In spite of being the organ of the body with the second greatest relative arterial perfusion (second only to the suprarenal glands), the thyroid is a rare location for metastases.1,2 In studies carried out in oncology patients, it is an incidental finding in 1.4%–3% of thyroidectomy surgical specimens2–4 and 1.9%–24.2% in necropsy studies.1,3–5 The prevalence, diagnosis and most appropriate management of thyroid metastases continue to be controversial.2
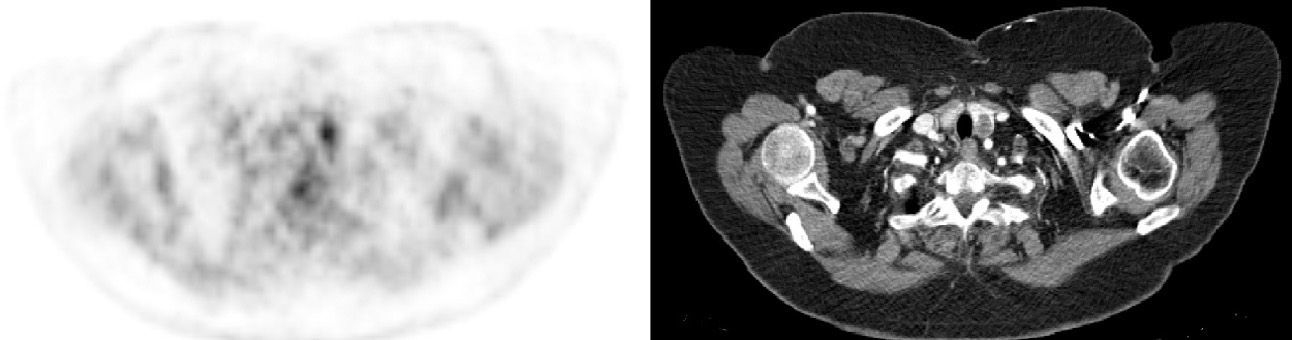
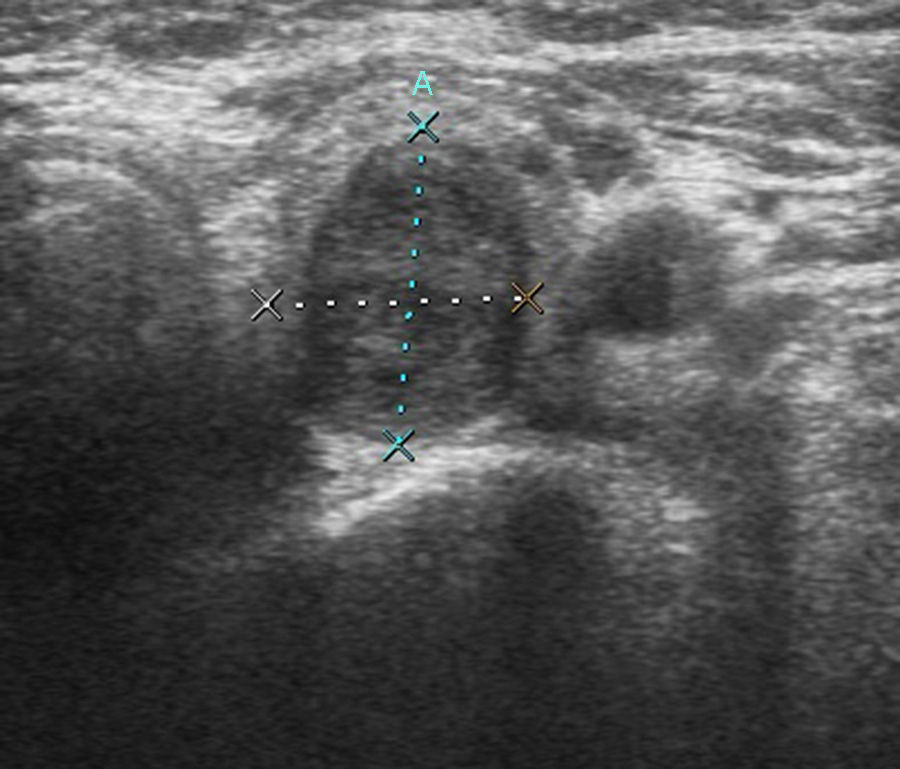
We present the case of a 70-year-old female patient with a history of adenocarcinoma of the sigmoid colon (stage pT3N1b) that had been treated with urgent sigmoidectomy due to perforation. During the extension CT study, the only finding of interest was a hypodense nodule measuring 17mm in the left lobe of the thyroid. The patient initiated adjuvant chemotherapy in accordance with the XELOX regimen. After its completion, re-evaluation with PET-CT once again demonstrated the thyroid nodule with hypermetabolic characteristics (Fig. 1). Given the high suspicion for malignancy, ultrasound-guided fine needle aspiration was performed (Fig. 2), and the results were compatible with a poorly differentiated carcinoma that seemed to be secondary in origin. With this finding, and given the elevated suspicion for secondary thyroid metastasis, total thyroidectomy was performed along with cervical exploration and central lymphadenectomy. The pathology study of the piece reported thyroid nodular infiltration by an adenocarcinoma with a moderate degree of differentiation, compatible with an intestinal primary origin, and negative lymph nodes.
Even though thyroid metastases may appear due to lymphatic as well as vascular dissemination,3 they are uncommon.5,6 There are 2 hypotheses for this phenomenon. One postulates that the rapid blood flow through the gland impedes the tumor cells to adhere,2,3 while the second argues that the high concentrations of oxygen and iodine in the gland would inhibit malignant cell growth.2,6,7 This seems to be confirmed by the higher frequency of this disease in previously pathologic thyroids, especially those affected by goiter or follicular adenomas.2,6
Club (Clear) cell renal carcinomas are the tumors that most frequently metastasize in the thyroid.1–4 These are followed by pulmonary, breast, melanoma, colorectal and sarcomas,2–4,6 although there have been isolated descriptions of several other types, such as: urothelial, bladder, testicular seminomas, endometrial, ovarian, carcinosarcoma, neuroendocrine tumors, meningioma, GIST, nasopharyngeal and pancreatic mucinous tumors. In the autopsy series, the most common tumor was pulmonary, followed by breast and melanoma.2
Mean age at presentation of thyroid metastases is 60, and there is a greater prevalence in women.2,3 The incidence is on the rise due to the wider use of imaging tests such as PET-CT and ultrasound.2,3,7
Thyroid metastases can be found decades after the appearance of the primary tumor. Mean interval at presentation is 53 months, although presentation may also be synchronous.2,6 This disease is commonly associated with other metastatic lesions in other locations.6
40% of thyroid metastases are solitary.2,4 When they are multicentric, they usually infiltrate and substitute the thyroid tissue, surpassing the capsule and causing a worse prognosis.4 Most patients are euthyroid at diagnosis.2,3,5 The appearance of hypothyroidism is usually due to massive infiltration of the gland, while thyrotoxicosis is secondary to a neoplastic embolization that triggers glandular damage and massive dumping of hormones into the blood.2 The most frequent extra-thyroid symptoms are: dysphagia, stridor, cough, hoarseness or a palpable mass.1,2 When thyroid metastasis causes clinical symptoms, long-term patient survival becomes drastically reduced.1 Nonetheless, the clinical progression of these patients mostly depends on whether the tumor has disseminated to other locations.2,3,6
Most thyroid metastases are not detected clinically but instead as part of the follow-up studies for oncology patients. The finding is generally incidental.1,5 Although primary thyroid tumors are more frequent,6 the appearance of a thyroid nodule in a cancer patient requires ruling out this disease using cytology,5 and ultrasound-guided fine needle aspiration is the initial study.1,4 This technique may not provide a definitive diagnosis in 13%–24% of cases, which generally occurs when the sample is inadequate.2,6 Immunohistochemistry is generally able to differentiate between a primary thyroid tumor or one of metastatic origin thanks to thyroglobulin; this may fail, however, in anaplastic thyroid tumors.2–5 When the needle aspiration is negative or indeterminate, surgical excision is the most appropriate management for the diagnosis of these patients.2
Although there is not a clear consensus about which surgical technique to perform,1 early surgical treatment has been demonstrated to increase survival by preventing local recurrence and complications such as thyrotoxicosis, airway compression and infiltration of local structures such as the recurrent nerve, for instance.1,2,5
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Sagarra Cebolla E, Rodriguez-Bachiller Villaronga L, Carrasco Muñoz S, Morales Taboada ÁG, García Sabrido JL. Metástasis tiroidea por adenocarcinoma de colon. Cir Esp. 2015;93:43–44.