In acute liver failure secondary to iatrogenic lesions caused during cholecystectomy, emergency liver transplantation is a last-resort therapeutic option due to the transcendence of the procedure.
We present the case report of a patient with damage to the hepatic artery and portal thrombosis that occurred during open cholecystectomy. The patient is a 61-year-old woman with a medical history of fibromyalgia, dyslipidemia, hypothyroidism, obesity and chronic lumbago due to a herniated disc. In another hospital, she had been diagnosed with acute cholecystitis, based on clinical, analytical and ultrasound criteria. Urgent cholecystectomy was performed by a right subcostal laparotomy, with no intraoperative incident. The patient's postoperative recovery was slow, with malaise, progressive oliguria, metabolic acidosis and atrial fibrillation that required administration of vasoactive drugs. High transaminase levels (17800U/l) and a 37% drop in prothrombin time were also observed. CT angiography showed an ischemic lesion in the right liver lobe (RLL) with thrombosis of the right portal branch but did not identify the filiform right hepatic artery (RHA) and left portal branch. With the diagnosis of severe post-cholecystectomy ischemic hepatitis and multiple organ failure, the decision was made to transfer the patient to our hospital for further treatment.
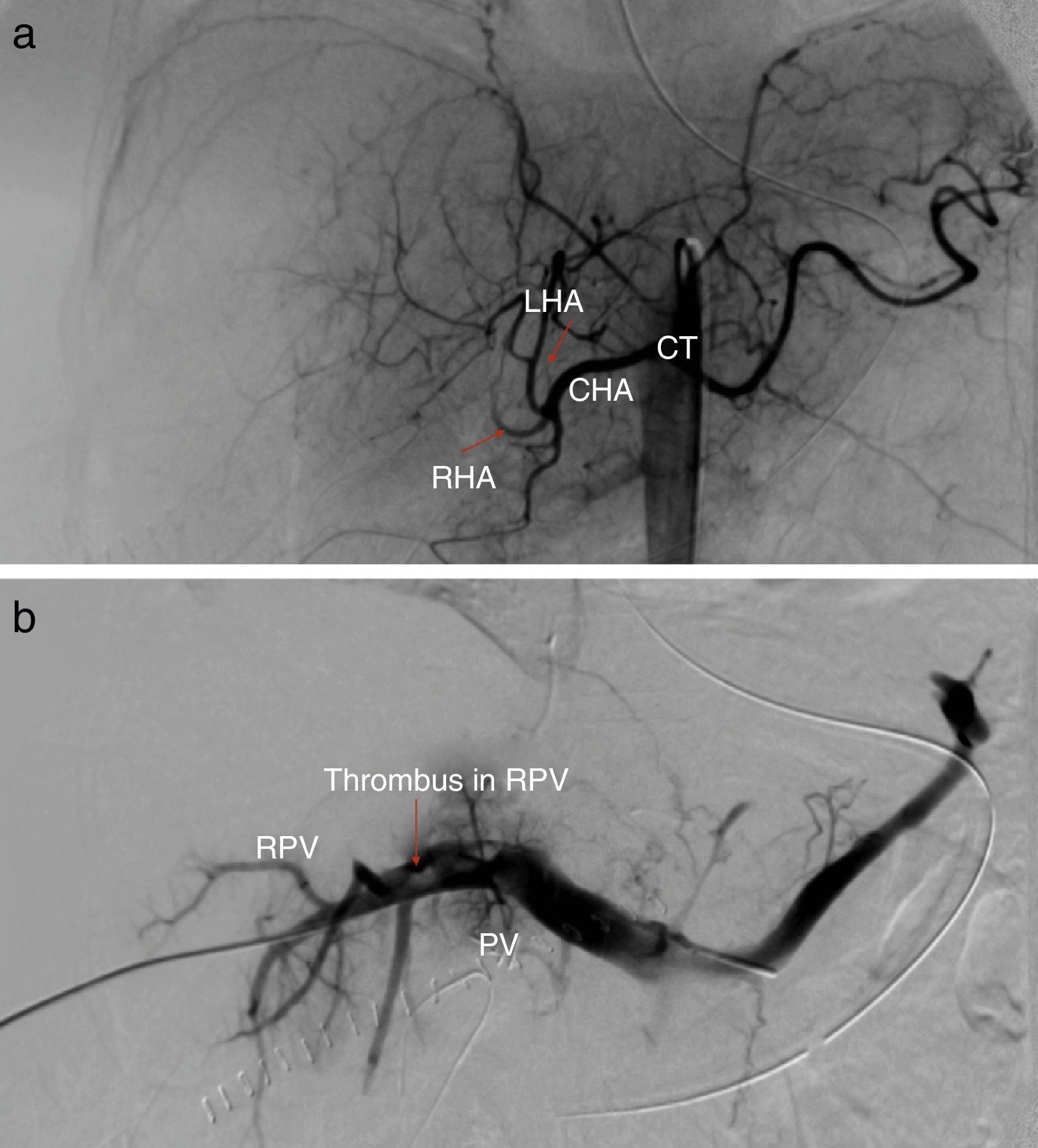
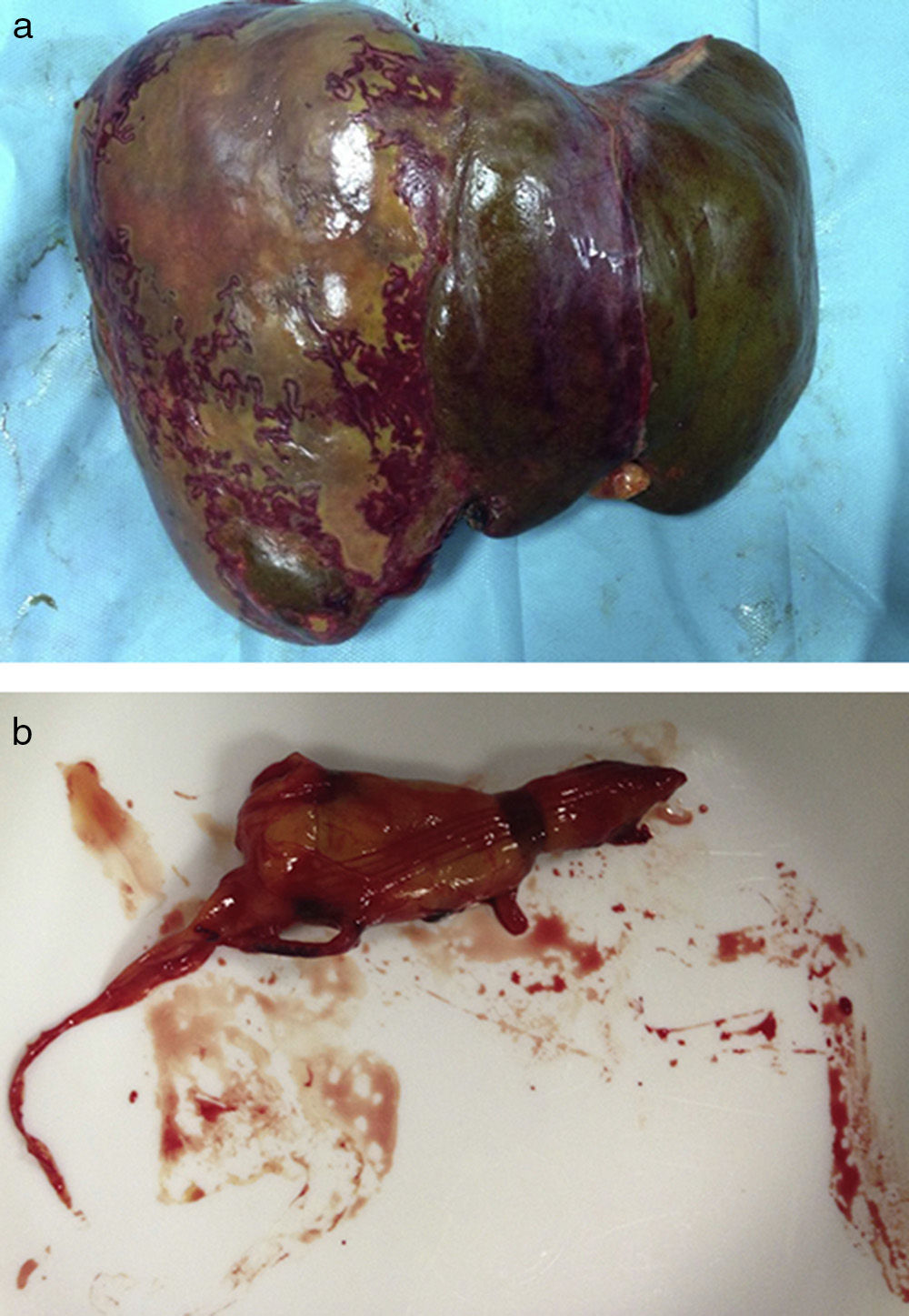
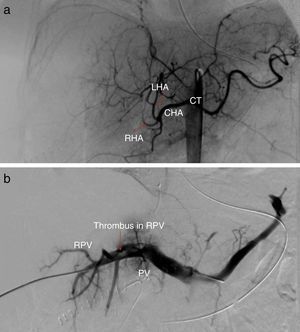
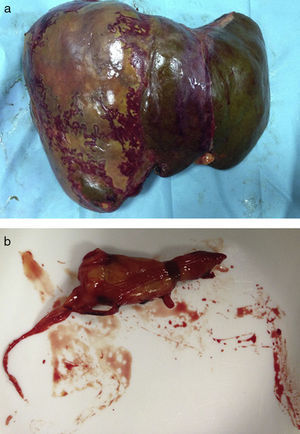
Lab work-up upon admission showed: aspartate aminotransferase 6570IU/l; alanine aminotransferase 5470IU/l; gamma-glutamyl transpeptidase 540IU/l; total bilirubin 3.90mg/dl; alkaline phosphatase 866IU/l; platelets 51×109/l; and prothrombin time 42.2%. Doppler ultrasound showed evidence of a heterogeneous liver in the RLL region, complete thrombosis of the left portal branch, partial thrombosis of the right portal branch, and permeable RHA that was small in caliber and had a low pulsating flow. Given these findings, we carried out transparietal-hepatic portography and hepatic arteriography with mechanical thrombectomy of the right and left portal vein and balloon angioplasty on the left portal vein. Arteriography demonstrated occlusion of the RHA adjacent to surgical clips with absence of right hepatogram (Fig. 1a and b). Follow-up ultrasound 6h after the procedure once again detected thrombosis of the 2 intrahepatic branches of the portal vein and part of the extrahepatic portal vein. Given the situation of hepatic ischemia, transplantation was considered a therapeutic option and code 0 was activated, after having previously ruled out other potential causes of portal thrombosis. Within 48h of being placed on the list, a compatible donor was offered for liver replacement. During surgery, we confirmed the presence of surgical clips in the RHA, the ischemic appearance of the RLL (Fig. 2a) and presence of a thrombus in the main portal vein (Fig. 2b).
The pathology study of the surgical specimen reported the presence of complete bilateral portal thrombosis with extension to smaller intrahepatic branches, thrombosis of the hepatic artery, hepatic ischemic infarction and no evidence of underlying liver disease.
During hospitalization, the patient did not present any surgery-related complications and had adequate liver function when discharged.
In recent years, the progressive use of laparoscopy for gallbladder surgery and the necessary learning curve have increased the number of cases with iatrogenic injuries to the hepatic hilum. Although there are a growing number of cases in laparoscopic cholecystectomy, these incidences may also occur in open surgery. As described by some authors,1,2 vascular lesions are normally associated with biliary duct lesions. A single lesion of the RHA rarely has any clinical significance,3 and the need for liver transplantation for single lesions is rare.4 Less information is available about portal vein injury as it is a structure that is less vulnerable to iatrogenesis.5
The present case report involves injury to the RHA together with bilateral portal thrombosis resulting in severe ischemic hepatitis and multiple organ failure. Intraoperative bleeding during cholecystectomy occasionally involves performing imprecise hemostatic surgical maneuvers that lead to iatrogenic vascular lesions (especially of the portal vein). In general, the therapeutic options for different vascular/biliary injuries depend on their nature and on the associated clinical repercussions. Treatment of surgical lesions to the portal triad should be multidisciplinary and done in hospitals that have experience in liver surgery and transplantation.
Acute liver failure secondary to this type of lesions during cholecystectomy is a very serious complication. The indication for urgent liver transplantation is the context of liver failure with acute coagulopathy and secondary multiple organ failure, with transplantation as the only valid therapeutic option. Although the number of case reports is limited, this affirmation is supported by other authors,6–9 and the recently published series by Parrilla et al.10 on biliary duct lesions is especially interesting. Nonetheless, due to the severe nature of these indications, these situations should be carefully assessed after continuous clinical follow-up in order to choose the right time for transplantation.
Please cite this article as: Ferrer-Fábrega J, Barrufet M, Prado V, Fuster J, García-Valdecasas JC. Trombosis portal asociada a lesión de la arteria hepática derecha durante una colecistectomía: indicación infrecuente de trasplante hepático urgente. Cir Esp. 2015;93:45–46.
The authors of the following article have received no funding or grants, and the article has not been previously presented at congresses.