of this study was to quantify the impact that outpatient treatment has in reducing healthcare costs.
Patients and MethodsStudy Subjects and DesignPatients eligible for the present retrospective study had been diagnosed with uncomplicated acute diverticulitis according to their medical history, physical examination and abdominal CT findings during the period between January 2005 and June 2011 at the Hospital del Mar.
Included in the study were all patients diagnosed with uncomplicated acute diverticulitis who met the criteria to be treated as outpatients in accordance with the protocol of our Unit: tolerance to oral intake prior to discharge from the emergency department, absence of comorbidities and adequate family or social support. The CT diagnostic criteria for uncomplicated acute diverticulitis included the presence of diverticula with colon wall thickening (>4mm) or pericolonic fat stranding.11
The cohort was divided into two groups:
- -
Outpatient treatment group: patients diagnosed with uncomplicated acute diverticulitis treated with oral antibiotics as outpatients.
- -
Hospital treatment group: patients diagnosed with uncomplicated acute diverticulitis who met criteria for outpatient treatment but were admitted for intravenous antibiotic therapy; therefore, the outpatient treatment protocol was not applied. Despite having met outpatient criteria, reasons for hospitalization included unawareness of the precise criteria for hospitalization and, in most cases, decision of the doctor based on persistent pain.
Outpatient treatment of patients with uncomplicated acute diverticulitis consisted of liquid diet for the first 2 days and oral antibiotics for 7 days (amoxicillin-clavulanate 1g/8h or associated ciprofloxacin 500mg/12h and metronidazole 500mg/8h in patients allergic to penicillin) combined with oral analgesia (paracetamol 1g/8h). Once discharged from the Emergency Department, a follow-up visit was scheduled at the outpatient clinic of the Colorectal Surgery Unit between 4 and 7 days after diagnosis to confirm appropriate clinical course. Hospitalized patients received intravenous antibiotic treatment with cefotaxime 1g/6h and metronidazole 500mg/8h. In the last three years, the intravenous treatment pattern changed to intravenous amoxicillin-clavulanate 1g/8h. Hospitalized patients were discharged when they showed an improvement in their symptoms, and they completed the oral antibiotics at home.
In all cases, fiber optic colonoscopy was ordered between 1 and 3 months after the episode to confirm the diagnosis and rule out the presence of other lesions in the colon. If a recurrence presented months after the episode of diverticulitis, the patients were once again included in the same protocol.
We made a comparison of the patient characteristics; ER consultations in the first days after discharge, readmissions and reasons for readmission were all recorded. Likewise, the antibiotic regimen received during the hospital stay was recorded for all inpatients, and treatment and duration were recorded for outpatients. Recurrences during follow-up were also recorded.
Cost AnalysisThe cost estimate was performed with data from the accounting system of the hospital, based on total costs established in 2004, which were still currently valid.12 This system ensures that all costs, both fixed and variable, are divided between all the episodes treated. This means that the cost of each episode is the sum of all variable costs (direct costs) plus the overhead costs allocated by activity (indirect costs). The remaining general costs that are directly attributable to the patient have been input with activity-based criteria. The cost includes outpatient treatment in both the study group (complete treatment) and in the control group when they completed treatment once discharged.
Statistical AnalysisQuantitative variables were expressed as mean±standard deviation and the qualitative variables as absolute numbers or percentages of the total number of patients studied. The comparison between quantitative variables was done with the Student's t test, and the Chi squared test was used for qualitative variables. Statistical significance was considered when p was less than 0.05. The data analysis was performed using SPSS version 13.0. The comparative analysis was performed by intention to treat.
ResultsDuring the study period, 136 patients were diagnosed with uncomplicated acute diverticulitis and met criteria for outpatient treatment. In the end, 90 patients began outpatient treatment while the remaining 46 were hospitalized with intravenous antibiotic therapy. Despite meeting criteria for outpatient treatment, the reasons for hospitalization were: unawareness of the precise criteria for hospitalization and, in most cases, decision of the doctor due to persistent pain.
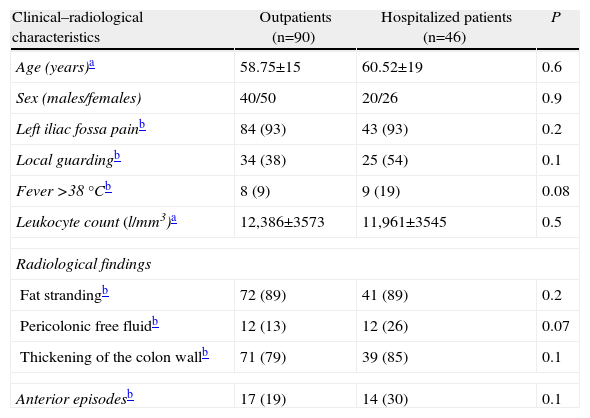
Table 1 shows the patient characteristics. We observed no statistically significant differences in age, sex, clinical manifestations or radiological findings on CT, although the percentage of patients with localized guarding in the left iliac fossa, fever and pericolonic free fluid was higher in the group of hospitalized patients. All patients who were treated as outpatients were in the ER for less than 24h, while the mean hospital stay of inpatients was 6 days with a range from 2 to 10 days.
Clinical and Radiological Characteristics of the Patients Diagnosed With Uncomplicated Acute Diverticulitis in the Two Study Groups.
| Clinical–radiological characteristics | Outpatients (n=90) | Hospitalized patients (n=46) | P |
| Age (years)a | 58.75±15 | 60.52±19 | 0.6 |
| Sex (males/females) | 40/50 | 20/26 | 0.9 |
| Left iliac fossa painb | 84 (93) | 43 (93) | 0.2 |
| Local guardingb | 34 (38) | 25 (54) | 0.1 |
| Fever >38°Cb | 8 (9) | 9 (19) | 0.08 |
| Leukocyte count (l/mm3)a | 12,386±3573 | 11,961±3545 | 0.5 |
| Radiological findings | |||
| Fat strandingb | 72 (89) | 41 (89) | 0.2 |
| Pericolonic free fluidb | 12 (13) | 12 (26) | 0.07 |
| Thickening of the colon wallb | 71 (79) | 39 (85) | 0.1 |
| Anterior episodesb | 17 (19) | 14 (30) | 0.1 |
In total, 7 patients returned to the Emergency Department after discharge: 5 of the 90 patients in the outpatient treatment group due to persistent pain, fever or nausea, who were hospitalized; and, 2 patients from the hospital treatment group were readmitted due to recurrence of symptoms (5.5% vs 4.3%; P=.7). None of these 7 patients required emergency surgery during their hospital stay, and intravenous treatment resolved the inflammatory process in all cases. Mean follow-up was 17±5 months. During this time, recurrence of the diverticulitis was seen in 16 (18%) patients in the outpatient group and 10 (22%) cases in the inpatient group, although the difference was not statistically significant (p=0.6).
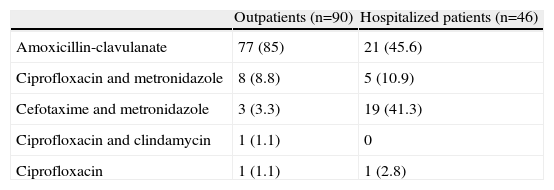
Table 2 shows the antibiotic treatment used in the two groups. Patients in the hospital treatment group received cefotaxime and metronidazole or amoxicillin-clavulanate. All patients in the intravenous treatment group continued with amoxicillin-clavulanate orally to complete the 7-day treatment once discharged from hospital.
Antibiotic Treatment Administered to the Patients of the Two Groups.
| Outpatients (n=90) | Hospitalized patients (n=46) | |
| Amoxicillin-clavulanate | 77 (85) | 21 (45.6) |
| Ciprofloxacin and metronidazole | 8 (8.8) | 5 (10.9) |
| Cefotaxime and metronidazole | 3 (3.3) | 19 (41.3) |
| Ciprofloxacin and clindamycin | 1 (1.1) | 0 |
| Ciprofloxacin | 1 (1.1) | 1 (2.8) |
Results expressed as absolute numbers and percentages.
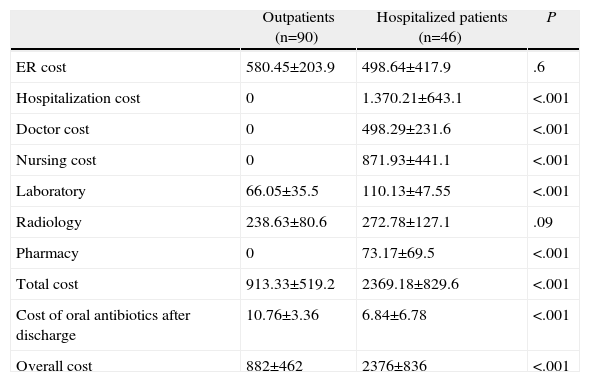
Table 3 shows the comparison of costs between the two groups. The overall healthcare cost per episode was significantly lower in the study group compared with the control group (882±462 vs 2376±830 euros; P=.0001). This cost is the sum of the total cost of all healthcare services provided, including the oral antibiotics with which the patient was discharged.
Total Cost of Uncomplicated Acute Diverticulitis Treatment, Broken Down According to the Two Study Groups.
| Outpatients (n=90) | Hospitalized patients (n=46) | P | |
| ER cost | 580.45±203.9 | 498.64±417.9 | .6 |
| Hospitalization cost | 0 | 1.370.21±643.1 | <.001 |
| Doctor cost | 0 | 498.29±231.6 | <.001 |
| Nursing cost | 0 | 871.93±441.1 | <.001 |
| Laboratory | 66.05±35.5 | 110.13±47.55 | <.001 |
| Radiology | 238.63±80.6 | 272.78±127.1 | .09 |
| Pharmacy | 0 | 73.17±69.5 | <.001 |
| Total cost | 913.33±519.2 | 2369.18±829.6 | <.001 |
| Cost of oral antibiotics after discharge | 10.76±3.36 | 6.84±6.78 | <.001 |
| Overall cost | 882±462 | 2376±836 | <.001 |
The case load and healthcare costs due to diverticular disease has steadily increased in recent years. According to data from the National Hospital Discharge Survey,13 diverticular disease is responsible for 312,000 hospital admissions and 1.5 million days of hospitalization per year in the U.S. The annual cost is estimated at about $2.6 billion per year.14 In a recent study, it was found that 80% of patients with acute diverticulitis are treated conservatively with intravenous antibiotics, so that an outpatient treatment protocol would result in a significant reduction in the average cost of treating this disease.15 In the present study, we demonstrate that outpatient treatment reduced healthcare costs associated with treating this disease by more than 60%, even with such a high prevalence. This is especially important at a time of severe economic hardship, as we are currently experiencing. In this regard, the reduction in health care costs observed in this present study is similar to that recently described by Moya et al.16 In a nonrandomized comparative study, the authors compared the efficacy, safety and costs in a group of 44 patients with uncomplicated acute diverticulitis who received intravenous antibiotic therapy and a group of 32 patients who were treated on an outpatient basis. The reduction in costs was 1600 euros per episode of diverticulitis, mainly due to the shorter hospital stay. Martín-Gil et al.17 had previously demonstrated that outpatient treatment of uncomplicated acute diverticulitis was able to reduce hospital costs by 40%. However, from the methodological point of view, it should be noted that in this study the shortened stay and reduced total expense were achieved by considering an average hospitalization time to be 10 days per patient. In our study, we have observed a reduction in spending of more than 60%, even though the average stay of hospitalized patients was less than 7 days.
According to these results, the treatment of choice in most patients with uncomplicated acute diverticulitis should be ambulatory and with oral antibiotics. Although there are no data on the implementation of outpatient treatment in Spain, we can make estimations with the existing literature, which is still very limited although in recent years ample evidence has appeared demonstrating the safety and effectiveness of this form of treatment.16–18
Moreover, the results of this study confirm that the ambulatory treatment of uncomplicated acute diverticulitis is safe and effective because the inflammatory process was resolved in more than 90%. Only 5 out of 90 patients treated with oral antibiotics at home were readmitted after being discharged from the Emergency Department, and in none of those cases did the diverticulitis become complicated.
The application of less stringent exclusion criteria and individualized decision-making could increase the applicability of outpatient treatment (which in our first series was 75%) and further reduce the costs associated with the treatment of this disease.9 In most patients with diabetes mellitus, heart failure or renal failure presenting uncomplicated diverticulitis, there is no decompensation of their chronic disease and outpatient treatment is possible. An alternative to hospitalization in these patients is a home hospital program. In a prospective series of 176 patients with uncomplicated acute diverticulitis, 33 (18%) with comorbidities were successfully treated at home with intravenous antibiotics, with a high percentage of satisfaction expressed by patients.19
One aspect of this study that should be discussed is the high number of patients (46 out of 136 patients; 33%) who were hospitalized for intravenous antibiotic treatment despite meeting criteria for outpatient treatment. One reason was the unawareness of the exact criteria for inclusion and exclusion of the protocol. Thus, elderly patients and those with recurrence were hospitalized when neither of these two situations are exclusion criteria. In most cases, however, the decision to admit the patient was made by the doctor on call due to persistent pain, even though the inflammatory parameters had improved on the work-up. Thus, clinical judgment prevailed over the criteria in the written protocol. In this regard, it should be noted that, although the differences were not significant, the percentage of patients with guarding, fever and pericolonic free fluid on CT was higher in the group of patients who were admitted. It is very likely that these clinical and radiological signs influenced the decision of the surgeon who treated the patient even though patients met the criteria for outpatient treatment. It should also be noted that the evolution in most of these patients was satisfactory, contrary to a recent retrospective study which showed that patients with free fluid on CT also had an increased risk of outpatient treatment failure.20 Furthermore, the high number of patients who were not treated under the protocol allowed us to have a control group with exactly the same characteristics as the outpatient treatment group. From a methodological standpoint, this provides additional value to the results obtained.
Since this is an uncontrolled study, the two groups did not receive the same antibiotic treatment and that could be considered a limitation. While the vast majority of patients treated as outpatients received amoxicillin-clavulanate or ciprofloxacin and metronidazole in case of allergy to penicillin, the intravenous treatment regimen was more varied. This is partly due to the fact that in the last three years the intravenous treatment pattern changed to intravenous amoxicillin-clavulanate 1g/8h. However, most of the hospital treatment cost is due to the physician and nursing costs, while the pharmaceutical cost is less than 5% of the total hospitalization.
Continuing with the evolution of the treatment of uncomplicated acute diverticulitis, some authors have gone a step further and have suggested that these patients do not require antibiotic treatment.21 A recent randomized multicenter study compared a group of 314 patients diagnosed with acute diverticulitis and treated with antibiotics with another group of 309 patients who received no antibiotic treatment.22 The authors observed that antibiotic therapy does not speed recovery or prevent the development of complications or recurrences, so they recommend reserving antibiotic treatment for complicated diverticulitis. Although the proposal is interesting, it is noteworthy that the patients in both groups were hospitalized. First of all, it will be necessary to demonstrate the safety of outpatient treatment without antibiotics before proposing it as a therapeutic option for uncomplicated acute diverticulitis. Moreover, the results of our study show that the highest cost-efficiency is achieved by avoiding hospitalization, not by suppressing antibiotic treatment.
In short, outpatient treatment of uncomplicated acute diverticulitis is not only safe and effective, but it is also able to reduce healthcare costs by more than 60%.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Lorente L, Cots F, Alonso S, Pascual M, Salvans S, Courtier R, et al. Tratamiento ambulatorio de la diverticulitis aguda no complicada: impacto sobre los costes sanitarios. Cir Esp. 2013;91:504–509.