Trans Oral Endoscopic Thyroidectomy through Vestibular Approach (TOETVA) allows access to the thyroid with the best cosmetic results as there are no visible scars.
MethodsHere we present a prospective observational study of 53 patients which underwent TOETVA from July 2017 to June 2021.
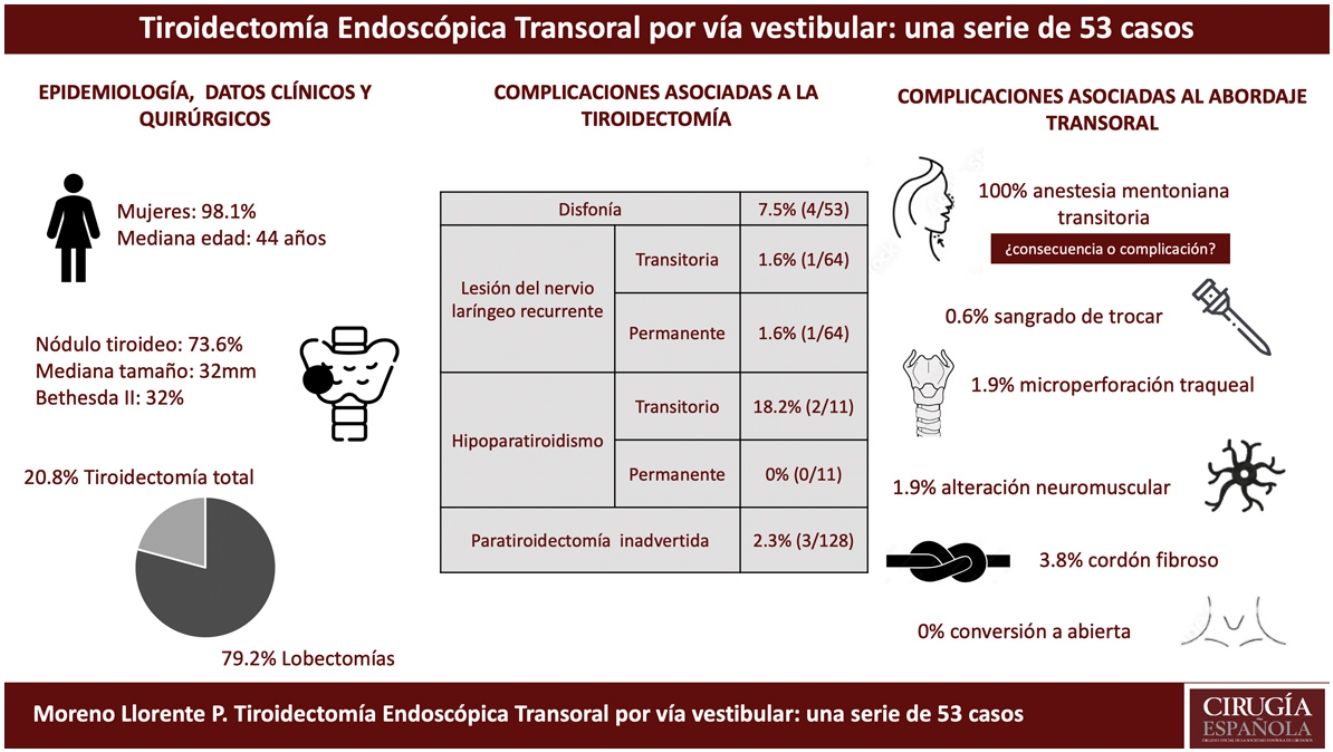
ResultsFifty-two cases (98.1%) cases were women (median age 44 years old). Thyroid nodule was the main surgical indication accounting 73.6% of cases. We performed 42 lobectomies and 11 total thyroidectomies; 4 left Central Neck Dissection (CND) were also associated. The median surgical time for port placement was 14 min and for lobectomy, total thyroidectomy and left CND were 80, 140 and 30 min, respectively. The median of hospital stay was 2 days. Dysphonia was present in 4 patients; however, laryngoscopy only confirmed laryngeal nerve impairment in 2 cases, one of them classified as permanent (1.6%). In those patients that underwent total thyroidectomy, the rate of transient hypoparathyroidism was 18.2% whereas permanent was 0%. Regarding complications associated to the new approach, transient chin numbness appeared in all patients with a variable degree of intensity.
ConclustionsTransoral surgery is a recent approach in our Unit. Our results, based on the first 53 patients, show that it is a safe and effective approach when performed in appropriately selected patients offering the best cosmetic result. Besides, new complications associated to the approach has been shown to be transient.
La Tiroidectomía Endoscópica Transoral por vía vestibular (TOETVA) permite el acceso al tiroides sin cicatrices visibles y con el mejor resultado cosmético posible.
MétodosEstudio observacional prospectivo de 53 pacientes sometidos a tiroidectomía endoscópica transoral desde julio de 2017 hasta junio de 2021.
ResultadosCincuenta y dos casos (98.1%) fueron mujeres con una mediana de edad de 44 años. El nódulo tiroideo fue la indicación quirúrgica más frecuente (73.6%). Se realizaron 42 lobectomías,11 tiroidectomías totales y en 4 casos se asoció vaciamiento ganglionar del compartimento central izquierdo (VGCCI). La mediana de tiempo para la colocación de trocares fue de 14 minutos y para la lobectomía, tiroidectomía total y VGCCI de 80, 140 y 30 minutos respectivamente. La mediana de estancia hospitalaria fue de 2 días. Cuatro pacientes presentaron disfonía (7.5%) pero la laringoscopia sólo confirmó lesión del recurrente en 2 casos, una de ellas permanente (1.6%). En los pacientes con tiroidectomía total la frecuencia de hipoparatiroidismo transitorio fue de 18.2% y el permanente de 0%. Dentro de las complicaciones asociadas al abordaje, en todos los pacientes se presentó anestesia de la región mentoniana transitoria y de intensidad variable.
ConclusionesLa cirugía transoral es un abordaje de aplicación reciente en nuestra unidad. Los resultados en nuestros primeros pacientes muestran que es un abordaje eficaz y seguro cuando se realiza en pacientes bien seleccionados, con el mejor resultado cosmético y con complicaciones nuevas, asociadas al abordaje, transitorias en nuestra serie.
The cervical incision described by Köcher1 is the standard approach to thyroidectomy2. In recent years, new approaches have been proposed to minimize visible scars3–6, but they generally involve greater dissection of anatomical planes to access the thyroid and, in many cases, do so only unilaterally.
Recently, natural orifice surgery has been used to approach the thyroid through the oral cavity7,8, initially with a sublingual access9,10, although with unsatisfactory results. Later, the vestibular approach11,12 provided good results, and its use has been more widespread.
Transoral endoscopic thyroidectomy via the vestibular approach (TOETVA) provides the most direct, bilateral remote access to the thyroid, with no visible incisions13 and the best cosmetic results14. TOETVA as we now know it was first introduced by Anuwong in 201513. The technique was developed primarily in Asia, where, for cultural reasons, cervical scars are a stigma. Although it was rapidly adopted in the West, its growth has been at a slower pace since the demand for this procedure is exclusively due to cosmetic and not cultural reasons.
We present the results of our first TOETVA cases.
MethodsWe conducted a prospective, observational study of 53 patients who underwent TOETVA from July 2017 to June 2021 at 2 referral hospitals, performed by 2 senior endocrine surgeons.
All patients who met the inclusion criteria (Table 1) were explained the details of the procedure, signed a specific informed consent form, informed of the novelty of the approach and the order number that they represented in this series, and authorized the publication of images and data related to the surgical procedure in scientific journals and medical conferences. In accordance with the Ethics Committee of our hospital, and in compliance with the Spanish Protection of Personal Data Law (LOPD 3/2018), a high degree of confidentiality was ensured.
TOETVA inclusion and exclusion criteria.
| Inclusion criteria |
|---|
| Clinical |
| No previous cervical surgery or cervical radiotherapy |
| Bethesda II-IV: ≤4 cm |
| Bethesda V and VI: ≤2 cm15, mobile vocal cords, no signs of locoregional invasion |
| Hyperthyroidism (Graves-Basedow disease) |
| No hypothyroidism (Hashimoto thyroiditis) no active thyroiditis |
| Ultrasound |
| Size of thyroid lobe ≤10 cm (craniocaudal) |
| Thyroid nodule ≤4 cm |
| Thyroid volume ≤ 30 cc |
| Exclusion criteria |
| Upper pole |
| Very voluminous |
| Large cranial prolongation |
| Lower pole |
| Endothoracic extension |
| Locally advanced thyroid cancer |
| Suspicion of extrathyroid extension |
| Presence of lateral cervical lymphadenopathies |
Relative indication, determined by the experience of the surgeon.
We performed the surgery under general anesthesia and orotracheal intubation, which allows the laryngeal nerve to be monitored with conventional orotracheal devices. Generally, a 10 mm 30° scope is used with 5 mm forceps and ultrasonic devices for
PlacementThe patient is placed in the supine position with slight hyperextension of the neck. The surgeon stands at the head of the patient with the screen in front of him, the assistant on the side of the lobectomy, and the surgical nurse on the opposite side.
Asepsis and antibiotic prophylaxisThe oral cavity was decontaminated with non-alcoholic chlorhexidine, and amoxicillin-clavulanate was administered as prophylaxis (2 g during induction and 1 g/8 h on the first postoperative day).
Incisions/initial dissectionFor the 10 mm trocar, a horizontal incision measuring approximately 2 cm is made on the midline, 0.5–1 cm below the lip and approximately 5 mm above the labial frenulum. For the 2 lateral trocars, the incision is vertical and approximately 5 mm. Through the incisions, a solution of epinephrine and saline solution (1 mg/500 mL) is injected with a Veress needle under the platysma, in the anterior cervical region, between the sternocleidomastoid muscles and up to the sternal notch. Subsequently, blunt subplatysmal dissection is performed. Once the trocars are in place, CO2 is insufflated at a maximum pressure of 6 mmHg and a flow of 15 L/min. We placed a traction suture at the level of the cricoid cartilage to lift the flap and improve visibility.
Thyroid dissectionOnce the prethyroid muscles have been separated on the midline, the thyroid lobe is mobilized, and the isthmus is divided. Thyroidectomy is performed in a craniocaudal direction, beginning with the sealing and division of the vessels of the upper pole of the thyroid which, once released, is moved medially and caudally to identify the superior parathyroid gland and recurrent nerve. In all patients, we monitored the recurrent nerve intraoperatively.
Extraction/closureOnce the thyroidectomy is complete, the specimen is placed in a bag and extracted through the 10 mm trocar orifice. Subsequently, the prethyroid muscles are approximated, and the access orifices are closed with interrupted sutures of absorbable material, 5 mm in one plane and 10 mm in 2.
Postoperative managementOral intake of liquids is initiated the same day of surgery. On the first postoperative day, the submandibular compression bandage is removed. In all patients who presented dysphonia, laryngoscopy was performed in the first postoperative week to rule out injury to the vocal cords. Minimum patient follow-up was 2 months.
Study variablesClinical-epidemiological:
- •
Sex
- •
Age
- •
Diagnosis
- •
Nodule size (mm)
- •
Hospital stay (days)
Surgical:
- •
Resection type: lobectomy, total thyroidectomy and/or left central neck dissection (LCND)
- •
Surgical time (min):
▪Trocar placement
▪Lobectomy
▪Extraction of the specimen
Thyroidectomy complications:
- •
Dysphonia: subjective sensation of voice change
- •
Recurrent nerve injury: total or partial alteration of the mobility of the vocal cord observed by laryngoscopy, considered permanent if persisting more than 6 months16.
- •
Bleeding
- •
Infection
- •
Inadvertent parathyroidectomy: reported by the pathology study
- •
Hypoparathyroidism: need for treatment with calcium and/or vitamin D, considered permanent if required for more than 12 months17.
Approach complications:
- •
Permanent mental nerve anesthesia
- •
Neuromuscular alteration: asymmetry of the lips and corner of the mouth due to inflammation of the marginal branch of the 5th cranial nerve
- •
Trocar bleeding
- •
Subcutaneous edema
- •
Tracheal microperforation
- •
Fibrous cervical band: limits hyperextension of the neck
Quantitative variables are expressed as the median and interquartile range. Qualitative variables are provided with the number of subjects and the percentage they represent.
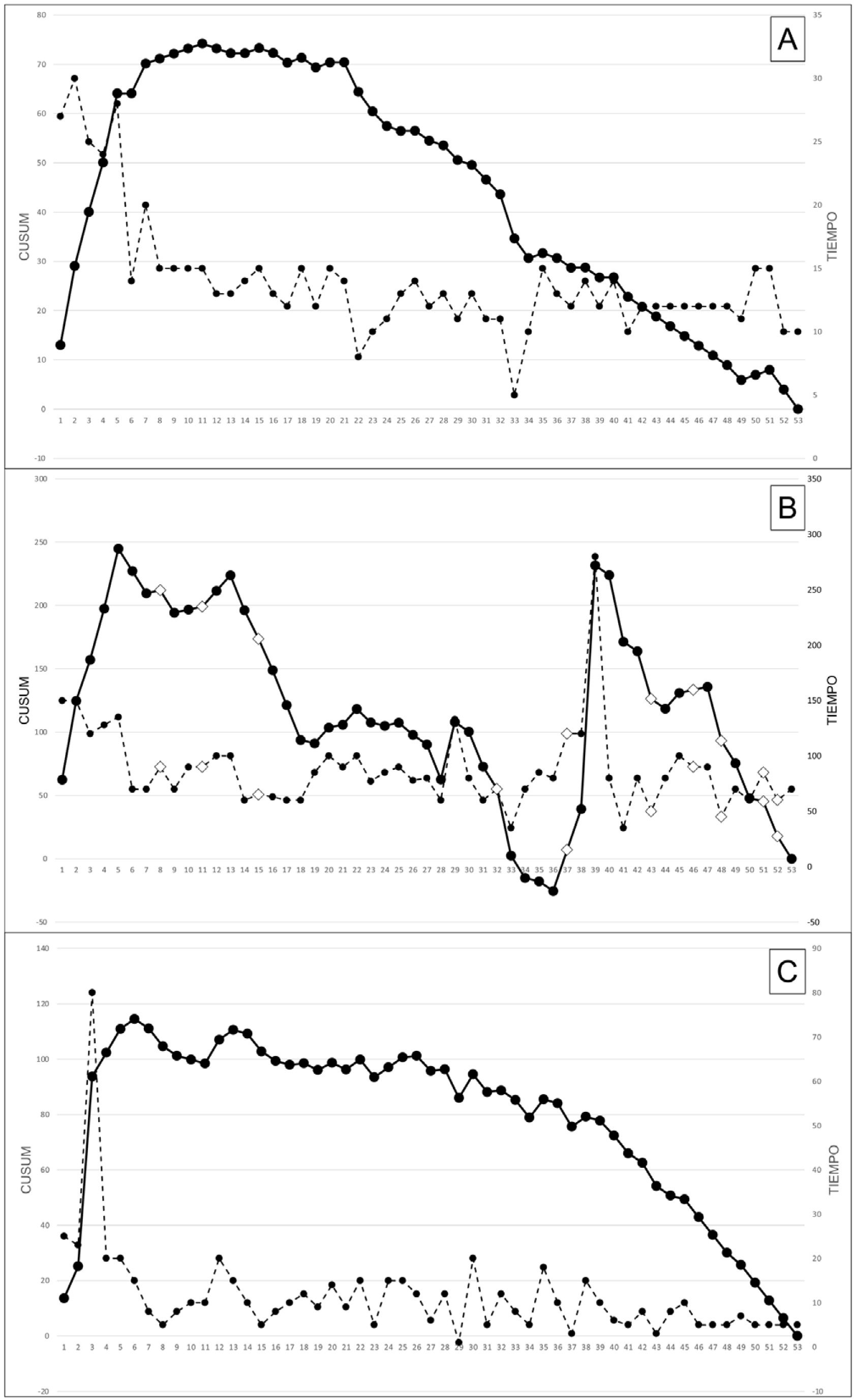
We analyzed the cumulative sums (CUSUM) of the surgical time as a reflection of the learning curve for the technique. Surgical time was divided into 3 stages: trocar placement time, time to complete lobectomy, and time to extract the specimen. In patients undergoing total thyroidectomy, we only considered the time to complete the first lobectomy, which determined the surgical indication. The graphical representation of the CUSUM curves represents the learning curve18. Each case is assigned a value determined by the difference between the time of said case versus the series average, added to the value of the immediately previous case. The ascending slope indicates that the learning of the technique is progressing; when it flattens, this indicates that said learning has been achieved; when it descends, this is the stage when the technique is perfected.
ResultsFifty-three patients with a median age of 44 years (38−50) were analyzed, 52 of whom (98.1%) were women; the median size of the thyroid lesion was 32 mm (16−38). The most frequent indication was thyroid nodule (39 cases; 73.6%), most of which were benign lesions (Bethesda II).
We performed 42 lobectomies (79.2%) and 11 total thyroidectomies (20.8%). Associated LCND was carried out in 4 cases (7.5%), only one in the context of a total thyroidectomy. A median of 14 min (12−15) was used for trocar placement, with a median duration of 80 min (65−100) for lobectomies, and 140 min (125−173) for total thyroidectomy. Median LCND time was 30 min (20−30). Mean specimen extraction time was 10 min (6−15). The hospital stay was 2 days (1−2) (Table 2). The median follow-up was 33.3 months (23.5–40.2).
Epidemiology, clinical surgical and pathological data.
| Epidemiology and clinical data | |
|---|---|
| Age (years), median (IQR) | 44 (38−50) |
| Female sex, n (%) | 52 (98.1) |
| Size of nodule (mm), median (IQR) | 32 (16−38) |
| Surgical indication | |
|---|---|
| Thyroid nodule, n (%) | 39 (73.6) |
| Multinodular goiter, n (%) | 10 (18.9) |
| Hyperthyroidism (toxic nodule), n (%) | 4 (7.5) |
| Cytology, n (%) | FNA | Definitive malignant histology |
|---|---|---|
| Bethesda I | 3 (5.6) | 2 (66.6) |
| Bethesda II | 17 (32) | 1 (5.8) |
| Bethesda III | 5 (9.4) | 3 (60) |
| Bethesda IV | 9 (17) | 3 (33.3) |
| Bethesda V | 3 (5.6) | 3 (100) |
| Bethesda VI | 8 (15) | 8 (100) |
| Surgical data | |
|---|---|
| Lobectomy, n (%) | 42 (79.2) |
| Total thyroidectomy, n (%) | 11 (20.8) |
| LCND, n (%) | 4 (7.5) |
| Trocar placement time (min), median (IQR) | 14 (12−15) |
| Surgical time for partial lobectomy (min), median (IQR) | 80 (65−100) |
| Surgical time for total thyroidectomy (min), median (IQR) | 140 (125−173) |
| LCND time (min), median (IQR) | 30 (20−30) |
| Specimen extraction time (min), median (IQR) | 10 (6−15) |
| Hospital stay (days), median (IQR) | 2 (1−2) |
FNA: fine-needle aspiration; IQR: interquartile range; LCND: left central neck dissection.
Fig. 1 shows the CUSUM and the respective surgical times. Note in the figure that the trocar placement from case 7 onward reached a plateau (learning curve completed), and the descent began starting at case 21 (improvement). For the extraction of the piece, the plateau was reached at case 5, with a slowly descending slope that is accentuated from case 35 onward. The lobectomy time curve shows an initial learning phase that reached the plateau again in case 5, descending from case 13 on. However, starting at case 36 there is a second stage of upward slope, indicating a new learning phase.
Regarding the morbidity of our series, the intrinsic complications entailed in a thyroidectomy and those associated with the transoral approach are presented separately (Table 3).
Postoperative morbidity.
| Morbidity associated with thyroidectomy | |
|---|---|
| Recurrent laryngeal nerve lesion (nar = 64) | |
| Dysphonia | 7.5% (4/53) |
| Transient | 1.6% (1/64) |
| Permanent | 1.6% (1/64) |
| Bleeding | |
| Hematoma, subcutaneous | 1.9% (1/53) |
| Hematoma, deep | 1.9% (1/53) |
| Hematoma, suffocating | 0% (0/53) |
| Would infection | 0% (0/53) |
| Hypoparathyroidism | |
| Transient | 18.2% (2/11) |
| Permanent | 0% (0/11) |
| Parathyroid glands in the specimen (par = 128) | 2.3% (3/128) |
| Hospital readmission | 0% (0/53) |
| Morbidity related with the transoral approach | |
| Transient palsy of the mental region | 100% (53/53) |
| Trocar bleeding | 0.6% (1/159) |
| Microperforation of the trachea | 1.9% (1/53) |
| Cervical fibrous band | 3.8% (2/53) |
| Conversion to open surgery | 0% (0/53) |
nar: nerves at risk; par: parathyroid glands at risk.
Sixty-two of the 64 nerves at risk were identified, and there was no loss of signal during neuromonitoring. In 2 of the 4 patients (7.5%) who presented dysphonia during the immediate postoperative period, laryngoscopy confirmed vocal cord hypomobility: one patient recovered spontaneously one month after surgery, while in the other this condition persisted for 6 months. The frequency of permanent recurrent lesion is 1.6%.
Only 2 of the 11 patients who underwent total thyroidectomy needed calcium temporarily (18.2%).
The frequency of inadvertent parathyroidectomy was 2.3% (3/128 glands at risk), 2 of which were resected in the same patient who underwent total thyroidectomy with LCND.
There were no surgical site infections, hospital readmissions, or conversions to open surgery. There was one subcutaneous hematoma (1.9%) secondary to trocar bleeding (Fig. 2), one deep hematoma (thyroid bed) (1.9%) and none suffocating. One patient also presented a tracheal microperforation (1.9%), which resolved spontaneously and required prolonged antibiotic treatment.
Regarding the morbidity associated with the new approach, 100% of the patients manifested transient anesthesia of the mental region of varying intensity. The midline of the lower lip and the tip of the chin were the last areas to recover, between 6 and 12 months later (Fig. 3).
DiscussionWith the implementation of endoscopic and robotic surgery, new thyroid approaches have appeared in recent years: cervical, anterior thoracic, axillary, mammary, axillary-breast, retroauricular and transoral14. Of all the above, only the TOETVA avoids a visible scar, as it is performed through a natural orifice.
The number of cases in the transoral surgery series published in the literature is highly variable (from 5 to 260 cases)13,19–27. This is probably due to the difficulty of finding suitable patients that meet the strict inclusion criteria and the low demand for this approach in Western countries, as cervical scars are not considered a stigma.
Most of our patients were women (98.1%) with a median age of 44 years, which is similar to other publications (88.5%–96% women)13,19–27, with mean ages of 35–41.36 years13,19,20,22. This is due to the high prevalence of thyroid disease in women and, likely, their greater interest in cosmetic results after surgery.
The thyroid nodule was the most frequent indication (73.6%), and the median size (32 mm) was slightly smaller than reports by other authors (54 mm13 and 41 mm22). This would be explained by the high frequency of Bethesda IV, V, and VI cases (37.6%) and because we follow the recommendation to exclude malignant tumors larger than 20 mm to avoid capsule disruption and loss of diagnostic sensitivity.28
Unlike other authors20,22, we initially considered Graves-Basedow disease a relative contraindication, assuming that these cases are more technically difficult, especially due to the risk of bleeding. Similarly, we believe that patients with thyroid cancer and/or lesions in the context of thyroiditis should be included progressively as we increase our experience with this approach13,20,22. In contrast, we have included in our series 4 patients in whom LCND was performed prophylactically, since it is technically simpler on this side as the fatty lymphoid tissue is located anterior to the recurrent nerve.
In general, natural orifice surgery involves a longer surgical time than conventional surgery14.
We divided the surgical time into 3 categories: trocar placement, total lobectomy/thyroidectomy and LCND time, and specimen extraction time. We have chosen the CUSUM curves as the method to reflect the learning curves using the surgical time of this technique. Although this technique has been widely used in the field of surgery29–31, only one author had previously analyzed the TOETVA learning curve using CUSUM graphs32.
However, in said study, the interventions were not divided into different stages like in our case, which makes it difficult to compare the results. Thus, in our study we see how the curves of the different stages show different learning periods, so we believe that this division provides a more precise description of the process. If we look at the median time spent on lobectomies (80 min) and total thyroidectomies (140 min), our data are similar to those published in the literature13,19–27. Both the trocar placement curves and the specimen extraction curve have the characteristic shape, with an ascending stage, a plateau stage, and a descending stage, although it is true that these changes are much more evident in the trocar placement curve. However, the lobectomy time curve has a biphasic shape, in which, after an initial phase of learning-plateau-improvement, we find a new phase in the final part of the series. This second phase of “relearning” is probably due to the fact that, once the technique was consolidated, more complicated cases (carcinoma) were incorporated.
The transoral approach in our series did not entail a longer hospital stay13,17–25, which is similar to Western countries22 and lower than in Asia13,20.
We have confirmed only one permanent recurrent nerve injury after hemithyroidectomy (1.6%), and this patient was one of 2 in whom we could not identify the recurrent nerve. Although this incidence is within the standard for quality, other series have not reported permanent injuries20,22. The frequency of transient injury (1.6%) was lower than those published in other series (5.9%20, 4.5%22).
Only 2 of the 11 patients who underwent total thyroidectomy presented transient hypocalcemia (18.2%), and in no case was this permanent. These figures are similar to those of other larger published series (10.9%20, 18.2%22).
Inadvertent parathyroidectomy occurred in 3 of the 128 glands at risk (2.3%), a figure that is lower than others published with conventional surgery (17.3%33, 17.7%34). We believe it is necessary to point out that 2 of these 3 parathyroidectomies occurred in one of the patients in whom LCND was performed. Although the number of cases is very low and does not allow for conclusions to be drawn, we believe that, although total thyroidectomy does not seem to associate more risks of hypoparathyroidism than the conventional approach, the associated central neck dissection could carry a greater risk of inadvertent parathyroidectomy.
New approaches bring new complications. Paradoxically, with the TOETVA procedure, some of these are associated with negative cosmetic effects.
In our experience, all complications have been transient and have involved no sequelae.
Transient mental region palsy appeared in all cases and at varying intensities. In our opinion, it is more a consequence than a complication of the approach, and it can be minimized with correct trocar placement and by performing gentle, not extreme, movements to avoid distending the mental nerve15.
The same patient presented several complications (hematoma due to trocar bleeding, tracheal microperforation and fibrous band), which resolved spontaneously.
In no case was there infection of the surgical wound, hospital readmission or conversion to open surgery.
Our results are similar to others published previously, and we can conclude that, in selected patients, TOETVA is a safe and feasible technique in our setting. It offers results similar to open surgery, a condition sine qua non to persist, with the best cosmetic result.
Further studies with larger series are needed to define the role of this approach in cancer and the morbidity of central dissection.
AuthorshipP. Moreno Llorente and J. Vidal Fortuny have designed and written the manuscript.
M. Pascua Solé, A. García Barrasa, J.M. Francos Martínez, J.L. Muñoz de Nova and G. Fernández Ranvier have contributed to the composition and revision of the manuscript.
Conflict of interestsThe authors have no conflict of interests to declare.?