To study the recurrence/persistence rate of complex cryptoglandular anal fistula after the LIFT procedure and analyze the patterns of recurrence/persistence.
MethodsObservational study of patients with transe-sphincteric or supra-sphincteric anal fistula treated using the LIFT procedure from December 2008 to April 2016. Variables studied included clinical characteristics, surgical technique and results. Clinical cure was defined and imaging studies were used in doubtful cases. Wexner's score was used for continence evaluation. The minimum follow-up time was one year.
ResultsA total of 55 patients were operated on: 53 with a trans-sphincteric fistula and 2 supra-sphincteric. There were 16 failures (29%): 7 complete fistulas (original), 6 intersphincteric (downstage), and 3 external residual tracts. A posterior location and complexity of the tract were risk factors for recurrence/persistence. The presence of a seton did not improve results. No case presented decrease of continence (Wexner 0). Nine patients presented minor complications (9%): 4 intersphincteric wounds with delayed closure and one external hemorrhoidal thrombosis. The median time to closure of the external opening was 5 weeks (IR 2–6). Intersphincteric wounds closed in 4–8 weeks.
ConclusionIn our experience, the LIFT technique is a safe and reproducible procedure with low morbidity, no repercussion on continence and a success rate over 70%. There are 3 types of recurrence: the intersphincteric fistula, the original fistulatula (trans- or supra-sphincteric) and the residual external tract. Considering the types of recurrence, only 12.7% of patients need more complex surgery to solve their pathology. The rest of the recurrences/persistence was solved by simple procedures (fistulotomy in intersphincteric forms and legrado in residual tracts).
Valorar la recidiva/persistencia de la fístula anal compleja tras cirugía de tipo LIFT y analizar los patrones de recurrencia/persistencia.
MétodoEstudio observacional de pacientes afectos de fístula anal transesfinteriana o supraesfinteriana tratada mediante la técnica LIFT durante el periodo diciembre de 2008-abril de 2016. Se analizan las características clínicas, la técnica quirúrgica y su resultado. Se define la curación clínica y se emplean pruebas de imagen en casos de duda. Se utiliza la escala Wexner para el estudio de la continencia. El tiempo mínimo de seguimiento ha sido de un año.
ResultadosUn total de 55 pacientes fueron intervenidos: 53 con fístula transesfinteriana y 2 supraesfinteriana. Se produjeron 16 fracasos (29%): 7 fístulas completas (originales), 6 interesfinterianas (downstage) y 3 trayecto residuales externos. La localización posterior y la complejidad del trayecto fueron factores de riesgo de recurrencia/persistencia. La presencia de un sedal previo no mejoró los resultados. Ningún caso presentó alteración de la continencia (Wexner 0). Del total, 9 pacientes presentaron complicaciones leves (9%): 4 heridas interesfinterianas con cierre tardío y una trombosis hemorroidal externa. La mediana del cierre del orificio externo fue de 5 semanas (RI: 2-6). Las heridas interesfinterianas curaron en 4-8 semanas.
ConclusiónLa técnica de LIFT en nuestra experiencia ha resultado una operación segura, reproductible, con escasa morbilidad, nula repercusión en la continencia y un porcentaje de éxito superior al 70%. Se definen 3 tipos de recurrencia: la fístula interesfinteriana, la fístula original (trans- o supraesfinteriana) y el trayecto externo residual. Considerando los tipos de recurrencia, tan solo el 12,7% de los pacientes han necesitado cirugías más complejas para solucionar esta entidad. El resto de las recurrencias/persistencias se han solucionado con gestos simples (fistulotomía en la formas interesfinterianas y legrados en los trayectos residuales).
The objectives of anal fistula treatment are to eradicate sepsis, close the fistulous tract, avoid recurrence and preserve continence. Many surgical interventions have been described, which can basically be classified as sphincter-preserving or non-sphincter preserving. Fistulotomy has the best results in fistula eradication, with success rates above 90%,1 but it also entails an important percentage of continence disorders.2 Fistulotomy with sphincteroplasty has provided excellent results in some groups, but its use has not spread in the surgical community.3 Among the preservation techniques, advancement flap, plugs and sealants have been the most widely used. However, flaps can be very technically demanding, despite their good results. Furthermore, all plugs, sealants or glues have been showing decreasing success rates as more series are published.4
In 2007, Arun Rojanasakul, a Thai surgeon, published the first results of a sphincter-preserving technique using ligation of the intersphincteric fistula tract (LIFT).5 Since then, this technique has spread among surgeons, with more than 6 variations, making it very complex to draw clear conclusions.6 However, this approach is not so novel; in 1993, Matos et al. described an intersphincteric approach for the treatment of cryptoglandular fistula.7
Dissection of the fistulous tract in the LIFT procedure has resulted in new patterns of recurrence and persistence. This is unlike the remaining techniques, whose failure results in fistulae similar to the original or, in cases such as flaps, even more complex. Tan et al. have discussed this peculiarity.8 The aim of this study was to describe the types of recurrence/persistence after cryptoglandular fistula surgery using the LIFT technique and its evolution over time.
MethodsThis is an observational, retrospective study of patients treated with complex anal fistulae (transsphincteric and suprasphincteric) of cryptoglandular origin from December 2008 to May 2016 at a university hospital using the LIFT technique and registered in a prospective database. The study was approved by the hospital Ethics Committee, and informed consent was obtained in all patients. The fistulae were classified according to the Parks system.9 Transsphincteric fistulae were defined as low or high, depending on whether the tract was palpated or not. In addition, imaging studies (endoanal ultrasound or MRI) were occasionally done after clinical examination. Mechanical preparation was carried out with phosphate enemas and antibiotic prophylaxis with metronidazole and ciprofloxacin. All patients were operated on with hyperbaric spinal anesthesia in the prone position. The surgical technique has been described by Rojanasakul.5,10 The main steps are: placement of a Lockhart Mummery probe, incision in the intersphincteric groove and dissection of the intersphincteric plane with diathermy, dissection of the fistulous tract and placement of 2 absorbable sutures, removal of the probe and proximal double knot; dissection of the tract, curettage of the distal end and closure of the orifice in the external sphincter with absorbable suture in the intersphincteric plane. The dissection of the tract is checked by instillation of saline solution through the external orifice. Finally, the intersphincteric space and groove are closed with absorbable material. According to the preference of the surgeon, excision of the intersphincteric tract was occasionally performed, while on other occasions only very central ligation and dissection of the fistulous tract was used. Antibiotic treatment was continued for 5–7 days, with the same initial dosage. All patients were discharged within the first 24h. Outpatient follow-up office visits were during the second week, after the first and third months, and after one year.
In February 2017, patient files were reviewed and patients were contacted. Excluded from the study were patients with Crohn's disease, as well as those with intersphincteric, extrasphincteric or double fistulae.
Patient variables and fistula characteristics (type, position, distance from the external orifice to the anal margin, etc.) were collected in a prospective database. Likewise, we also collected data about the intervention and outpatient follow-up, paying special attention to the closure of the intersphincteric wound and the primitive external fistulous orifice. Recovery was defined as the closure of wounds, fistulous orifice and absence of suppuration or pain. In cases of suspected persistence or recurrence, patients were examined in the outpatient consultation, operating room or with imaging tests (ultrasound or MRI), depending on the case. Continence was assessed with the Wexner scale.11 The types of recurrence described after the LIFT8 intervention have been followed: persistence of the intersphincteric wound (type I), intersphincteric fistula (type II) and complete fistula (type III).
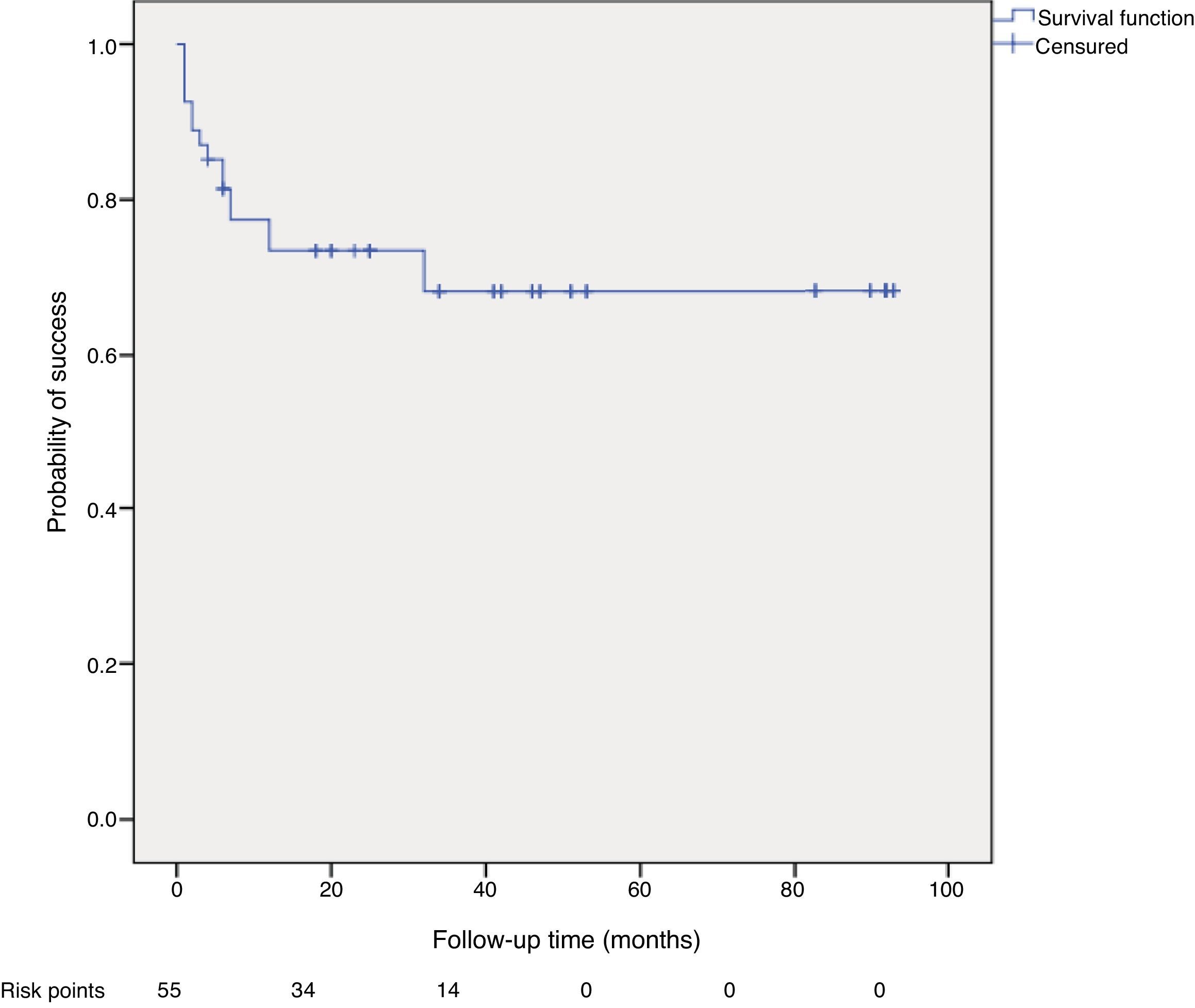
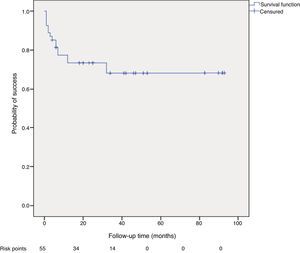
Categorical variables were analyzed using the chi-squared test and Fisher's exact test, and the quantitative variables were analyzed using the non-parametric Mann–Whitney test. A multivariate analysis was completed using binary logistic regression to study the risk factors for recurrence. Variables with univariate significance of 0.2 or less were included. The probability of recurrence was analyzed using the Kaplan–Meier test.
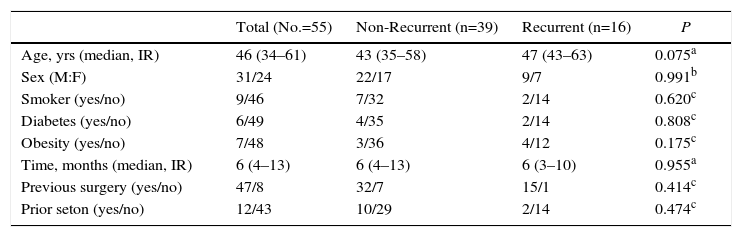
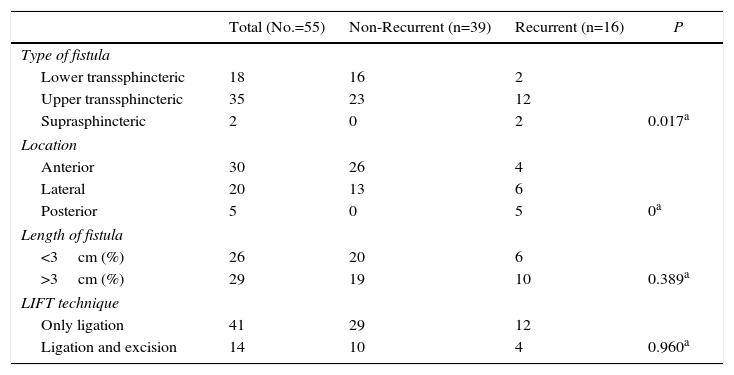
ResultsDuring the study period, 55 patients were included. The median follow-up was 32 months (IR: 6–51), and no patients were lost to follow-up. A total of 16 patients presented recurrence or persistence of the fistula after the LIFT operation (29.09%). The clinical characteristics of the patients are presented in Table 1. There were no differences between the main characteristics of patients with or without recurrence except for age (worse results were observed with greater age, but the difference was not statistically significant). Among the generally accepted risk factors for recurrence (smoking, diabetes, obesity), no differences were observed either. Furthermore, the presence of a previous seton showed no advantage in this series. In addition, more recurrences were not observed in correlation with previous surgeries. The characteristics of the fistulae are shown in Table 2. The length of the fistulous tract did not influence results. However, both the type of fistula and its location were risk factors. More complex fistulae (suprasphincteric and high transsphincteric) showed higher recurrence (P=.017). Meanwhile, those in posterior locations recurred more frequently (P=0). There were no differences for relapse/persistence between the technical methods of ligation of the tract and ligation with excision of the tract (P=.960). The multivariate analysis only detected the fistula type as a risk factor for recurrence (OR 5.5, 95% CI 1.06–27.1) (Figure 1).
Clinical Characteristics of the Series (No.=55 patients).
| Total (No.=55) | Non-Recurrent (n=39) | Recurrent (n=16) | P | |
|---|---|---|---|---|
| Age, yrs (median, IR) | 46 (34–61) | 43 (35–58) | 47 (43–63) | 0.075a |
| Sex (M:F) | 31/24 | 22/17 | 9/7 | 0.991b |
| Smoker (yes/no) | 9/46 | 7/32 | 2/14 | 0.620c |
| Diabetes (yes/no) | 6/49 | 4/35 | 2/14 | 0.808c |
| Obesity (yes/no) | 7/48 | 3/36 | 4/12 | 0.175c |
| Time, months (median, IR) | 6 (4–13) | 6 (4–13) | 6 (3–10) | 0.955a |
| Previous surgery (yes/no) | 47/8 | 32/7 | 15/1 | 0.414c |
| Prior seton (yes/no) | 12/43 | 10/29 | 2/14 | 0.474c |
Characteristics of the Fistulae and Surgical Technique.
| Total (No.=55) | Non-Recurrent (n=39) | Recurrent (n=16) | P | |
|---|---|---|---|---|
| Type of fistula | ||||
| Lower transsphincteric | 18 | 16 | 2 | |
| Upper transsphincteric | 35 | 23 | 12 | |
| Suprasphincteric | 2 | 0 | 2 | 0.017a |
| Location | ||||
| Anterior | 30 | 26 | 4 | |
| Lateral | 20 | 13 | 6 | |
| Posterior | 5 | 0 | 5 | 0a |
| Length of fistula | ||||
| <3cm (%) | 26 | 20 | 6 | |
| >3cm (%) | 29 | 19 | 10 | 0.389a |
| LIFT technique | ||||
| Only ligation | 41 | 29 | 12 | |
| Ligation and excision | 14 | 10 | 4 | 0.960a |
Out of the 16 patients who presented recurrence, 7 (43.7%) were complete fistulae like the original ones, 6 (37.5%) were intersphincteric and 3 (18.7%) were residual tracts outside the external sphincter that were successfully treated (2 with liquid silver nitrate and another with surgical curettage). Out of the 7 patients with complete recurrence, 3 were treated with fistulotomy and sphincteroplasty (with good functional results and no technical difficulties), 2 with loose setons, one with Permacol and one with Tissucol (later recurrence required loose setons). The 6 intersphincteric recurrences were treated by simple fistulotomy with healing in all patients and good functional results. The median time to the appearance of recurrence was 10 weeks (IR: 8–29).
None of the patients presented fecal incontinence after surgery, and the median Wexner score was 0.
Complications were reported in 5 patients (9%): one external hemorrhoidal thrombosis and 4 intersphincteric wounds that took 4–8 weeks to close and required local treatment. In our series, the wounds of the intersphincteric groove were considered a complication of the surgery and not a type of failure: they closed completely with local topical treatment. The wounds that did not close were recurrent intersphincteric fistulae. Suppurative intersphincteric wounds closed in 2–7 weeks, except those of 6 patients who had recurrence/persistence of an intersphincteric fistula. The median time for closure of the external orifice was 4 weeks (IR: 2–6). All recurrences/persistence occurred within the first 10 weeks of follow-up.
DiscussionIn our experience, the LIFT technique has been a safe, reproducible operation, with low morbidity, no impact on continence, and a success rate of more than 70%. In addition, considering the types of recurrence, only 12.7% of the patients have needed more complex surgeries to resolve their condition. The remaining cases of recurrence/persistence have been resolved with simple measures (fistulotomy in the intersphincteric forms and curettage of residual tracts).
The concept of the intersphincteric approach is not new. In 1993, the St Mark's group published a series of 13 patients treated with the intersphincteric procedure, with drainage of the space and closure of the fistulous orifices, both in the internal and external sphincters, with final closure of the wound. The technique was completely successful in 7 patients (53.8%). In addition, 5 patients had inflammatory bowel disease.12 However, this preservation technique had not been updated until the publication in 2007 by Rojanasakul, with some modifications. Recently, there has been a report of another intersphincteric approach using the opening of this space, which calls into question the curative and preserving role of this approach.13
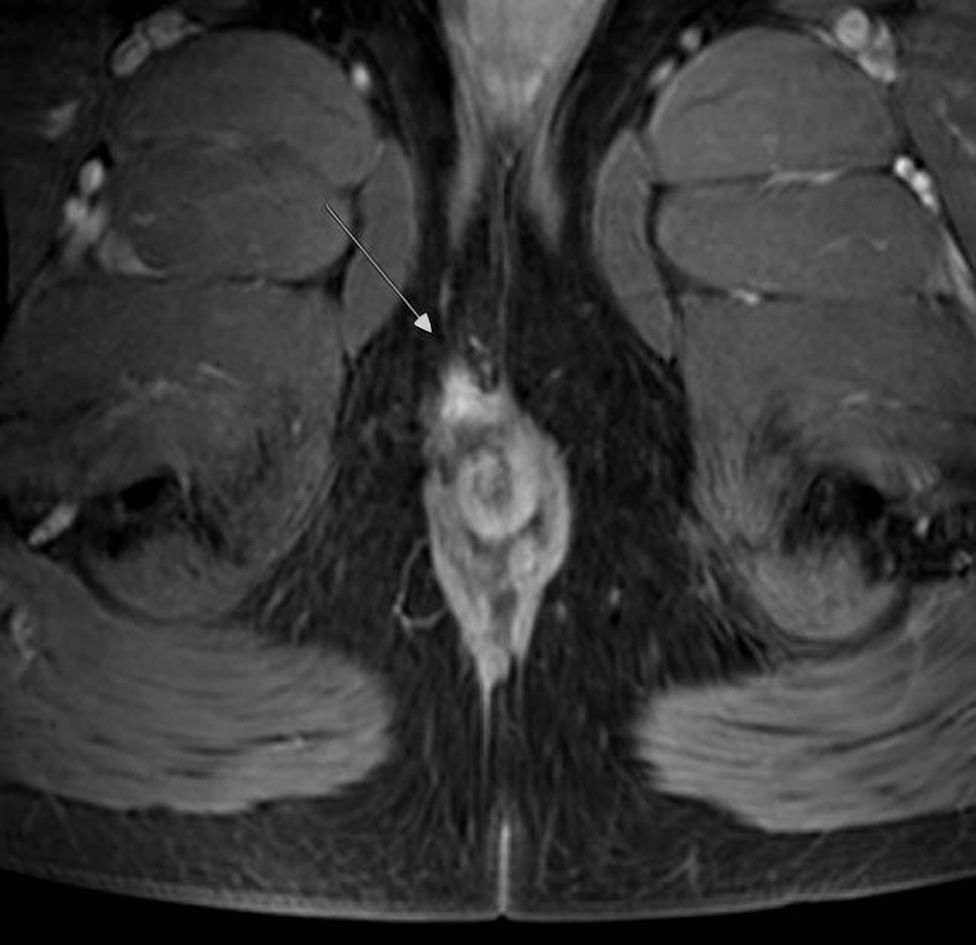
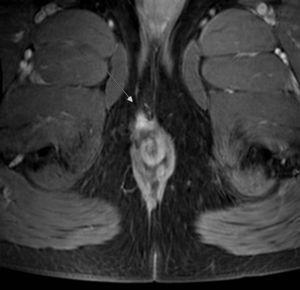
The opening of the intersphincteric space and the dissection of the fistulous tract could lead to a phenomenon of downstaging in recurrence. In a retrospective series of 93 patients, Tan et al.8 described 3 patterns of recurrence/persistence after LIFT surgery: group I with unclosed suppurative intersphincteric wound, group II with intersphincteric fistula, and group III with recurrence/persistence of the complete fistulous tract. In our experience, type I is more a complication of delayed closure than persistence. In our cases, only the 3 patients with persistent/recurrent intersphincteric fistulae presented lack of complete closure of the intersphincteric wound. The rest improved spontaneously with local topical treatment. Even though the external orifice closed very early (2 to 3 weeks in our series), the intersphincteric wound can open and require from 6 to 8 weeks to close. This same experience has been reported by other authors.14 Our results, however, unlike Tan's article, show 3 types of recurrence/persistence patterns, which coincides with the experience of the Australian Schulze group.14 Besides the recurrence/persistence of the intersphincteric fistula and the original trans- or suprasphincteric one, we have found several cases with persistence of the external tract and its external orifice in the absence of internal orifice or communication with the anal canal (Figure 2). Out of our 3 cases, only one required surgery with simple curettage and another 2 were treated with silver nitrate. There are several ways to complete the external treatment of the tract outside the intersphincteric ligation: curettage, core-out or seton. The limited literature that deals with this aspect does not show clear advantages of any of the different options.8,14,15
The impact on continence is often limited or zero, as in our case series. This fact is recognized in most reviews about the LIFT technique and represents a strong point of the technique in cases of recurrence, something that does not occur with other more widespread techniques.6,15–19 Tsunoda et al. prospectively evaluated anal continence in 20 patients, using anal manometry and function scores. They found that there were no changes in pressures, rest or contraction after LIFT-type surgery.20
In our experience, the placement of a loose seton prior to the LIFT technique offers no advantages. This point has created controversy since the publication of the technique.15 It is true that the presence of a tract that is not very fibrous makes it difficult or impossible to perform the technique; however, prior use of a seton does not guarantee greater consistency of the tract. Some studies even point out that the creation of false tracts during the placement of the seton could further complicate surgery.21 In an attempt to improve the consistency of the tract for ligation, a trial has studied the joint use of a plug. However, the results have not improved the overall technique outcomes in the few studies published.22
Few studies have analyzed the location of the fistula and its correlation with outcome. In our experience, a posterior location obtained the worst results with the LIFT technique, which is perhaps related with the greater complexity of these fistulae. In the largest LIFT series published, Parthasarathi et al. concur in this regard and attribute this to the greater technical difficulty of the dissection of the intersphincteric tract in this location.23
In complex fistulae of cryptoglandular origin, no intervention has demonstrated clear superiority over the rest. In addition, the level of evidence is very low, with few randomized studies.16 The LIFT operation is a very good choice in complex fistulae, with success rates above 70%, no repercussions on continence, and recurrence/persistence patterns that make re-operations easier. In addition, the minimal distortion that occurs in the anal anatomy and the absence of continence alterations allow for new surgeries to be performed, or the same procedure could even be repeated, as shown by Rojanasakul.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Placer Galán C, Lopes C, Múgica JA, Saralegui Y, Borda N, Enriquez Navascues JM. Patrones de recurrencia/persistencia en la operación de LIFT para la fístula anal de origen criptoglandular. Estudio observacional a largo plazo. Cir Esp. 2017;95:385–390.