Bariatric surgery is considered a more effective means of achieving weight loss than non-surgical options in morbid obesity. Rates of failure or relapse range from 20% to 30%. The study aims to analyze the influence of psychological variables (self-esteem, social support, coping strategies and personality) in the maintenance of weight loss after bariatric surgery.
MethodsA cohort study was conducted involving 64 patients undergoing bariatric surgery for 24 months. At the end of the follow-up period, patients were divided into 2 sub-cohorts classified as successes or failures. Success or favorable development was considered when the value of percent excess weight loss was 50 or higher.
ResultsNo statistically significant differences were observed between the 2 groups in any variable studied. All patients had high self-esteem (87.3 those who failed and 88.1 those who are successful) and social support (90.2 and 90.9). Patients who succeed presented higher scores for cognitive restructuring (57.1) and were more introverted (47.1), while those who failed scored more highly in desiderative thinking (65.7) and were more prone to aggression (50.7) and neuroticism (51.7).
ConclusionsHigh self-esteem and social support does not guarantee successful treatment. The groups differed in how they coped with obesity but the data obtained do not justify the weight evolution. In the absence of psychopathology, personality trait variability between patients is insufficient to predict the results.
El tratamiento de la obesidad mórbida mediante la cirugía bariátrica es más efectivo que las opciones no quirúrgicas. Las tasas de fracaso o recaída oscilan entre el 20 y el 30%. El estudio pretende analizar la influencia de determinadas variables psicológicas (autoestima, apoyo social, estrategias de afrontamiento y personalidad) en el mantenimiento de la pérdida de peso de los pacientes después de la cirugía bariátrica.
MétodosSe realizó un estudio de cohorte compuesta por 64 pacientes intervenidos mediante cirugía bariátrica con 24 meses de seguimiento. Al final del periodo, los pacientes fueron divididos en 2 subcohortes según fueran éxitos o fracasos. Se consideró éxito o evolución favorable cuando el valor del porcentaje de sobrepeso perdido era 50 o superior.
ResultadosNo se observaron diferencias estadísticamente significativas entre los 2 grupos en ninguna variable estudiada. Todos los pacientes tuvieron alta la autoestima (87,3 los que fracasan y 88,1 los que tienen éxito) y el apoyo social (90,2 frente a 90,9). Los pacientes que tuvieron éxito presentaron puntuaciones más altas para la reestructuración cognitiva (57,1) y eran más introvertidos (47,1); mientras que los que fracasaron anotaron más alto en pensamiento desiderativo (65,7) y eran más propensos a la agresión (50,7) y el neuroticismo (51,7).
ConclusionesUna alta autoestima y un alto apoyo social no garantizan el éxito del tratamiento. Los grupos difieren en la forma en que hicieron frente a la obesidad, pero los datos obtenidos no justifican la evolución del peso. En ausencia de psicopatología, la variación de los rasgos de personalidad entre los grupos de pacientes es insuficiente para predecir los resultados.
Clinically severe or morbid obesity causes health consequences that are much more severe than moderate obesity.1 Its prevalence in developed countries reaches almost 7% (with a 70% increase in the last 15 years) and is rapidly increasing in developing countries.2,3 At present, bariatric surgery is the most effective treatment for morbid obesity.4–8 Surgery generates substantial weight loss in patients, but 20%–30% do not achieve this goal in the long term, which is considered treatment failure.9 Morbid obesity is associated with high levels of psychopathology, including depression, anxiety, eating disorders and pathological personality traits. Psychiatric problems such as alcoholism, bulimia, severe mood disorders and personality disorders are considered contraindications for bariatric surgery because patients with these characteristics are at high risk of presenting psychological and somatic complications after surgery.10,11 The identification of negative predictors after surgery is essential to predict long-term failure as well as possible increased risk for postoperative morbidity and mortality.12 The persistence of possible psychological problems (that are not a surgical contraindication) after surgery may counteract initial weight loss and jeopardize the success of the procedure. In this context, psychological evaluation plays an essential role, not only to reject or approve the patient as a candidate for surgery, but also to identify possible emotional, cognitive, behavioral and social factors that may influence the success or failure of the intervention.13,14
Some studies attribute weight gain to physiological factors,15,16 while others affirm that inadequate coping strategies, personality traits, or the patient's psychological inability to adapt to new lifestyle habits (dietary patterns, physical activity and work), or lack of postoperative follow-up, are generally the source of the failure to maintain weight loss after surgery.17–19 Recent research20 remains inconsistent, but findings indicate that preoperative cognitive function, personality, mental health, and psychological variables related with binge-eating can predict postoperative weight loss, as these factors influence postoperative eating behavior.
The main objective of this study is to detect psychological characteristics or traits associated with poor weight loss results 24 months after surgery.
MethodsThe study population included all morbidly obese patients treated surgically by the Bariatric Surgery Unit at our hospital who met the inclusion criteria from January 2012 to December 2014. The study population coincided with the sample population as it was a consecutive non-randomized sample from the same time period. Sixty-four patients were included, with a precision of 9.8% in the estimation of a proportion using a bilateral normal asymptotic 95% confidence interval, and assuming a failure to treat rate of 20%.9 The inclusion criteria were: a) voluntary acceptance to participate, with the signing of informed consent; b) compliance with local criteria for bariatric surgery, recommended by the Spanish Society of Obesity Surgery (SECO)21; c) evaluation as “competent” by the Mental Health Unit; and d) attendance to scheduled postoperative follow-up office visits in the Surgery Department outpatient clinic for 2 years.
The decision to perform one or the other surgical technique depended mainly on the patient's body mass index (BMI) (if higher than 50kg/m2, we performed laparoscopic vertical sleeve gastrectomy [VSG]), whether the patient had gastroesophageal reflux disease (if GERD, we performed gastric bypass [GB]) and associated co-morbidities (poorly controlled diabetes mellitus led us to GB).
The study design was a single initial cohort of all patients included during the study period. The 24-month assessment of the surgery allowed us to create 2 subcohorts according to the response type: those who evolved favorably and maintained the weight loss achieved (responsive subcohort) and those who did not, with treatment failure (nonresponsive subcohort). The cut-off criterion adopted for this classification was the percentage of excess weight loss (%EWL).22,23 Its value is measured in a standardized manner using the following formula: (initial weight-current weight)/(initial weight-ideal weight, equivalent to a BMI of 25kg/m2)×100. Successful patients were those who achieved a score that was “excellent” (%EWL≥65%) or “good” (%EWL=50%–64%). Patients who failed had achieved a result of less than 50%.
With regard to the protocol, organic clinical data were obtained in the preoperative period and 2 years after surgery, while the psychological variables were only assessed after 24 months, using the following self-administered scales: Rosenberg's Self-Esteem Scale24; MOS Social Support Survey25; coping strategies inventory by Tobin et al. (Spanish adaptation of Cano García et al.)26; Minnesota Multiphasic Personality Inventory-2 Restructured Form (MMPI-2-RF) by Ben-Porath and Telleggen.27
The study was approved by the Central Almeria Research Ethics Committee (Study 69/2013), which is ascribed to the Torrecárdenas Hospital (Almeria) of the Andalusian Public Health Services (Spain).
The clinical variables studied were sex, age, height, waist circumference, hip-to-waist ratio, weight, BMI, %EWL and type of surgical intervention.
The results of the psychological variables were assessed in percentiles (%ile) obtained by the tests utilized. The studied variables were: self-esteem, classified as high (%ile≥75), moderate (%ile 74–55) and low (%ile<55); social support (%ile>80 indicates a high perceived level of social support, %ile 80–57 is a moderate level, and a %ile<57 is low); coping strategies (%ile>50 in the following variables: problem solving, cognitive restructuring, social support and emotional expression indicate adequate coping, while a %ile≥50 in the variables for problem avoidance, wishful thinking, social withdrawal and self-criticism reflect inadequate coping); and personality (%ile≥65) are considered psychopathological levels.
The following is a description of the surgical techniques used:
VSG: The intervention begins with the introduction of the supraumbilical optical trocar and the placement of 4 accessory trocars. The greater curvature of the stomach is dissected with a thermal scalpel, starting about 4cm from the pylorus up to the angle of Hiss. Dissection is performed using an endostapler over a 34F Faucher tube, which is subsequently reinforced with absorbable 2–0 monofilament sutures. The suture line is tested for leaks with methylene blue, the surgical specimen is withdrawn and a suction drain is placed.
GB: The simplified technique is performed, which is carried out entirely in the supramesocolic compartment. The gastric dissection is done over a 34F Faucher tube. The intestinal loop (60cm from the Treitz) is pulled up, and a gastroenteric anastomosis is performed with a linear endostapler. The enteroenteric anastomosis is created 140cm from the anastomosis. Methylene blue is used to check all anastomoses for leaks, and the base of the loop is then dissected. Suction drains are used in all patients. All closures (both buttonholes and mesentery) are performed with 2–0 barbed suture.
Statistical AnalysisThe IBM SPSS Statistics 23.0 statistical package for Windows was used for the analysis. The quantitative variables are expressed as means accompanied by their standard deviation and the qualitative variables as percentages, with their 95% confidence interval, estimated by the usual method. The comparisons of the quantitative variables were made using the Student's t test, with previous evaluation of the homogeneity of variances using the Levene test, or the Mann–Whitney U test if more appropriate, controlling for potential collinearity or confounding effects. Pearson's chi-squared test was used to compare the qualitative variables. Likewise, the odds ratio was applied with 95% confidence intervals for the calculation of significance, with a P value of .05.
ResultsA total of 64 patients were included. During the 24-month follow-up, no patients were lost, which was due in part to their intensive follow-up in this process after surgery. Mean age of the sample was 41.6±8 years. The GB surgical technique was performed in 21 (32.8%) patients, and 43 (67.2%) underwent VSG. During the 24-month follow-up, 22 (34.3%) patients failed (16 women and 6 men) and 42 (65.6%) were successful (28 women and 14 men). The mean age of the successes and failures was 41.6±8 and 41.6±8 years, respectively. There was no statistically significant difference between the two groups regarding age and sex.
95% of the patients treated with GB (n=20) were successful after a 24-month follow-up. As for VSG, 49% (n=21) of patients failed, while the remaining 51% (n=22) were successful.
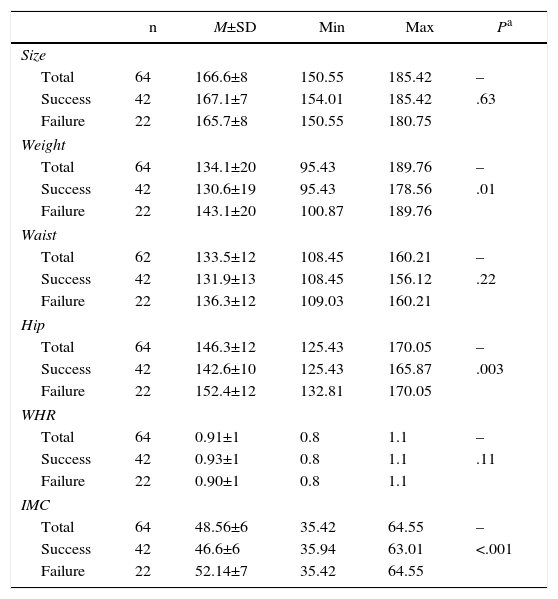
The organic preoperative values presented significant differences between the two groups for the weight, hip and BMI variables, although not in the remainder (height, weight or waist–hip ratio) (Table 1). After 24 months of follow-up, the patients that evolved favorably obtained an average %EWL of 68.3, versus 42.7 of those who failed.
Descriptive and Bivariate Analysis of the Preoperative Organic Variables.
| n | M±SD | Min | Max | Pa | |
|---|---|---|---|---|---|
| Size | |||||
| Total | 64 | 166.6±8 | 150.55 | 185.42 | – |
| Success | 42 | 167.1±7 | 154.01 | 185.42 | .63 |
| Failure | 22 | 165.7±8 | 150.55 | 180.75 | |
| Weight | |||||
| Total | 64 | 134.1±20 | 95.43 | 189.76 | – |
| Success | 42 | 130.6±19 | 95.43 | 178.56 | .01 |
| Failure | 22 | 143.1±20 | 100.87 | 189.76 | |
| Waist | |||||
| Total | 62 | 133.5±12 | 108.45 | 160.21 | – |
| Success | 42 | 131.9±13 | 108.45 | 156.12 | .22 |
| Failure | 22 | 136.3±12 | 109.03 | 160.21 | |
| Hip | |||||
| Total | 64 | 146.3±12 | 125.43 | 170.05 | – |
| Success | 42 | 142.6±10 | 125.43 | 165.87 | .003 |
| Failure | 22 | 152.4±12 | 132.81 | 170.05 | |
| WHR | |||||
| Total | 64 | 0.91±1 | 0.8 | 1.1 | – |
| Success | 42 | 0.93±1 | 0.8 | 1.1 | .11 |
| Failure | 22 | 0.90±1 | 0.8 | 1.1 | |
| IMC | |||||
| Total | 64 | 48.56±6 | 35.42 | 64.55 | – |
| Success | 42 | 46.6±6 | 35.94 | 63.01 | <.001 |
| Failure | 22 | 52.14±7 | 35.42 | 64.55 | |
SD: standard deviation; WHR: waist-to-hip ratio; BMI: body mass index; M: mean; Max: maximum; Min: minimum.
The comparison of the mean scores of the 2 groups for all the psychological variables analyzed did not reveal any statistically significant differences. The mean %ile of the total sample for the self-esteem variable was 87.1±10 (range 99–50). 59% (n=38) obtained high and 41% (n=26) mean. Another 28 patients with high self-esteem (67% of the group) and 14 with medium self-esteem (33%) were successful, resulting in a mean total %ile for the group of 88.1%±11% (range 99–50). Those who failed scored high (45%, n=10) and moderate (56%, n=12) in self-esteem, with a mean %ile of 87.3±10.0 (range 99–70). The mean %ile of the total sample for the social support variable was 90.6±9.9 (range 99–60), in which 47 patients scored high (73%) and 17 scored moderately (27%). Among those who progressed favorably, 32 patients (76%) received high social support and 10 patients (24%) moderate; 15 patients (68%) with high social support failed and 7 (32%) did so with average social support. The mean %ile of the successes was 90.9±9, (range 99–65) versus 90.2±9 (range 99–60) of those who failed.
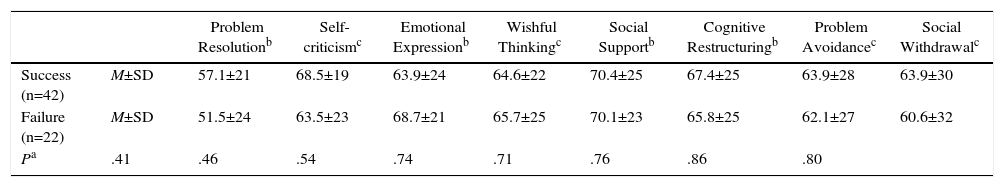
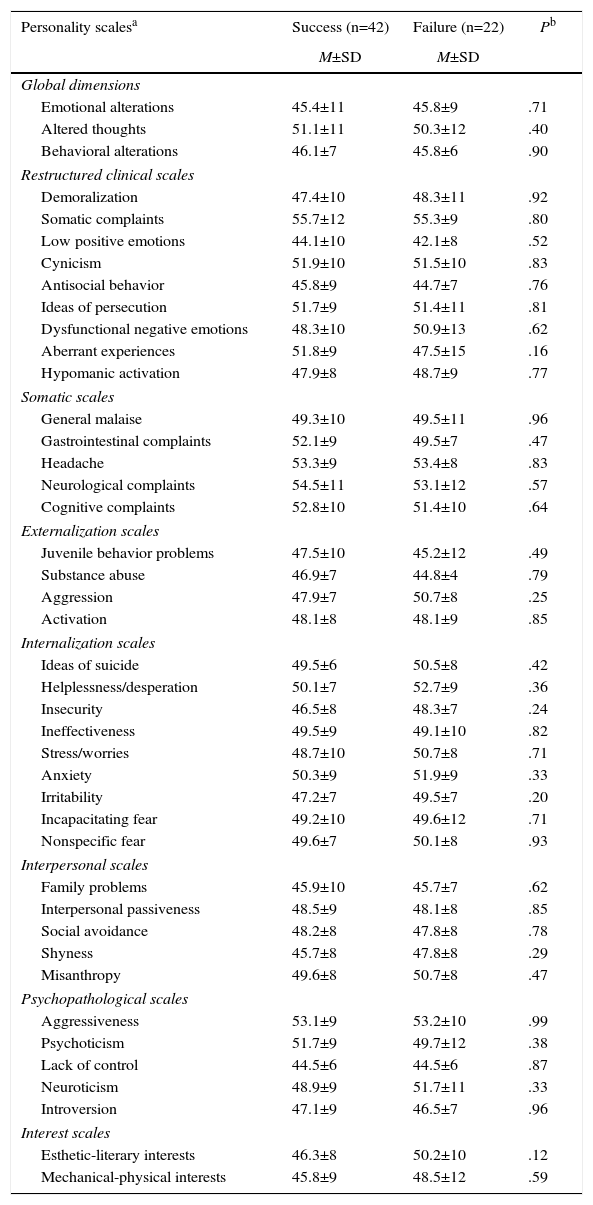
The 2 groups presented differences in the strategies used to cope with the obesity problem. Data from the Inventory of Coping Strategies scale indicated that successful patients presented greater problem solving, self-criticism, social support, cognitive restructuring, avoidance of problems and social withdrawal. Meanwhile, those who failed had more emotional expression and greater wishful thinking than those who succeeded (Table 2). No mean values of psychopathological personality were found in the 5 clinical scales of MMPI-2-RF. The rest of the personality scales were examined in detail, in spite of providing different values, and the differences between the 2 groups were minimal, both in the second order (behavioral, thought and emotional alterations) and in the specific problems and interest scales (Table 3).
Descriptive Bivariate Analysis of the Variable Coping Strategies After 24 Months of Postoperative Evolution.
| Problem Resolutionb | Self-criticismc | Emotional Expressionb | Wishful Thinkingc | Social Supportb | Cognitive Restructuringb | Problem Avoidancec | Social Withdrawalc | ||
|---|---|---|---|---|---|---|---|---|---|
| Success (n=42) | M±SD | 57.1±21 | 68.5±19 | 63.9±24 | 64.6±22 | 70.4±25 | 67.4±25 | 63.9±28 | 63.9±30 |
| Failure (n=22) | M±SD | 51.5±24 | 63.5±23 | 68.7±21 | 65.7±25 | 70.1±23 | 65.8±25 | 62.1±27 | 60.6±32 |
| Pa | .41 | .46 | .54 | .74 | .71 | .76 | .86 | .80 |
SD: standard deviation; M: mean.
Descriptive Analysis of the Personality Variable After 24 Months of Postoperative Progress.
| Personality scalesa | Success (n=42) | Failure (n=22) | Pb |
|---|---|---|---|
| M±SD | M±SD | ||
| Global dimensions | |||
| Emotional alterations | 45.4±11 | 45.8±9 | .71 |
| Altered thoughts | 51.1±11 | 50.3±12 | .40 |
| Behavioral alterations | 46.1±7 | 45.8±6 | .90 |
| Restructured clinical scales | |||
| Demoralization | 47.4±10 | 48.3±11 | .92 |
| Somatic complaints | 55.7±12 | 55.3±9 | .80 |
| Low positive emotions | 44.1±10 | 42.1±8 | .52 |
| Cynicism | 51.9±10 | 51.5±10 | .83 |
| Antisocial behavior | 45.8±9 | 44.7±7 | .76 |
| Ideas of persecution | 51.7±9 | 51.4±11 | .81 |
| Dysfunctional negative emotions | 48.3±10 | 50.9±13 | .62 |
| Aberrant experiences | 51.8±9 | 47.5±15 | .16 |
| Hypomanic activation | 47.9±8 | 48.7±9 | .77 |
| Somatic scales | |||
| General malaise | 49.3±10 | 49.5±11 | .96 |
| Gastrointestinal complaints | 52.1±9 | 49.5±7 | .47 |
| Headache | 53.3±9 | 53.4±8 | .83 |
| Neurological complaints | 54.5±11 | 53.1±12 | .57 |
| Cognitive complaints | 52.8±10 | 51.4±10 | .64 |
| Externalization scales | |||
| Juvenile behavior problems | 47.5±10 | 45.2±12 | .49 |
| Substance abuse | 46.9±7 | 44.8±4 | .79 |
| Aggression | 47.9±7 | 50.7±8 | .25 |
| Activation | 48.1±8 | 48.1±9 | .85 |
| Internalization scales | |||
| Ideas of suicide | 49.5±6 | 50.5±8 | .42 |
| Helplessness/desperation | 50.1±7 | 52.7±9 | .36 |
| Insecurity | 46.5±8 | 48.3±7 | .24 |
| Ineffectiveness | 49.5±9 | 49.1±10 | .82 |
| Stress/worries | 48.7±10 | 50.7±8 | .71 |
| Anxiety | 50.3±9 | 51.9±9 | .33 |
| Irritability | 47.2±7 | 49.5±7 | .20 |
| Incapacitating fear | 49.2±10 | 49.6±12 | .71 |
| Nonspecific fear | 49.6±7 | 50.1±8 | .93 |
| Interpersonal scales | |||
| Family problems | 45.9±10 | 45.7±7 | .62 |
| Interpersonal passiveness | 48.5±9 | 48.1±8 | .85 |
| Social avoidance | 48.2±8 | 47.8±8 | .78 |
| Shyness | 45.7±8 | 47.8±8 | .29 |
| Misanthropy | 49.6±8 | 50.7±8 | .47 |
| Psychopathological scales | |||
| Aggressiveness | 53.1±9 | 53.2±10 | .99 |
| Psychoticism | 51.7±9 | 49.7±12 | .38 |
| Lack of control | 44.5±6 | 44.5±6 | .87 |
| Neuroticism | 48.9±9 | 51.7±11 | .33 |
| Introversion | 47.1±9 | 46.5±7 | .96 |
| Interest scales | |||
| Esthetic-literary interests | 46.3±8 | 50.2±10 | .12 |
| Mechanical-physical interests | 45.8±9 | 48.5±12 | .59 |
SD: standard deviation; M: mean.
The results of the study largely coincide with current literature, where information is limited and contradictory in many cases because most research indicates isolated variables that do not provide clear and determinant predictors.19,20,28,29
The average levels obtained in self-esteem and social support in the 2 response groups are elevated and quite similar. However, the prevalence of patients with high values among those who were successful was higher than among those who failed in both variables (91% vs 82% in self-esteem and 76% in social support), which seems to suggest that at higher values, the greater the probability of success. A recent study30 on self-esteem evaluated weight loss one and two years after surgery and concluded that self-esteem improved significantly during the second year. However, other research31 indicates that it is not affected by surgery, or that it remains stable during the postoperative period, so it is not related to weight loss. The study of social function after bariatric surgery is important because its absence is considered a risk factor. Some authors32,33 have observed that having friends or family support for the treatment of weight loss improves short- and long-term outcomes.
The use of appropriate coping strategies for problems was greater in patients who evolved favorably than in patients who failed (52% vs 42%), both in problem-based management (problem-solving and cognitive restructuring, 50% vs 40%), as well as in appropriate emotion-based management (social support and emotional expression, 71% vs 63%). Faced with the decision of undergoing surgery and facing their illness with the intention of maintaining weight reduction, do patients consider their coping in a different way? Or after surgery do they continue to use the same strategies used previously, resistant to morbid obesity? Although the results obtained do not provide statistically significant data, we observed that focusing the new situation differently than what patients did in the preoperative stage has been able to influence, and even modify, the postoperative process and favor patient evolution.34 Some authors31 indicate that instrumental support and emotion-based strategies are positive predictors after 6 months of evolution, albeit moderate.
Recent studies35 indicate that personality traits play an important role in both the development and evolution of obesity, in which self-awareness (internal appetite regulator) and self-control behaviors act as protective factors. Risk factors include neurosis, impulsiveness and sensitivity to positive reinforcement. However, the study of the influence of personality (pathological or not) on morbid obesity and, specifically, on its correlation with progress after bariatric surgery, is limited and ambivalent at the present time. Most studies propose inconsistent and even contradictory predictors for weight maintenance in both the short and long term.36–38 In our study, although we did not obtain means that indicated psychopathology in any of the groups, we did observe more pronounced personality traits in one group over the other. Compared with those who succeeded, the group of patients who failed scored higher in aggressiveness, irritability, hopelessness, insecurity, and neurosis, which may be potential risk factors for failure. A recent study39 contrasts with this latter result and concludes that the neuroticism factor correlates with more than 5% of the success of the treatment. Another important study40 states that neuroticism levels are more elevated in obese patients treated with surgery than in obese patients who were not and in non-obese subjects, although the authors did not explain whether it favors success or failure after the surgical intervention.
The cohort study has ensured the inclusion of all patients who had undergone surgery and were followed up in the outpatient surgery consultation by offering them the possibility to participate. However, the limited number of annual operations and the fact that postoperative outpatient follow-up only lasts a short period of time (maximum 24 months), which some patients do not comply with, mean that the possibility to lose patients in the study increases over time. In order to minimize this, surgically treated patients should be included from a period of no more than 3 years. The result is a small sample that, along with the short study period, has limited both the analysis and the obtaining of statistically significant results.
When the results were assessed according to the surgical technique used, the analysis for each was considered separately. However, the resulting sample size (21 GB and 43 VSG) was not able to obtain statistically solid results, so the small sample size has hindered reaching conclusions
It is necessary to consider that, in order to undergo surgical treatment, all the patients studied had been considered psychologically “fit”, meaning that they started out in a state of mental “stability” before surgery. In order to carry out the study, the same variables described in the preoperative evaluation were used, which enabled us to assess both the psychological evolution of the patients after surgery as well as the influence of these variables on the outcome after 24 months of follow-up. The overall results indicated that all patients had obtained mean values that were “not inferior” to those before the intervention in all variables, preoperative psychological stability was maintained, and differences were only detected in the psychological traits between the 2 response groups. Although they did not provide specific measurements, the preoperative psychological reports indicated the presence of medium-high levels of self-esteem and social support, adequate coping strategies and absence of any type of psychiatric disorder (including personality). However, these evaluations could not be used as prior measurements since they were done at very different times (most patients were on a surgical waiting list for 2–5 years) and by different mental health professionals, thereby avoiding information bias. This has generated an important limitation since no preoperative measurements were available, which has prevented completing inferential analysis 24 months after the operation.
Nonetheless, this aspect has not prevented us from evaluating the psychological evolution of patients as a function of these variables, along with its influence on results, since the psychological constructs studied represent continuous dimensions that share similar characteristics: consistency and little variation for change in the short and mid-term. These are “psychological traits” that allow us to describe behavior trends that are relatively consistent and stable over time,41 which presupposes minimal changes in the psychological characteristics of patients after surgery. Therefore, if we consider that the differences found in both groups already existed before surgery, we could assess the psychological characteristics of those who fail as possible “risk factors” that predict poor postoperative evolution. Recognizing this fact would allow us to identify these traits previously in order to apply a specific, scheduled psychological treatment in these patients after surgery, which would avoid a poor response.
We can conclude that the psychological variables studied do not explain the success or failure of treatment. Despite not being clear and consistent predictors, the differences observed in patients’ ways of dealing with problems, like the variation of their personality traits, indicate the presence of different psychological characteristics among patients according to the weight loss obtained. High self-esteem and adequate social support do not guarantee treatment success. In order to obtain more solid conclusions, future studies are necessary with a larger number of patients and longer prospective evaluation and follow-up.
Conflict of InterestsThe authors have no conflicts of interest to declare.
Please cite this article as: Rodríguez-Hurtado J, Ferrer-Márquez M, Fontalba-Navas A, García-Torrecillas JM, Olvera-Porcel MC. Influencia de variables psicológicas en pacientes obesos mórbidos operados con cirugía bariátrica tras 24 meses de evolución. Cir Esp. 2017;95:378–384.