Traumatic thoracic duct (TD) injury is an uncommon complication of cervical lymph node dissection for the treatment of thyroid cancer, and its incidence is about 2%. Although the most serious complications appear when this lesion occurs in the thorax, typically during esophagectomy, cervical lesions also have associated postoperative morbidity, including nutritional complications (malnutrition, hypoproteinemia, hyponatremia and dehydration), immunosuppression and extension to the thorax in the form of chylothorax.1
The TD is the largest lymphatic vessel of the body; it collects lymph from almost all the subdiaphragmatic areas, the posterolateral wall of the thorax and several terminal collectors at the base of the neck. It usually originates at the T12-L1 vertebrae, where a dilated sac known as the cisterna chyli can appear. After ascending through the mediastinum, it reaches the base of the neck, where it finally curves before emptying into the internal jugular vein (46%), the junction of the subclavian and jugular veins (32%) or the subclavian vein (18%).2
We present the case of a 47-year-old patient diagnosed with papillary thyroid carcinoma and left level III lymph node involvement. Total thyroidectomy was performed with lymph node dissection of the bilateral central compartment and modified left radical lymphadenectomy. On the first day post-op, the patient presented a high volume of discharge through the surgical drain tube (550ml) that was chylous in appearance. As a TD fistula was suspected, triglyceride levels were determined in the drained fluid, which was 147mg/dL and confirmed the diagnosis.3
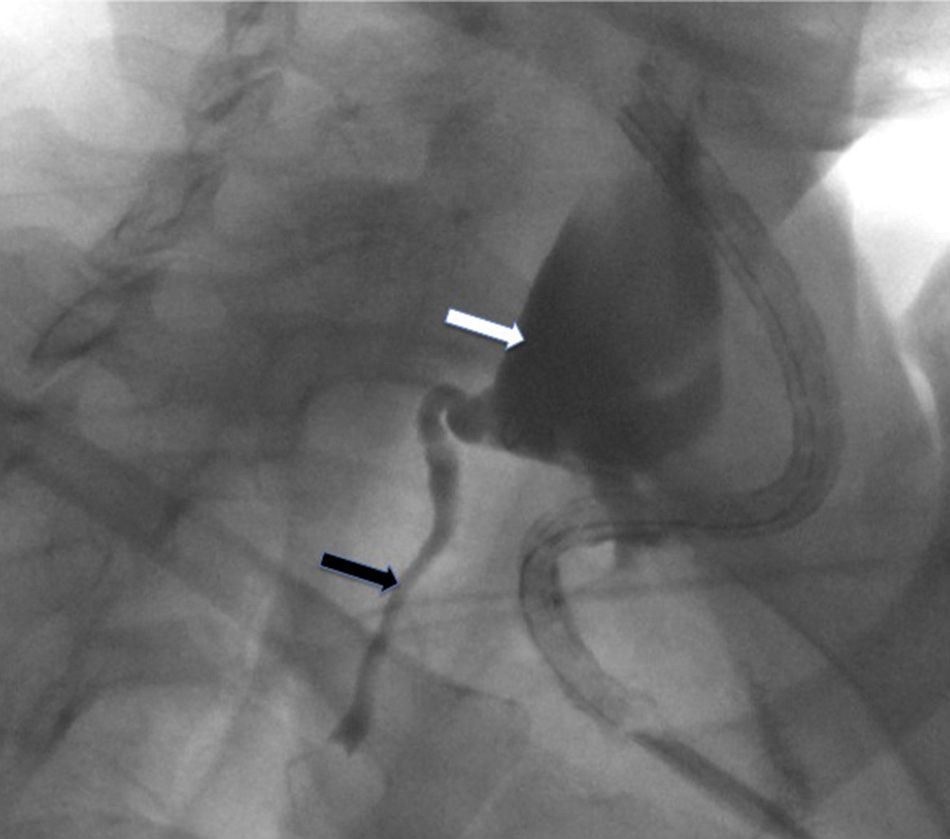
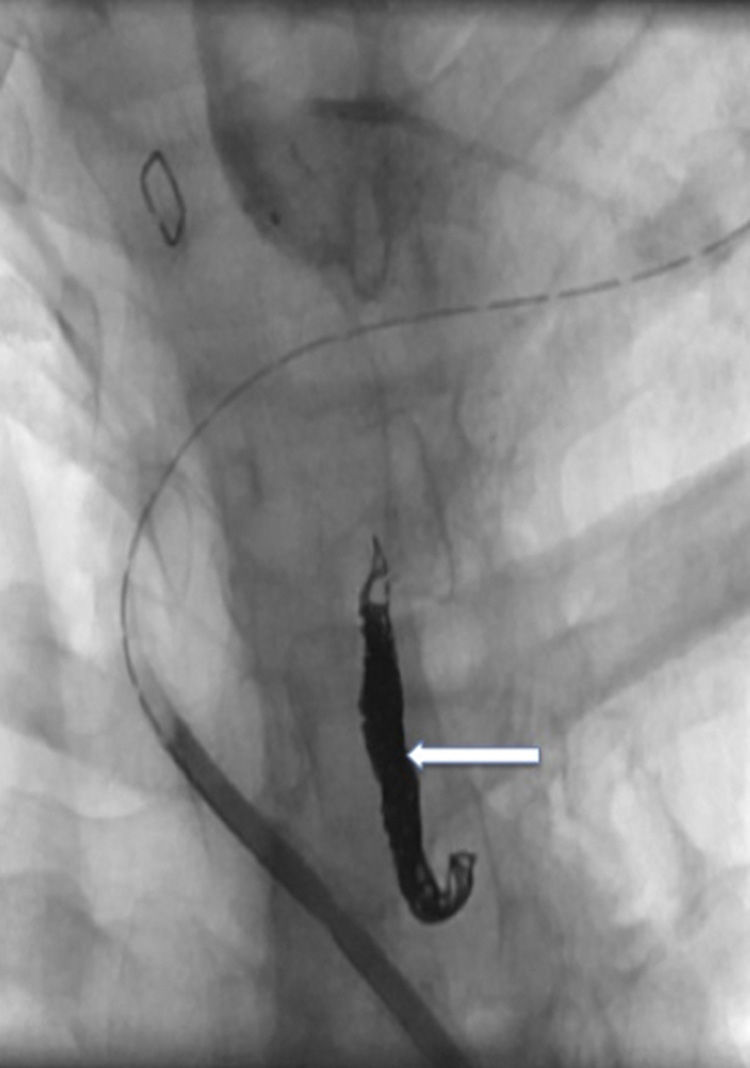
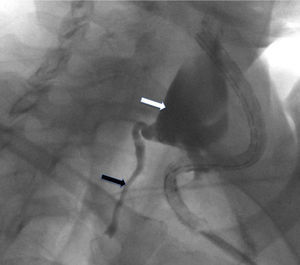
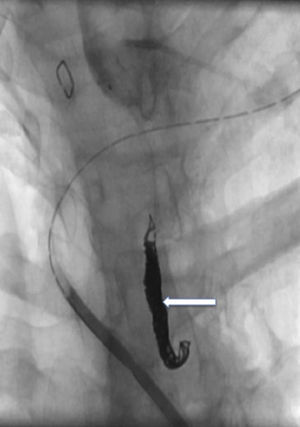
Initial treatment was conservative, with low-fat enteral nutrition, medium-chain triglyceride supplements, octreotide (0.1mg/8h, subcutaneous) and antibiotics. In spite of these measures, the discharge through the drain persisted at a volume of about 300ml/day. Therefore, we decided to perform thoracic duct embolization to definitively treat the fistula. The first attempt used a pedal lymphography approach to try to identify the cisterna chyli for percutaneous catheterization. During the procedure, we did not identify any dilatations that were suitable for percutaneous access, and the size of the TD was uniform. It was then decided to use a cervical percutaneous approach. Iodine contrast was injected into the surgical drain, which filled the cavity created by the lymphocele and allowed us to identify the site of the TD leak. Using percutaneous puncture, a macrocatheter (Progreat®, 2.7/2.9 France, Terumo®) was introduced at the cervical level, directed by a 0.021″ guide through the TD orifice. In this manner, lymphography was done (Fig. 1) along with embolization using microcoils (Axium® 0.018″, eV3) and N-butyl-2-cyanoacrylate (Gluebrand 2®-Gem) (Fig. 2). The following day, no discharge was seen through the drain tube. The drain was removed and the patient was discharged from the hospital after having started a normal diet.
Although there is no consensus about the standard treatment for this type of lesions, most authors recommend an initial conservative treatment, which usually consists of a low-fat diet with medium-chain triglyceride supplements and somatostatin analogs.4 Nonetheless, there are cases in which the high discharge volume (>1000ml/day) or the persistence of the fistula for more than 5–7 days indicate the need for more aggressive treatment in order to prevent the appearance of complications.5 In these cases, the objective is closure of the TD. There are several options, such as TD embolization, the use of sclerosing substances or biological glues, or the surgical closure of the TD (cervical as well as thoracic), where the use of video-assisted thoracoscopy techniques is especially useful.
Embolization of the TD was originally described by Cope et al.,6 who used a transabdominal percutaneous approach to access the cisterna chyli after its previous identification with iodine-contrast pedal lymphography. Although this is currently the most widely used technique, modifications have arisen to access the TD. One approach that stands out is the intranodal lymphangiography technique recently described by Rajebi et al.,7 which demonstrates practical importance. In expert groups,8 TD catheterization is achieved in 67% of patients, in whom the embolization success rate is close to 90%. Long-term complications after this technique appear in 14.3% of patients, the most frequent of which are chronic diarrhea and edema of the lower extremities.9
In our case, the transcervical retrograde approach of the TD enabled us to locate the lesion and treat it satisfactorily. To our knowledge, there are no previously published reports of this approach in the literature, and we therefore contribute a new technique for treating this type of situations.
FundingThe authors declare that they have received no funding.
Conflict of InterestsThe authors declare that they have no conflict of interests.
We want to thank Dr. Eduardo Larrañaga Barrera for providing his experience toward the management of this case.
Please cite this article as: Muñoz de Nova JL, Friera Reyes A, Cuesta Pérez JJ, Rodríguez Sánchez A, Bravo Lifante JM. Acceso percutáneo de las fístulas cervicales del conducto torácico: un nuevo abordaje. Cir Esp. 2015;93:195–197.