Bariatric surgery is one of the most common surgical practices in Spain. However, this procedure currently has longest delay on surgical waiting lists (SWL). We have developed a special surgical program that aims to reduce this waiting list and to assess the economic and clinical repercussions in a high-volume bariatric surgery unit.
MethodsA three-month prospective study was carried out comparing outcomes, results and perioperative resources consumed for 45 patients who underwent bariatric surgery. The patients were divided into 2 groups: patients who underwent the standard procedure in the operating room, and patients treated in the special program. Epidemiological, healthcare and economic factors were taken into account.
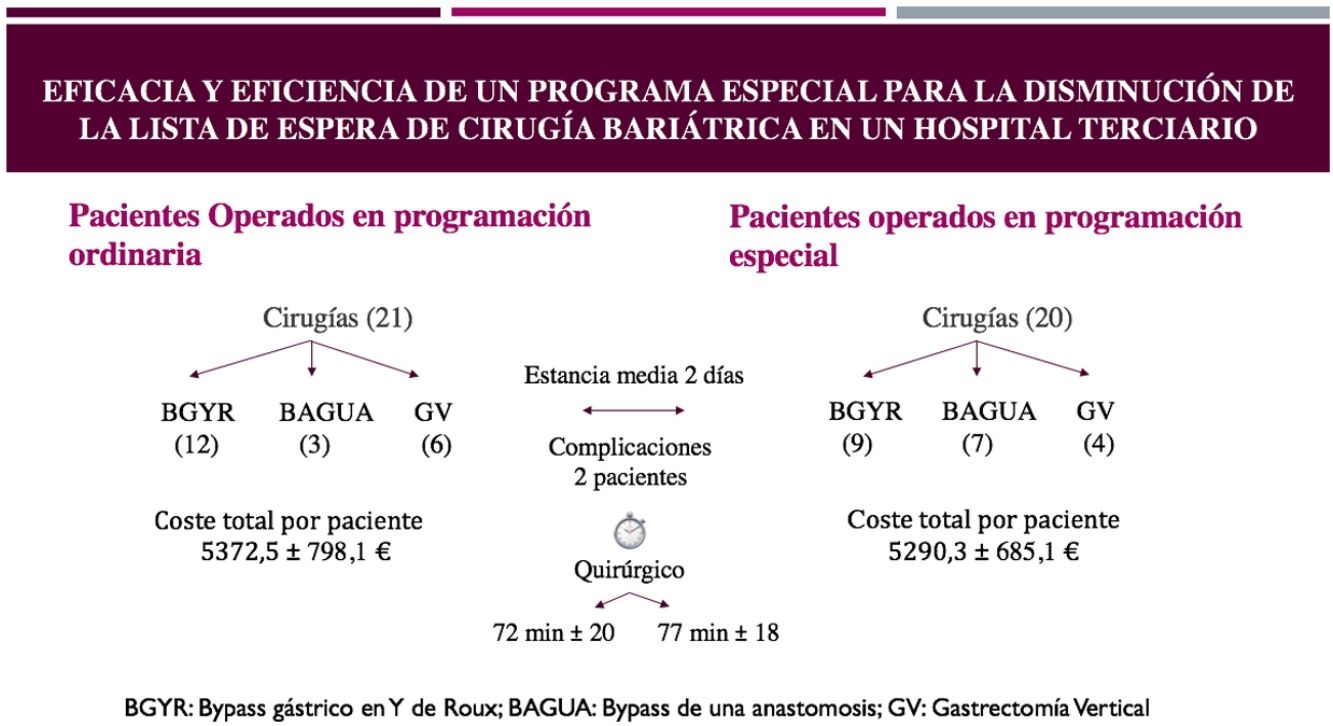
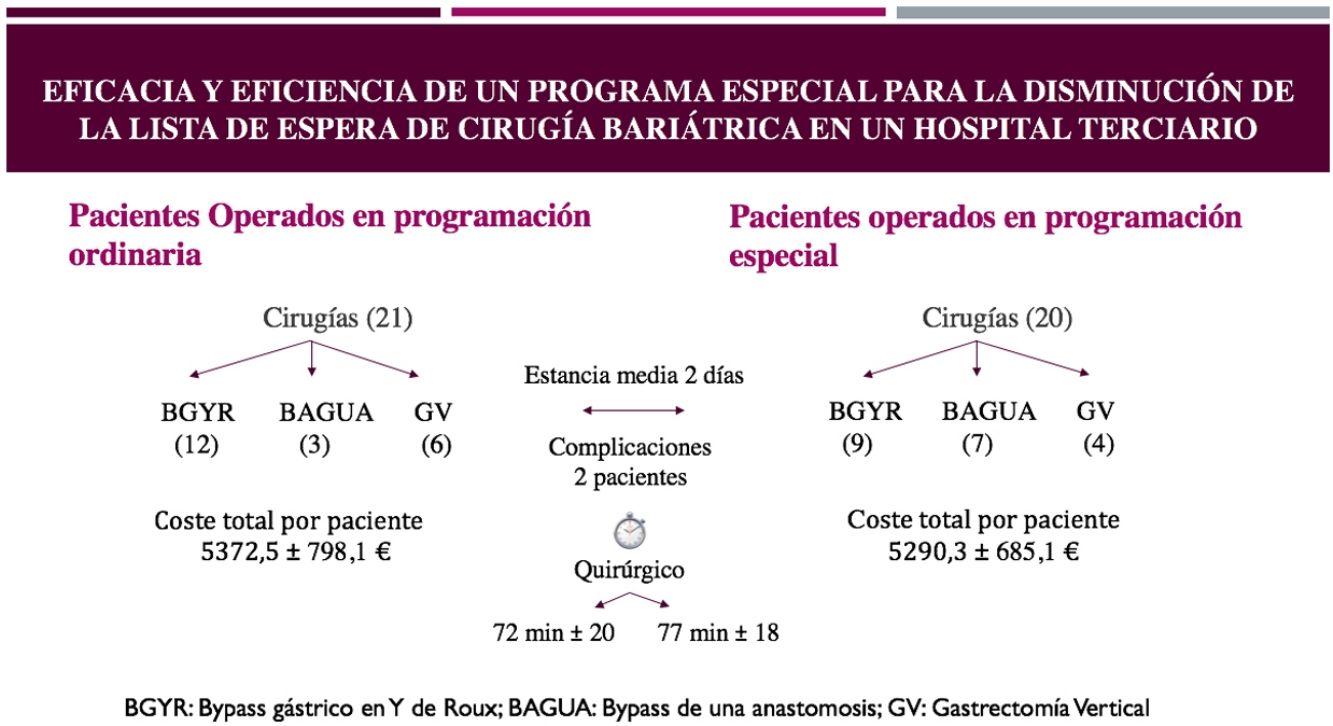
ResultsTwo homogeneous groups of patients were operated on, successfully reducing the SWL. Morbidity was similar in both groups and the average cost of the surgeries performed was €5,331.40; in the standard group, the cost was €5,372.50±€798.10, and the cost of the special program group was €5,290.30±€685.10, with no significant differences.
ConclusionsIn hospitals with a high volume of bariatric surgery, it is feasible to incorporate special surgical programs that are able to reduce surgical waiting lists, while maintaining quality criteria and without incurring a greater expense to the healthcare system.
La cirugía bariátrica es uno de los procedimientos quirúrgicos más realizados en España, sin embargo actualmente es la cirugía con mayor demora en la lista de espera quirúrgica (LEQ). Para disminuir la LEQ se pone en marcha un programa especial de autoconcertación, y se quiere valorar su utilidad, estudiando las repercusiones clínicas y económicas en una unidad de alto volumen de cirugía bariátrica.
MétodosSe realizó un estudio prospectivo de 3 meses comparando evolución, resultados y consumo de recursos perioperatorios de 45 pacientes operados de cirugía bariátrica, divididos en 2 grupos, pacientes operados en quirófano de forma estándar y pacientes operados en programación especial. Se tuvieron en cuenta factores epidemiológicos, asistenciales y económicos.
ResultadosSe operaron 2 grupos homogéneos de pacientes, reduciendo con éxito la LEQ. La morbilidad fue similar en ambos grupos y el coste medio de las cirugías realizadas fue de 5.331,4euros, 5372,5±798,1euros para el grupo estándar y 5.290,3±685,1euros para el grupo de programación especial, sin diferencias significativas.
ConclusionesEn centros hospitalarios donde se realiza alto volumen de cirugía bariátrica es factible incorporar programas especiales quirúrgicos que permiten la reducción en la demora de las listas de espera quirúrgica, manteniendo los criterios de calidad y sin suponer un mayor gasto al sistema sanitario.
Obesity, along with its associated comorbidities, poses a challenge to public healthcare systems and economies around the world. In Spain, the prevalence of being overweight in adults over the age of 18 is around 44% in men and 30% in women, while the prevalence of obesity is about 20% and 16%, respectively.1,2 In the Valencia region of Spain, it is estimated that one in 2 adults are overweight, classified as follows: 35% overweight, 15.8% obese, and 1.7% morbidly obese.3
In addition to resolving comorbidities and increasing the survival of morbidly obese patients by up to 10 years, bariatric surgery provides significant savings for the Spanish National Healthcare System, since these patients can consume up to 20% more healthcare resources and 68% more drugs than the general population.4 Furthermore, we must consider that delayed surgical treatment of morbid obesity leads to increased BMI and growing incidence and severity of comorbidities, with a reported 30% increase in mortality for every 5kg/m2 increase in BMI.5,6
Bariatric surgery is one of the most performed surgeries included in the public health system in Spain. Nevertheless, it is quite possibly the procedure with the longest delays, topping the surgical waiting list in our country. In 2017, the Spanish Society for Obesity Surgery carried out a study in which the average wait for bariatric surgery in Spain was 397 days, and 68% of the patients were on the list for more than 6 months.7 Currently, there is no uniform strategy based on established criteria to reduce this waiting list, and bariatric surgery is one of the first victims when there are shortages of operating rooms or hospital beds. Such was the case in the recent healthcare crisis caused by the SARS-Cov-2 pandemic, during which obesity surgery was canceled in practically all hospitals within the health network.
Faced with this situation, there are different strategies, such as outsourcing surgery through the creation of monographic hospitals for bariatric surgery, or agreements made with private medical centers. Another possible strategy to combat this situation, or to at least make amends in times of crisis, is to create specific publicly financed special programs aimed at the treatment of obese patients with surgical indication, which take place at the public hospitals themselves. The Consell de la Generalitat Valenciana reached an agreement, whose purpose is to establish and regulate the special productivity program aimed at reducing the delay in surgical procedures and in the performance of diagnostic techniques in the Valencian Healthcare System; one of the interventions included in the program was bariatric surgery.8 These programs are conducted in the surgery units of hospitals where bariatric surgery is normally included in their scope of services. This type of program raises 2 fundamental preliminary questions: firstly, as it is a complex surgery, will surgical risk increase in this different scenario? And secondly, are there cost differences that negatively affect the distribution of healthcare resources? To study both aspects, a 3-month pilot program in bariatric surgery was carried out to analyze whether including bariatric surgery in this type of program is worthwhile and ethical.
MethodsWe conducted a prospective study of patients with obesity treated consecutively in our department over a period of 3 months, during which a special bariatric surgery program was established. Our study compared the evolution and consumption of resources of patients who underwent normally scheduled surgery versus patients operated on in the special program.
- •
From November 1, 2019 to January 31, 2020, 45 bariatric surgeries were conducted in our service: 25 in the scheduled operating room, and 20 in the special program operating room.
- •
The inclusion criterion was: patients who underwent bariatric surgery in the period studied. The only exclusion criterion was: revision surgery, for which 4 patients were excluded.
Patients were classified into 2 different groups:
- •
Patients operated on in the standard operating room.
- •
Patients operated on in the special program operating room.
The following parameters were collected from all patients:
- •
Anthropometrics: age, sex, starting weight and body mass index (BMI); preoperative weight and BMI (after preoperative diet).
- •
Epidemiological: comorbidities present before surgery.
- •
Surgery: type of procedure, duration of operation, length of hospital stay, perioperative complications.
- •
Economic: approximate cost per patient.
All patients followed the same preoperative circuit, with standard pre-anesthesia work-up and a hypocaloric diet for one month, monitored by the endocrinology and nutrition service. The interventions performed were the Roux-en-Y gastric bypass (RYGB), the one-anastomosis gastric bypass, and sleeve gastrectomy (SG), all of which were laparoscopic. As this is a study of consecutive patients, there was no randomization or homogenization of techniques; the surgeries performed in the two programs were considered as a whole.
In the scheduled group, the interventions were carried out in continuous operating room sessions, from early in the morning until the end of surgery in the afternoon, combining bariatric and endocrine surgery procedures, which are performed in our hospital by the same unit. The teams consisted of experts in both schedules.
The special program operations were all done in the afternoon. The surgical team was the same in both groups, although the anesthetists varied. The nursing team kept one of the usual scrub nurses, although the other nursing member, the auxiliary nurse, and the orderlies were variable.
All patients were admitted the same day as the surgery and went directly to the operating room. After surgery, they spent a few hours in the post-anesthesia recovery unit, from where they were transferred to the surgical ward. Patients were usually discharged on the 2nd postoperative day.
The cost calculation was not done by individualized accounting, which is not possible in our setting, but instead by inference using data from the information and economic management department (SIGE) of the hospital, which determines the consumption of resources for each activity, distinguishing between human, material and structural resources.
The consumption of structural and consumable materials was similar in both groups, with no significant differences between techniques either. However, differences were found in the cost of personnel. In the case of the scheduled surgery group, this was calculated by the consumption of minutes and the cost in human resources in the standard operating room per minute of the procedure, according to SIGE data. In the case of the special program, the cost of human resources was established by the Agreement of the Consell de la Generalitat Valenciana,8 and the corresponding ‘price’ per minute was calculated; this was multiplied by the number of minutes to determine the human resources consumed for each procedure. In addition, the cost per day of hospitalization in our ward was added, multiplied by the number of days of stay. Although the final data are not absolutely exact, they are approximate, and the calculation method is similar for both groups. Complementary tests and lab work performed preoperatively or after discharge were not included in the cost calculation.
The descriptive statistical analysis was done by calculating the absolute values and frequencies or the median and range for categorical variables. For quantitative variables, their normality was verified with the Kolmogorov–Smirnoff test and expressed as means±SD. Both groups were compared using the Student’s t-test for unpaired data; a P value <.05 was considered statistically significant.
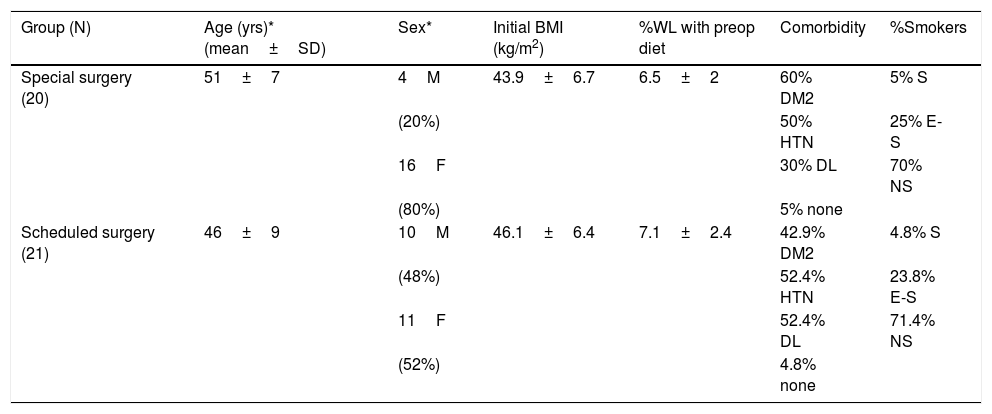
ResultsTwenty-one patients underwent surgery in the scheduled surgery group (14 in the morning and 7 in the afternoon), and 20 patients in the special program group. The data for the two groups are found in Table 1, and both groups were homogeneous. Only age showed a slightly significant difference; patients in the scheduled group were younger and nevertheless presented a higher percentage of male patients. Both groups were similar, with no statistically significant differences in terms of initial or preoperative BMI, response to the previous hypocaloric diet, presence of comorbidities, or percentage of smokers and ex-smokers.
Preoperative characteristics of the 2 groups.
| Group (N) | Age (yrs)* (mean±SD) | Sex* | Initial BMI (kg/m2) | %WL with preop diet | Comorbidity | %Smokers |
|---|---|---|---|---|---|---|
| Special surgery (20) | 51±7 | 4M | 43.9±6.7 | 6.5±2 | 60% DM2 | 5% S |
| (20%) | 50% HTN | 25% E-S | ||||
| 16F | 30% DL | 70% NS | ||||
| (80%) | 5% none | |||||
| Scheduled surgery (21) | 46±9 | 10M | 46.1±6.4 | 7.1±2.4 | 42.9% DM2 | 4.8% S |
| (48%) | 52.4% HTN | 23.8% E-S | ||||
| 11F | 52.4% DL | 71.4% NS | ||||
| (52%) | 4.8% none |
DL: dyslipidemia; DM2: diabetes mellitus type 2; E-S: ex-smoker; S: smoker; HTN: hypertension; BMI: body mass index; F: females; M: males; NS: nonsmoker; %WL: percent weight loss.
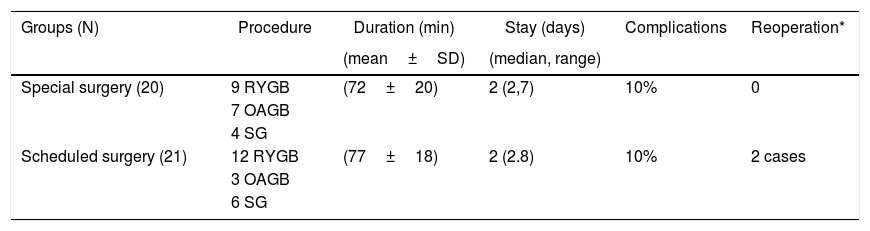
Table 2 summarizes the perioperative parameters. The procedures carried out in both groups were mainly the RYGB (51.0%), and the rest were OAGB (24.5%) and SG (24.5%). Although there was no systematization of the types of procedures performed, the same 3 types of interventions were performed in the 2 groups, the majority of which were RYGB in both groups. Similar durations of the intervention and postoperative stay were observed in both groups. Only 2 patients in each group had complications, although those in the scheduled group were more serious, requiring reoperation. Both cases were SG, which presented intraperitoneal hemorrhages due to omental bleeding and were resolved by laparoscopy in the first 48h. The other 2 complications included a SG stenosis, which was resolved with endoscopic dilations, and bleeding from the abdominal wall in a case of OAGB. None of the complications occurred in patients who underwent RYGB.
Perioperative parameters.
| Groups (N) | Procedure | Duration (min) | Stay (days) | Complications | Reoperation* |
|---|---|---|---|---|---|
| (mean±SD) | (median, range) | ||||
| Special surgery (20) | 9 RYGB | (72±20) | 2 (2,7) | 10% | 0 |
| 7 OAGB | |||||
| 4 SG | |||||
| Scheduled surgery (21) | 12 RYGB | (77±18) | 2 (2.8) | 10% | 2 cases |
| 3 OAGB | |||||
| 6 SG |
OAGB: one-anastomosis gastric bypass; RYGB: Roux-en-Y gastric bypass; SG: sleeve gastrectomy.
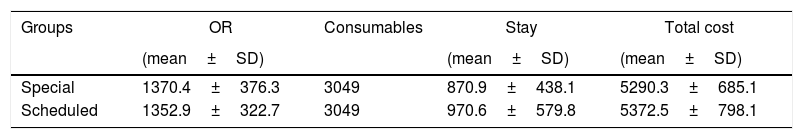
The mean cost of bariatric surgery in our hospital was €5331.40, and Table 3 shows the approximate costs of the interventions in both programs. The CA program was slightly cheaper, but the differences were not statistically significant.
Costs per patient (€).
| Groups | OR | Consumables | Stay | Total cost |
|---|---|---|---|---|
| (mean±SD) | (mean±SD) | (mean±SD) | ||
| Special | 1370.4±376.3 | 3049 | 870.9±438.1 | 5290.3±685.1 |
| Scheduled | 1352.9±322.7 | 3049 | 970.6±579.8 | 5372.5±798.1 |
Stay: mean cost of stay in ward; Consumables: cost of materials consumed/disposables (total mean cost); OR: operating room costs, including staff, structure and materials.
No differences between the two groups were significant.
Currently, one of the main problems of public healthcare is the disproportion between the demand for services and the available resources, which leads to a delay in the treatment of surgical diseases. Bariatric surgery is one of the surgical subspecialties that is most affected by this problem because the prevalence of morbid obesity is increasingly high. Also, since it is not oncological or urgent surgery, it is often downgraded in the order of operating room priorities. This situation has been demonstrated over the course of the serious COVID-19 health crisis, in which emergency or oncological surgery was maintained in many health centers, but bariatric surgery was not maintained in practically any. In fact, during the month of March 2020, only 6 obesity patients were operated on in our hospital, and none were treated in the months of April and May.
The recent article by Arteaga et al. mentions a mean national delay of 397 days for the procedure after having been added to the surgical wait list. However, the delays range up to 5 years, and more than 11 000 patients are registered on the waiting list. At this time, morbid obesity is the third most frequent indication in general surgery, only surpassed by cholelithiasis and hernias. However, only 13% of hernias and 15% of cholelithiasis have to wait more than 6 months to be operated on, compared to 68% of obesity cases.7 Few studies have been published about the management of waiting lists in bariatric surgery: in Canada and the United States, there are reports of 5 years and up to 206 days, respectively.9,10 What seems to be proven is that the delay in the surgical treatment of these patients leads to the appearance of cardiovascular,11 endocrine, infectious, neoplastic and psychiatric12 complications. In many cases, mortality can also result from the delay, since surgery reduces the mortality rate up to 89% compared to patients in a homogeneous group that has not had bariatric surgery.12
For these reasons, it is necessary to increase bariatric surgical activity throughout the country. Some possible solutions include expanding the number of surgery services that provide this surgery (this is being achieved progressively, and in the Community of Valencian there is a training program that has incorporated this surgery in almost all regional hospitals), and another solution is to increase the number of these interventions in high-volume hospitals, through specially paid programs.
The results of our study show that bariatric surgery practically doubled in the study period, despite being months with holiday periods included. The use of special surgery programs for complex surgeries involves a risk that, when working outside standard practice, the resources assigned (generally volunteer personnel and in afternoon programs) may not be optimal, and increased morbidity and mortality rates could be a result. Therefore, this type of program must meet criteria for quality, safety and efficiency.13 In our study, we have verified that there were no significant differences in care, with a similar duration of surgeries and hospital stays, and a similar incidence of complications. The small number of cases collected is a limitation. In our program, 2 patients from the scheduled group had to be reoperated, although they were the only patients requiring reoperation during the year out of more than 120 bariatric surgery cases. The hospital stay in the scheduled surgery group was slightly longer, although without being statistically significant. The differences may be attributable to the 2 patients who had to be reoperated, as well as to the patients operated on in the morning, which slightly lengthened the hours of hospitalization.
These results reduce the concern about the increased risk when working outside standard practice, as appeared in another recent article,14 which mentions increased morbidity in patients operated on in direct surgery courses, despite being operated on by surgeons with recognized experience and prestige. This article reports that morbidity doubled, which they attribute to the lack of team coordination and little familiarity with the instruments and the environment, among other things.14 In our hospital, these factors were minimized by 2 circumstances: the staff involved in these programs had to have at least one team member for each staff category belonging to the usual teams for this surgery, thereby including anesthesiologists and nursing staff familiar with the procedure. In addition, our standard scheduled surgery was performed in both morning and afternoon sessions, with no protocol differences. Also, despite the accumulation of many patients operated on each week, surgeries were scheduled to be within the material possibilities of proper care to avoid the depletion of resources.
The other big question about this pilot program is its economic impact: lower costs would bring into question the overall efficiency of the national healthcare system, and an excessive increase in costs would raise ethical concerns about giving better use to economic resources. In national publications about this subject, and with the lack of individualized accounting in public hospitals that is available in private hospitals, it is difficult to assess specific care episodes, especially if they are carried out in common-use spaces like the operating and recovery rooms. The diagnosis-related group (DRG) system, in which this surgery would be code 288 ‘Gastric surgeries for obesity’ (relative weight=1.4767),15 has been shown to be ineffective in our settin,16 where costs are standardized in a non-specific manner.
The comparison with systems in other countries is not valid either, since it shows a considerable difference in costs: while prices in Spain for DRG 288 are €74684 or €8344,17 the average cost published in the United States is $19 746,18 and €14 600 in Finland.19
In our study, the data provided by the hospital SIGE, which uses the existing Economic Information System in the Community of Valencia,20 have been used. A cost estimate has been made by calculating the consumption of resources per minute in the operating room and per day of hospital stay, adding the cost of consumable materials used.
The amounts obtained are different from those reported by Sánchez et al.,4 who list the statistics portal of the National Health System as a source but do not explain the calculation method. They also differ from the Anselmino et al. study,17 whose calculation included office visits and follow-up, which were not included in our study. Our calculation system was quite similar to the Rodicio et al. study,16 although they also include the price of consultations and examinations, which we did not include, and their result was €10 572.20. In our opinion, the amount obtained is quite in line with the reality of the cases considering the public health parameters, but above all, it provides an objective comparison of the 2 case groups analyzed. Although there are no significant differences, the cost of the special program is slightly lower. In our opinion, this is due to the higher performance and the occupation of operating rooms in the afternoon, as well as the shorter duration of hospital stays. Furthermore, the cost allotted for surgeons’ services established in the special programs agreement8 is clearly on the low side.
In conclusion, the incorporation of special surgical programs for bariatric surgery in public hospitals is able to reduce delays in treatment and the surgical waiting list. In addition, it complies with criteria for total quality, safety and efficiency, which are required in the incorporation of surgical programs that go beyond standard scheduled surgery, all without entailing higher healthcare costs. For this reason, these surgery programs could be especially useful for resuming bariatric activity after a shutdown caused by a healthcare crisis.
FundingThis project has received no funding from external sources.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Kraus-Fischer G, Alfonso-Ballester R, Mora-Oliver I, Cassinello-Fernández N, Ortega-Serrano J. Eficacia y eficiencia de un programa especial para la disminución de la lista de espera de cirugía bariátrica en un hospital terciario. Cir Esp. 2021;99:276–281.