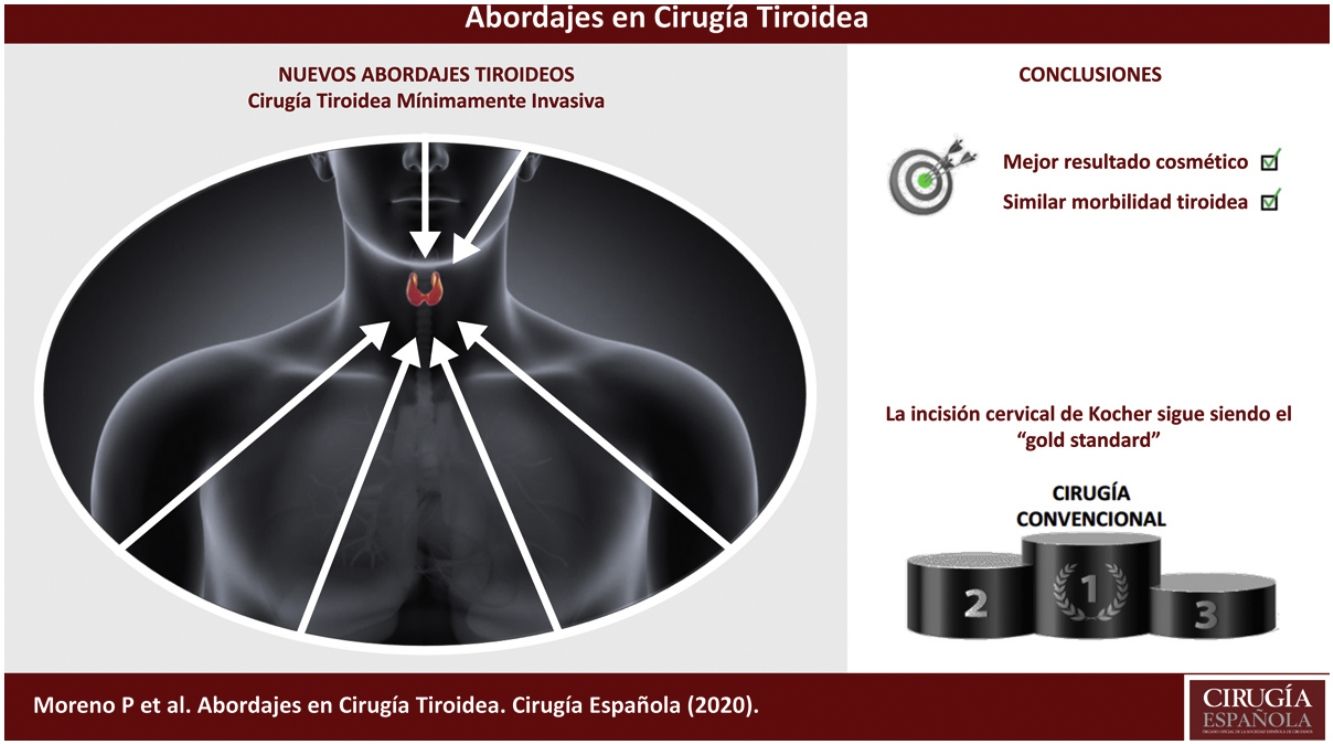
Thyroidectomy is the most frequent procedure in endocrine surgery. The conventional approach through a collar incision, as described by Kocher in 19th century, has become the “gold standard”. It is continuously evolving in spite of having been shown to be safe and efficient many years ago, with quality standards that are difficult to beat.
Endoscopic and robotic surgery have developed “new approaches” to the thyroid in order to improve the cosmetic results, even aiming for invisible scars.
We have made a thorough review of most of them with the intention of understanding their benefits and drawbacks.
Currently none of these “new approaches” have been shown to be better than conventional open thyroidectomy beyond offering a better cosmetic result. Besides, only a small percentage of patients can benefit of them. However, most of these approaches will remain if they treat the diseased thyroid and also improve the quality of life of our patients.
La tiroidectomía es el procedimiento más común en cirugía endocrina. La incisión cervical de Kocher es el «gold standard» para abordar el tiroides desde que fuera presentado por este a finales del siglo xix. Desde entonces, la tiroidectomía tal y como ahora la conocemos ha demostrado ser una técnica eficaz y segura, pero no por ello ha dejado de evolucionar habiendo conseguido además unos indicadores de calidad difíciles de superar.
El advenimiento de nuevas tecnologías y un intento constante por mejorar la cosmética de la cirugía han dado lugar a «nuevos abordajes». En este artículo hacemos una revisión de estos intentando mostrar sus beneficios y limitaciones.
Actualmente, ninguno ha demostrado ser mejor que la cirugía convencional más allá del valor añadido del beneficio cosmético, pero permanecerán si demuestran que han sido eficientes en el tratamiento de la enfermedad y en mejorar la calidad de vida de nuestros pacientes.
The history of thyroid surgery has been very eventful, especially in its beginnings, when at the start of the 17th century one of the first procedures led to the surgeon's condemnation. Fortunately, a deeper understanding of anatomy and physiology allowed for initial surgical misadventures to make thyroid surgery an art as well as a safe and effective treatment.1,2
The first descriptions of thyroid surgery come from the school of Salerno (Italy). In those days, even though only the size of the goiter was reduced, patients often died of sepsis or hemorrhage.3 The most famous surgeon of this time was Johann Hedenus, a German who reported the successful treatment of 6 large goiters in 1821.4 In the 1830s, Robert Graves and Karl von Basedow described diffuse toxic goiter using the recognition of the ‘Merseburg triad’ (goiter, palpitations, and exophthalmos).5,6 Interestingly, despite being attributed to Graves and Basedow, the association of goiter and orbital disease had been described in the 11th century by Persian doctors, Avicenna and Aj-Jurjani.7
The revolution in thyroid surgery began in the 19th century with the development of anesthesia, antisepsis and hemostasis.8 Albert Billroth and Theodor Kocher are considered the pioneers of modern thyroid surgery, as we now know it.
Billroth initially reported a post-thyroidectomy mortality rate close to 40%, mainly due to intraoperative hemorrhage and postoperative sepsis, which is why he abandoned the procedure for almost a decade.9 In 1877, after the advent of antisepsis and improved instrumentation, he regained confidence in the procedure and reduced the mortality rate to 8%.10,11
At the same time, the Swiss surgeon Theodor Kocher, considered the father of modern thyroid surgery, performed thyroidectomies through a collar incision that preserved the prethyroid muscles. Among other contributions, he also described the so-called ‘strumiprive cachexia’ secondary to the removal of the thyroid gland.9,12,13 Kocher is undoubtedly the example of a high-volume surgeon who, with a meticulous surgical technique and after performing more than 5000 thyroidectomies, reduced mortality to below 0.5%.12
William Halsted, a disciple of both, observed that most of Kocher's patients, unlike Billroth's, developed postoperative myxedema but rarely tetany, and he proposed that the origin of this phenomenon lay in technical differences.14 At the same time, in the United States, Charles Mayo adopted the Kocher partial thyroidectomy technique for patients with Graves’ disease,2 while his disciple, Thomas Peel Dunhill, adopted the total lobectomy technique on one side and subtotal resection on the other for patients with hyperthyroidism; additionally, he used a pericapsular thyroid dissection technique.13,14
Knowledge of the embryology and anatomy of the thyroid is essential to perform technically safe surgery. There is no place for improvisations in thyroid surgery given the serious consequences that these can have for the patient, exposing them to a life-threatening risk or negatively affecting their quality of life. The most important complications derived from surgical treatment are, basically, permanent injury to the recurrent laryngeal nerve and hypoparathyroidism. Nerve injury causes alterations in the voice that are sometimes difficult to treat, requiring rehabilitation and negatively affecting patient quality of life. Permanent hypocalcemia is an underrated chronic disease, both in its frequency and in its clinical importance. It causes a great variety of symptoms perceived daily on a recurring basis and generates drug and hospital dependency for life.
There are multiple factors that can affect the prognosis of patients after thyroidectomy, such as the diagnosis of the disease (benign or malignant), thyroid volume, retrosternal or endothoracic growth, the presence of inflammation or extrathyroid invasion and, very significantly, the surgeon's experience.
Although thyroidectomy, as we now know it, proved to be a safe and effective technique more than a century ago, it has continued to evolve and currently has quality indicators that are difficult to beat.
The advent of new technologies and a constant attempt to improve the cosmetics of surgery have led to new approaches. In this article, we review new approaches in thyroid surgery, attempting to show their indications, benefits and limitations.
Surgical approached for thyroidectomyConventional or open thyroidectomyThyroidectomy has become the most common endocrine surgery procedure. The most frequent indications include the treatment of thyroid nodules, large or symptomatic goiters, thyroid cancer or thyrotoxicosis that are refractory to medical treatment.15
The conventional cervical incision or Kocher incision has been the traditional approach to thyroidectomy since it was first introduced by Theodor Kocher in the late 19th century.
Although thyroidectomy, as described by Kocher, is still the gold standard technique used in most patients today, in recent years the development of endoscopic and robotic surgery has led to the implementation of minimally invasive techniques and new approaches to the thyroid through remote accesses, such as the armpit or the oral cavity.
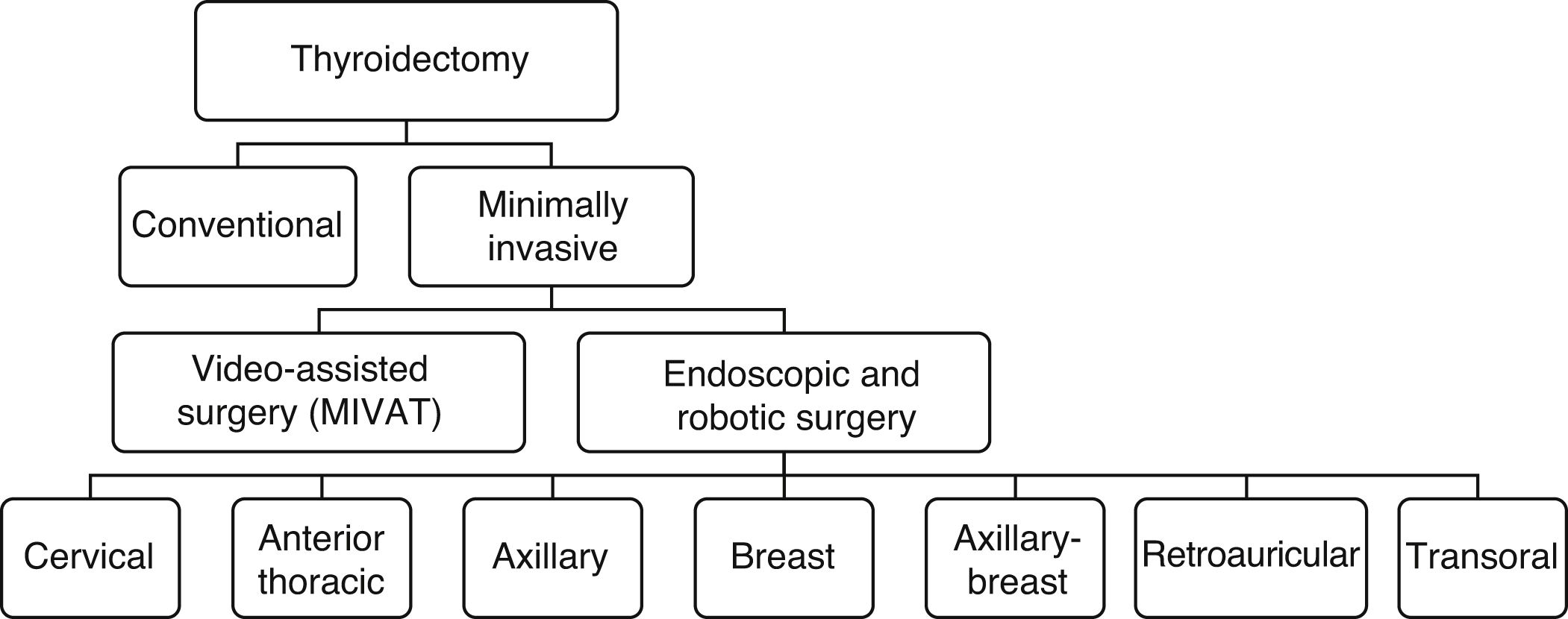
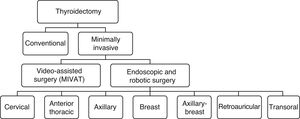
Fig. 1 lists the different minimally invasive techniques and approaches that make up this very heterogeneous group.
Minimally invasive thyroid surgeryMinimally invasive thyroid surgery was introduced in 1999.16 Although it was initially adopted with a certain degree of skepticism, it has now become increasingly more accepted worldwide.16,17 In recent years, remote accesses with endoscopes or robots have gained popularity for the surgical treatment of the thyroid gland. These techniques have been developed to minimize surgical morbidity and avoid or hide neck scars, as this is a cultural stigma in certain countries.
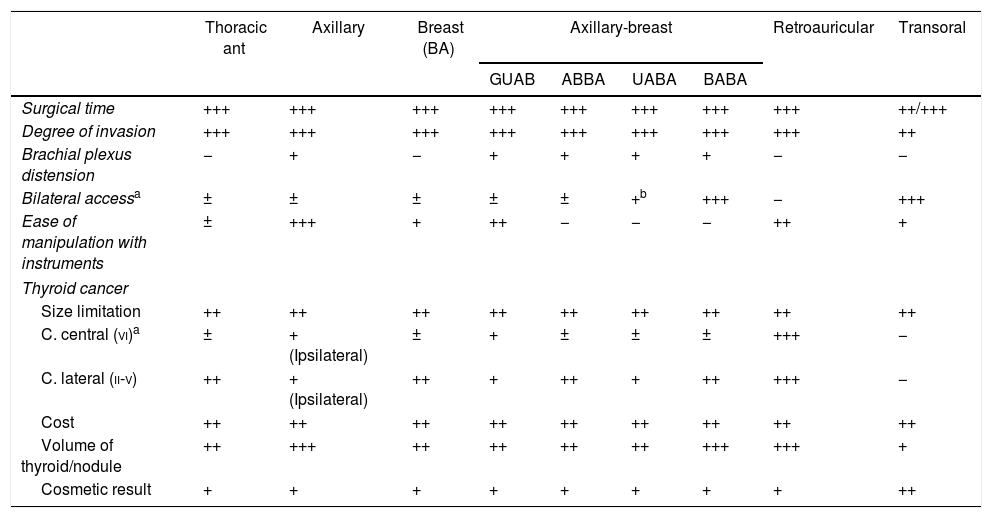
Remote approaches, either endoscopic or robotic, can be classified according to the approach, and multiple variants of each have been described. Table 1 summarizes the main remote access routes, which we will discuss below.
Characteristics of the remote thyroid approaches.
| Thoracic ant | Axillary | Breast (BA) | Axillary-breast | Retroauricular | Transoral | ||||
|---|---|---|---|---|---|---|---|---|---|
| GUAB | ABBA | UABA | BABA | ||||||
| Surgical time | +++ | +++ | +++ | +++ | +++ | +++ | +++ | +++ | ++/+++ |
| Degree of invasion | +++ | +++ | +++ | +++ | +++ | +++ | +++ | +++ | ++ |
| Brachial plexus distension | − | + | − | + | + | + | + | − | − |
| Bilateral accessa | ± | ± | ± | ± | ± | +b | +++ | − | +++ |
| Ease of manipulation with instruments | ± | +++ | + | ++ | − | − | − | ++ | + |
| Thyroid cancer | |||||||||
| Size limitation | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ |
| C. central (vi)a | ± | + (Ipsilateral) | ± | + | ± | ± | ± | +++ | − |
| C. lateral (ii-v) | ++ | + (Ipsilateral) | ++ | + | ++ | + | ++ | +++ | − |
| Cost | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ | ++ |
| Volume of thyroid/nodule | ++ | +++ | ++ | ++ | ++ | ++ | +++ | +++ | + |
| Cosmetic result | + | + | + | + | + | + | + | + | ++ |
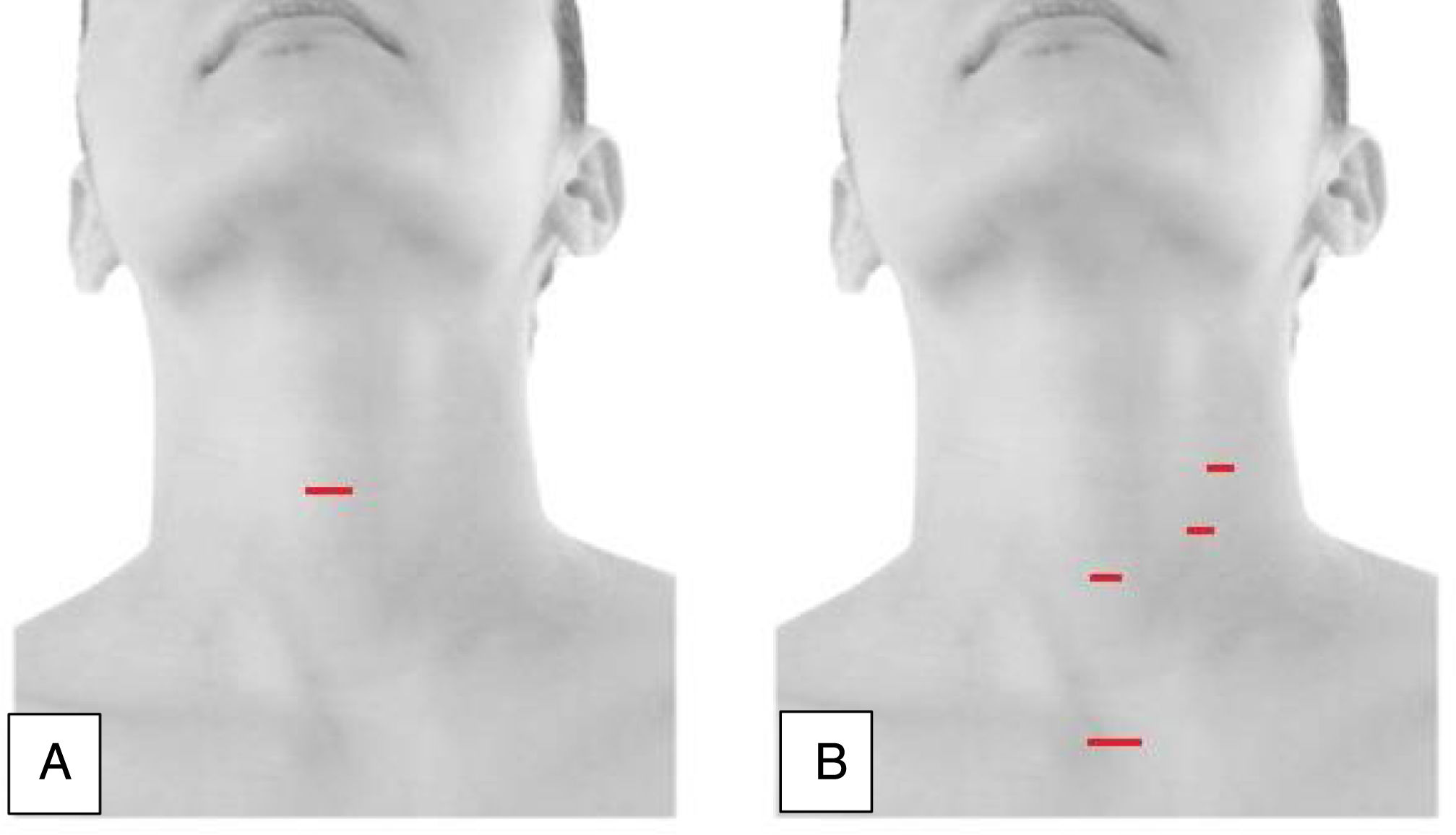
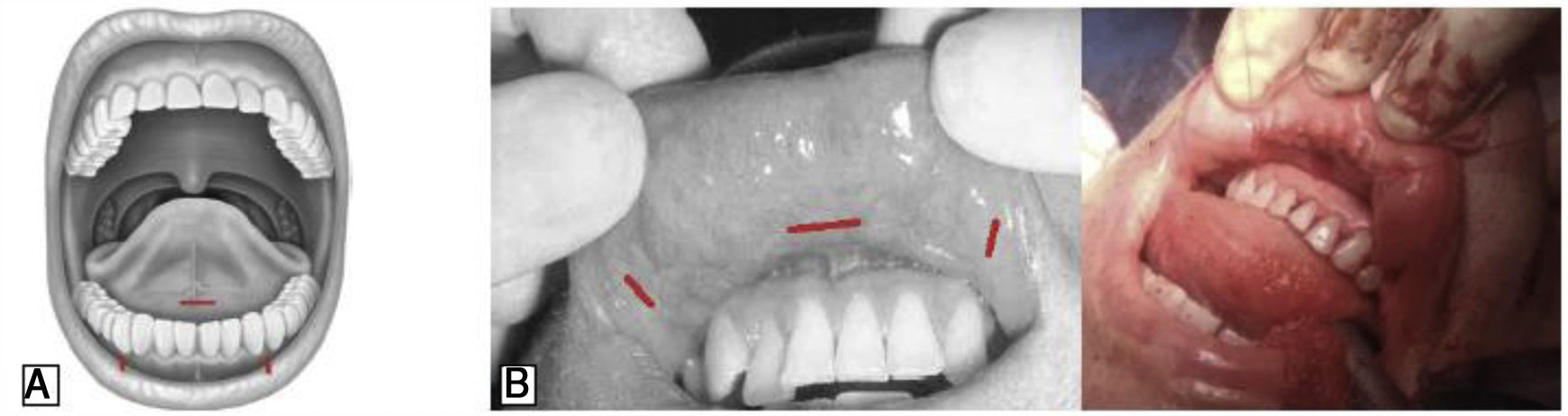
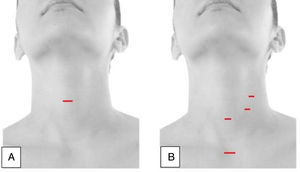
Video-assisted thyroidectomy is one of the first minimally invasive techniques to be described. It is performed through a single incision measuring approximately 1.5cm, located on the anterior surface of the neck, 2cm above the suprasternal notch (Fig. 2A). After making the incision, the platysma is divided, and the upper and lower skin flaps are made; subsequently, the prethyroid muscles are dissected and retracted laterally to explore the thyroid lobes. With the support of endoscopic vision, neurovascular structures and parathyroid glands are identified. This is a direct access method without CO2 insufflation and, although initially the use of videoendoscopic thyroid procedures was limited to treating only benign diseases, currently this treatment has also been performed in malignant tumors, although there is a broad consensus that it should be limited to ‘low-risk’ neoplasms. Proper patient selection is essential to make MIVAT a safe procedure with the same level of complications as conventional surgery, and which also offers some significant advantages in terms of cosmetic and postoperative results.18
Endoscopic thyroidectomyEndoscopic thyroidectomy through the cervical approachThis is an exclusively endoscopic procedure that uses CO2 insufflation to maintain the working field. In general, it uses one 10-mm endoscopic port and 2 or 3 5-mm ports for instruments (Fig. 2B). Careful patient selection plays an important role in the success of endoscopic thyroidectomy. Thus, patients with a long neck and a solitary thyroid nodule less than 3cm in diameter are highly suitable for this type of approach, while the treatment of malignant nodules by this means remains controversial.19,20
Endoscopic vision provides a magnification of the visual field, which is especially important for the laryngeal nerves and the parathyroid glands. In addition, because the muscle is not divided during endoscopic thyroidectomy, there is less tissue trauma, leading to a faster return of the patient to daily activities. This endoscopic approach aims to provide cosmetic results that are superior to conventional thyroidectomy due to the smaller size of its incisions. Its main drawback is the difficulty of working due to the proximity of the instruments and the long duration of the surgery, although this may improve with the experience of the surgeon.21
Endoscopic thyroidectomy through the anterior thoracic approachThe endoscopic thyroidectomy using an anterior thoracic approach proposed by Ikeda et al. describes an approach through the anterior chest wall to avoid cervical incisions.22
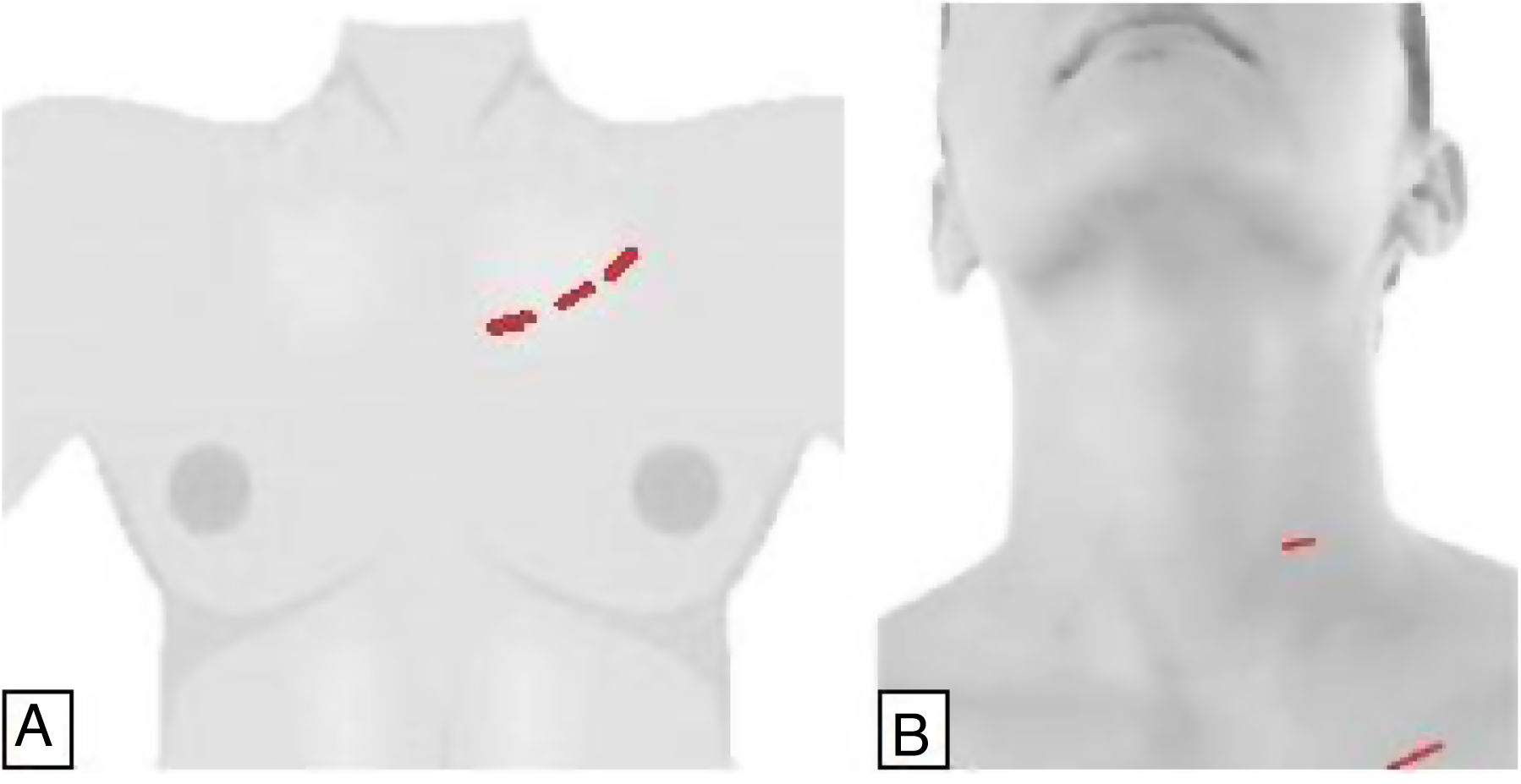
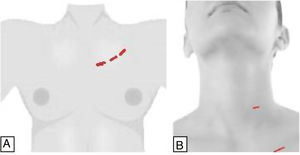
DescriptionA 3-cm incision is made below the lower edge of the clavicle on the side of the lesion. A 2-mm trocar is inserted through the tobacco pouch incision to prevent gas leakage, port slippage and insufflation of CO2 (4mmHg). Two additional 5-mm trocars are placed, one inferior to the sternal notch and the other below the ipsilateral clavicle (Fig. 3A).
VariationsEndoscopic thyroidectomy by axillary approachEndoscopic thyroidectomy through the axillary approach was first presented by Ikeda et al. in the year 2000.26
DescriptionA 3-cm incision is made in the axilla. Two trocars, one 12mm and the other 5mm, are inserted into the incision and a tobacco pouch is made to prevent gas leakage and trocar slippage. CO2 is insufflated to 4mmHg. A third 5mm trocar is inserted near the 3cm incision in the armpit. The specimen is extracted through the 3cm incision, leaving a drain tube through the 5-mm trocar. This approach avoids scars on the neck and anterior thorax, and the small scar in the armpit is completely hidden by the patient's arm in a natural position (Fig. 4A).26,27
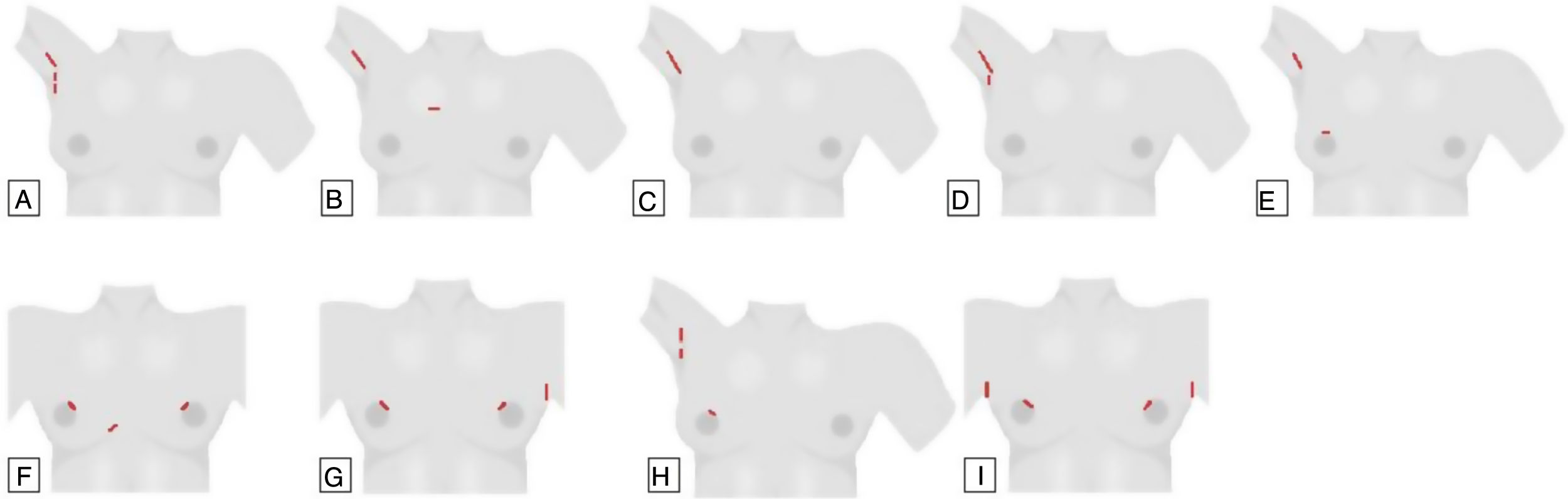
(A) Endoscopic axillary approach; (B) gasless transaxillary approach with anterior thoracic port; (C) single-incision transaxillary approach; (D) gasless unilateral axillary approach (GUA); (E) gasless unilateral axillary-breast approach (GUAB); (F) gasless breast approach; (G) axillary bilateral breast approach with gas (ABBA); (H) unilateral axillary-breast approach with insufflation of CO2; (I) Bilateral axillary-breast approach (BABA), with gas.
- -
- -
Robot-assisted gasless transaxillary approach29–31
- -
GUA or gasless unilateral axillary approach with areolar incision (gasless unilateral axillary-breast approach [GUAB])32 (Fig. 4D and E, respectively).
The advantages of the axillary approach over the other endoscopic techniques include:
- 1.
It provides for the extraction of larger tumors or nodules, so that more patients can benefit from this type of technique.32
- 2.
The nerve can be easily identified.
- 3.
Ipsilateral central lymph node dissection is possible.
- 4.
The scar is covered by the arm in a natural position.
The original breast approach with gas, described by Ohgami et al,33 used a port in each breast and a parasternal port (Fig. 4F), but since the scar in this area tends to have hypertrophy, several modifications were developed to avoid this incision, replacing it with one or two axillary ports.33,34
Variations- -
Axillary bilateral breast approach (ABBA)35
- -
Gasless unilateral axillary-breast approach (GUAB)32
- -
Unilateral axillary-breast approach with gas (UABA with gas)36
- -
Unilateral axillary-breast approach without gas (UABA without gas)37
- -
Bilateral axillary-breast approach (BABA)38
In 2003, Shimazu et al.35 presented the results of a technique called ABBA that uses 2 breast ports and an axillary port (Fig. 4G).
A mammary port and 2 axillary ports can also be used interchangeably on one or both sides36 (Fig. 4H).
In 2007, Choe et al.38 modified the ABBA, describing the BABA in order to obtain optimal visualization and access the entire thyroid gland by adding a contralateral axillary port. BABA requires 4 incision sites, 2 in the areola and an incision in each axilla (Fig. 4I), but it simplifies or facilitates the bilateral approach to the thyroid.
Since their introduction, ABBA and BABA have had similar indications that have included low-risk thyroid cancer no larger than 1cm, follicular neoplasms smaller than 3cm, and benign thyroid tumors.
Retroauricular approachThe gasless retroauricular robotic thyroidectomy described by Terris et al. in 2011 uses a retroauricular incision (Fig. 5), which offers good cosmetic results as well as a shorter access to the thyroid than the previously described techniques.39
The incision starts from the retroauricular fold, progressing toward the occipital hairline and creating a flap that extends laterally to the greater auricular nerve and jugular externally and inferiorly, ventral to the sternocleidomastoid muscle and to the clavicle. This defines a triangle between the omohyoid, sternocleidomastoid and sternohyoid muscles. It requires the use of a retractor to separate the prethyroid muscles ventrally and anteriorly, and another to retract the sternocleidomastoid muscle laterally and posteriorly.
Unlike the axillary approach, this technique has the advantage of the absence of distention of the brachial plexus, as well as the possibility of performing lymph node dissection of the central (level VI) and lateral (levels II-IV) compartments.
VariationsTransoral approachThe main objective of this approach was to develop a technique with no visible scars by accessing the thyroid through a natural orifice and by the shortest route, minimizing dissection. The transoral approach through a sublingual incision was first reported by Witzel et al. in cadavers.43 Subsequently, the technique has evolved into an oral vestibular approach with or without CO2 insufflation.44–46 The first transoral thyroidectomy performed in humans was performed by Wilhelm, using a sublingual port and 2 ports in the oral vestibule (Fig. 6A).47,48 The first exclusively vestibular approach was described by Richmon et al. in a cadaveric model using 3 oral ports in the vestibule of the oral cavity.49 Subsequently, Nakajo et al. also described a gasless transoral video-assisted surgical technique using a single 2.5-cm incision in the oral vestibule.50
Nevertheless, this approach was finally consolidated by Angkoon Anuwong, who made technical modifications to develop the transoral endoscopic thyroidectomy with a vestibular approach (TOETVA), as it is known worldwide today. In 2018, he published for the first time a series of 425 cases, reporting excellent results in terms of both thyroid morbidity and cosmetic results (Fig. 6B).51,52
The transoral approach provides access to the thyroid bilaterally and endoscopically through a natural orifice in a more direct way (less invasive and with less dissection), in addition to the central compartment.
Regarding the morbidity of TOETVA, new complications associated with the approach have been described, such as injury to the mental nerve, cervical infections due to the passage of saliva from the oral cavity, skin injuries during dissection, etc.
Currently, it has been shown that the transoral approach is feasible, effective and safe for thyroidectomy, while it also offers the best cosmetic results so far. However, adequate patient selection and more studies are essential to confirm its viability and to determine its place in the future surgical approach of the thyroid.
Robotic thyroidectomyParallel to the development of endoscopic thyroidectomy, robotic surgery has used the same remote accesses already described. It provides visual magnification, 3D vision and elimination of tremor, providing finer and more precise movements. However, robotic procedures require more time than endoscopic approaches, which, in turn, are longer than conventional surgery due to the time required for docking of the robotic arm.53–57 Furthermore, robotic surgery has an even greater learning curve than endoscopic surgery.58–60
Comparison between the different approachesCurrently, it is difficult to say which remote procedure is the best, as each has its advantages and disadvantages.
Techniques that use gas offer the advantage of a more stable surgical field, and the remote orifice requires a smaller incision with better cosmetic results. In contrast, the absence of gas insufflation provides a clearer visual field, with less influence of smoke and vapors. This also avoids other disadvantages of CO2 insufflation, such as subcutaneous emphysema, hypercapnia, respiratory acidosis, risk of cerebral edema and CO2 embolism, although the latter are extraordinarily rare when working with pressures below 6mmHg.61,62
Regarding the skin flap, the transoral approach offers the most direct access to the thyroid compared to the remaining remote approaches, but with the disadvantage that the surgical field is narrower, which significantly limits the mobility of the instruments.
With regard to cancer treatment, all techniques allow the central compartment to be approached with a more important limitation of the BABA due to lack of angulation and probably the transoral approach on the right side to access the recurrent laryngeal nerve lymph nodes. The retroauricular approach also enables lateral or functional lymph node dissection.
Regarding the volume of the surgical specimen, the transoral route undoubtedly has the greatest limitation (nodule≤6cm, thyroid≤10cm),63 especially in cancer cases, where the nodule must be intrathyroid and not exceed 2cm.64
Finally, although from a cosmetic perspective all these techniques provide excellent results, the transoral approach seems to be the best because it uses a natural orifice.
Table 1 summarizes the characteristics of the different remote accesses.
ConclusionDespite the fact that thyroid surgery was proven to be safe and effective more than a century ago, it is constantly evolving, and the current quality indicators are difficult to beat.
The implementation of endoscopic and robotic surgery has enabled the use of remote approaches of the thyroid with the intention of minimizing the scar or making it invisible.
Among the remote access approaches, the transaxillary, bilateral axillary-breast, retroauricular, and transoral are currently in common use. However, this is highly controversial because they are not considered very cost-efficient – rather a ‘niche’ surgery from which only a few patients can benefit. The challenge is to maintain the morbidity figures while minimizing the new complications associated with the access points.
Currently, none of these techniques has proven to be better than conventional surgery, beyond the added value of cosmetic benefits. Nonetheless, they will remain if they are efficient in treating the disease while improving the quality of life of our patients.
Conflict of interestThe authors have no conflict of interests to declare.
Please cite this article as: Moreno Llorente P, Gonzales Laguado EA, Alberich Prats M, Francos Martínez JM, García Barrasa A. Abordajes en cirugía tiroidea. Cir Esp. 2021;99:267–275.