The objectives of this study were to investigate the relationship between several factors and the incidence of postoperative abdominal wall dehiscence (POAD), and to estimate the influence of POAD on in-hospital mortality, excess length of stay and costs.
MethodsRetrospective observational study of a sample of abdominal surgery patients from a minimal basic data set of 87 Spanish hospitals during 2008–2010.
ResultsAmong 323894 admissions for abdominal surgery reviewed there were 2294 patients with POAD. Elderly patients, male, with non-elective admission, with alcohol, tobacco or drugs abuse, and with more comorbidities had higher incidence. POAD patients had an increase in in-hospital death (mortality excess of 107.5%), excess length of stay (15.6 days) and higher cost (14327 euros).
ConclusionsCertain demographic and behavioural variables, and several comorbidities are associated with the incidence of POAD, and this complication shows an increase in in-hospital mortality, the length of hospital stay and costs. Preventive measures might decrease the incidence of POAD and its impact on health and extra-costs.
Los objetivos de este estudio fueron el análisis de los factores asociados a la incidencia de dehiscencia postoperatoria de la laparotomía (DPL) y el impacto de esta última en la mortalidad, las estancias y los costes hospitalarios.
MétodosEstudio observacional retrospectivo de una muestra de pacientes intervenidos mediante laparotomía recogidos en los conjuntos mínimos básicos de datos de 87 hospitales españoles durante el periodo 2008–2010.
ResultadosSe estudiaron 323.894 ingresos por cirugía abdominal, entre los cuales hubo 2.294 pacientes con DPL. Los pacientes de mayor edad, varones, con ingreso urgente, con trastornos por alcohol, tabaco y drogas, y con más comorbilidades presentaron mayor incidencia. Además, aquellos con DPL presentaron un incremento de mortalidad (107,5%), una estancia mas prolongada (15,6 días) y un exceso de costes (14.327 euros).
ConclusionesHay una asociación entre ciertas variables demográficas, conductuales y comorbilidades, y la incidencia de DPL, y esta complicación aumenta la mortalidad, la duración de la estancia y su coste. Medidas preventivas podrían disminuir su incidencia y su impacto sanitario y económico.
Postoperative wound dehiscence (PWD) is a serious complication, with an incidence of 0.4%–3.5%,1–8 which associates high rates of complications and mortality.3–9 Despite the advances in anaesthesia and perioperative care, the incidence, morbidity and mortality associated remain stable, probably due to the increase in the prevalence of related risk factors among the surgical population.5
The Agency for Healthcare Research and Quality (AHRQ) includes the rate of postoperative dehiscence of the abdominal wall as one of the patient's safety markers,10 which has also been adopted in other countries, such as Spain. This rate is calculated using databases of discharges from the hospital in the USA and the minimum sets of databases in Spain (CMBD in Spanish). Despite the relevance of this complication, we have not found any studies carried out on the impact of this specific marker by AHRQ on the morbidity and mortality and the health care and economic burden among patients with abdominal surgery.
Therefore, for the purposes of analysing the risk factors of PWD upon admission to the hospital, we have studied the issue in patients 18 years of age or older admitted using a sample of 87 Spanish hospitals during the period 2008–2010, trying to control other confounding and interaction variables such as age, gender, type of hospital, addictions and a considerable number of comorbidities. Similarly, another purpose of this study is to analyse the potential influence of this complication on mortality, the extension of stays and the excess costs among patients hospitalised for abdominal surgery.
MethodsType of Study, Sample and ParticipantsRetrospective observational study in a sample of Spanish hospitals.
For the sample to be representative at a national and autonomic level, and taking into consideration the stratification of hospitals according the classification of groups of hospitals based on their size and complexity of the Ministry of Health,11 a multistage sampling was performed, and 87 Spanish hospitals of all Spanish CCAAs were selected, which are listed in Appendix.
Based on this written or digitalised summary of the medical history, the diagnoses of each patient and the procedures applied are codified based on the rules of the 9th Revision of the International Classification of Diseases in the Causes of Death Lists (CIE9). The coding and entering of information into the database was carried out by specialists in data recording. These databases of discharges from the hospital or CMBD contain information on the hospital providing the care, demographic data of the patient (date of birth and gender), dates of admission and discharge, type of admission and type of discharge. For the diagnoses of the main cause and secondary diagnoses, external causes and procedures, the CIE9 codes are used. These databases also include groups related with the diagnosis (GRD) and each hospital is classified in a group based on its size and complexity of care.11 The analysis was limited to patients who were 18 years of age or older on discharge.
VariablesFollowing the definition of the AHQR, cases of PWD were defined as those with procedure code 54.61 of the CIE9 (“Abdominal wall disruption closure [evisceration]”). Following the related criteria, cases with stays of less than 2 days, obstetric cases and cases among immunocompromised patients were excluded. All patients with abdominal surgery and no PWD who also met the criteria above were included as a comparison group. We used the CIE9 codes for the 386 abdominal and pelvic surgery procedures described by the AHRQ in its technical specifications.10 The age was stratified into the following groups: 18–34, 35–44, 45–54, 55–64, 65–74, 75–84 and 85 years or over. A considerable group of comorbidities was identified (shown in Table 1) using the CIE9 codes proposed by Quan et al.12 The CIE9 codes were used to define disorders caused by abuse of alcohol, tobacco and other drug addictions.13
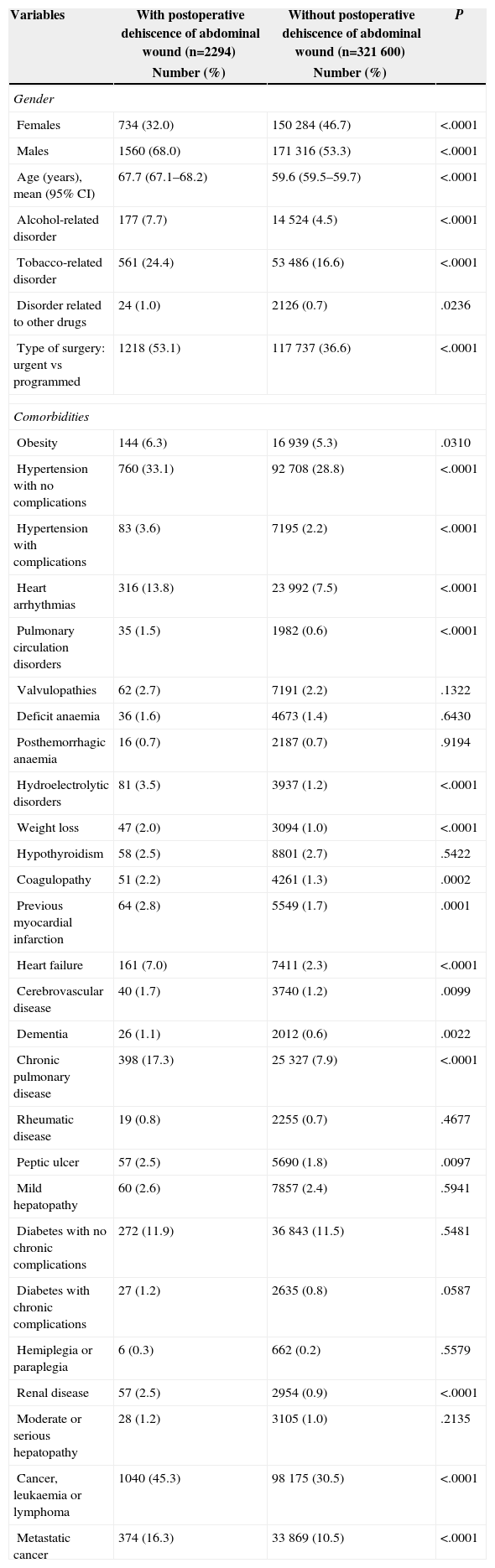
Characteristics of Patients With and Without Postoperative Dehiscence of Abdominal Wound.
| Variables | With postoperative dehiscence of abdominal wound (n=2294) | Without postoperative dehiscence of abdominal wound (n=321600) | P |
|---|---|---|---|
| Number (%) | Number (%) | ||
| Gender | |||
| Females | 734 (32.0) | 150284 (46.7) | <.0001 |
| Males | 1560 (68.0) | 171316 (53.3) | <.0001 |
| Age (years), mean (95% CI) | 67.7 (67.1–68.2) | 59.6 (59.5–59.7) | <.0001 |
| Alcohol-related disorder | 177 (7.7) | 14524 (4.5) | <.0001 |
| Tobacco-related disorder | 561 (24.4) | 53486 (16.6) | <.0001 |
| Disorder related to other drugs | 24 (1.0) | 2126 (0.7) | .0236 |
| Type of surgery: urgent vs programmed | 1218 (53.1) | 117737 (36.6) | <.0001 |
| Comorbidities | |||
| Obesity | 144 (6.3) | 16939 (5.3) | .0310 |
| Hypertension with no complications | 760 (33.1) | 92708 (28.8) | <.0001 |
| Hypertension with complications | 83 (3.6) | 7195 (2.2) | <.0001 |
| Heart arrhythmias | 316 (13.8) | 23992 (7.5) | <.0001 |
| Pulmonary circulation disorders | 35 (1.5) | 1982 (0.6) | <.0001 |
| Valvulopathies | 62 (2.7) | 7191 (2.2) | .1322 |
| Deficit anaemia | 36 (1.6) | 4673 (1.4) | .6430 |
| Posthemorrhagic anaemia | 16 (0.7) | 2187 (0.7) | .9194 |
| Hydroelectrolytic disorders | 81 (3.5) | 3937 (1.2) | <.0001 |
| Weight loss | 47 (2.0) | 3094 (1.0) | <.0001 |
| Hypothyroidism | 58 (2.5) | 8801 (2.7) | .5422 |
| Coagulopathy | 51 (2.2) | 4261 (1.3) | .0002 |
| Previous myocardial infarction | 64 (2.8) | 5549 (1.7) | .0001 |
| Heart failure | 161 (7.0) | 7411 (2.3) | <.0001 |
| Cerebrovascular disease | 40 (1.7) | 3740 (1.2) | .0099 |
| Dementia | 26 (1.1) | 2012 (0.6) | .0022 |
| Chronic pulmonary disease | 398 (17.3) | 25327 (7.9) | <.0001 |
| Rheumatic disease | 19 (0.8) | 2255 (0.7) | .4677 |
| Peptic ulcer | 57 (2.5) | 5690 (1.8) | .0097 |
| Mild hepatopathy | 60 (2.6) | 7857 (2.4) | .5941 |
| Diabetes with no chronic complications | 272 (11.9) | 36843 (11.5) | .5481 |
| Diabetes with chronic complications | 27 (1.2) | 2635 (0.8) | .0587 |
| Hemiplegia or paraplegia | 6 (0.3) | 662 (0.2) | .5579 |
| Renal disease | 57 (2.5) | 2954 (0.9) | <.0001 |
| Moderate or serious hepatopathy | 28 (1.2) | 3105 (1.0) | .2135 |
| Cancer, leukaemia or lymphoma | 1040 (45.3) | 98175 (30.5) | <.0001 |
| Metastatic cancer | 374 (16.3) | 33869 (10.5) | <.0001 |
The main purpose was to calculate the risk of PWD among patients with abdominal surgery. The secondary purposes were to determine mortality, duration of the stay and hospital costs in patients with and without that complication. We calculated costs using specific hospital costs for each GRD stratified according to the group of hospitals, based on the estimations published by the Ministry of Health for years 2008–2010.11
An unvaried analysis was carried out to analyse the relation between PWD and age, gender, type of admission (urgent vs scheduled), addiction disorders and comorbidities. Then, multivariate models were prepared using the analysis of unconditional logistic regression to determine the association of these variables on the incidence of PWD, and it was determined that statistical significance was <0.001 due to the size of the sample. A multivariate analysis was carried out on covariance to determine the effect of the PWD on in-hospital mortality, the stay in days and costs in patients of abdominal surgery. The data were adjusted based on age, gender, type of admission, addictions, the group of hospitals and severity of the patient's condition, using the comorbidities stated above, and also a statistical significance of at least <0.001 was set. The analysis was carried out using the statistical software STATA, version MP 13.1.
ResultsCharacteristics of the PatientsA total of 323894 patients treated with abdominal surgery were identified, of which 2294 (0.71%) presented PWD. The characteristics of patients with and without DPOA are listed in Table 1. Patients with PWD were older (mean age of 67.7 years), mainly males (68%), with a higher urgent admissions rate (53.1%) and with higher prevalence of addictions, especially tobacco (24.4%) and alcohol (7.7%). There was also a higher prevalence in many of the comorbidities studied.
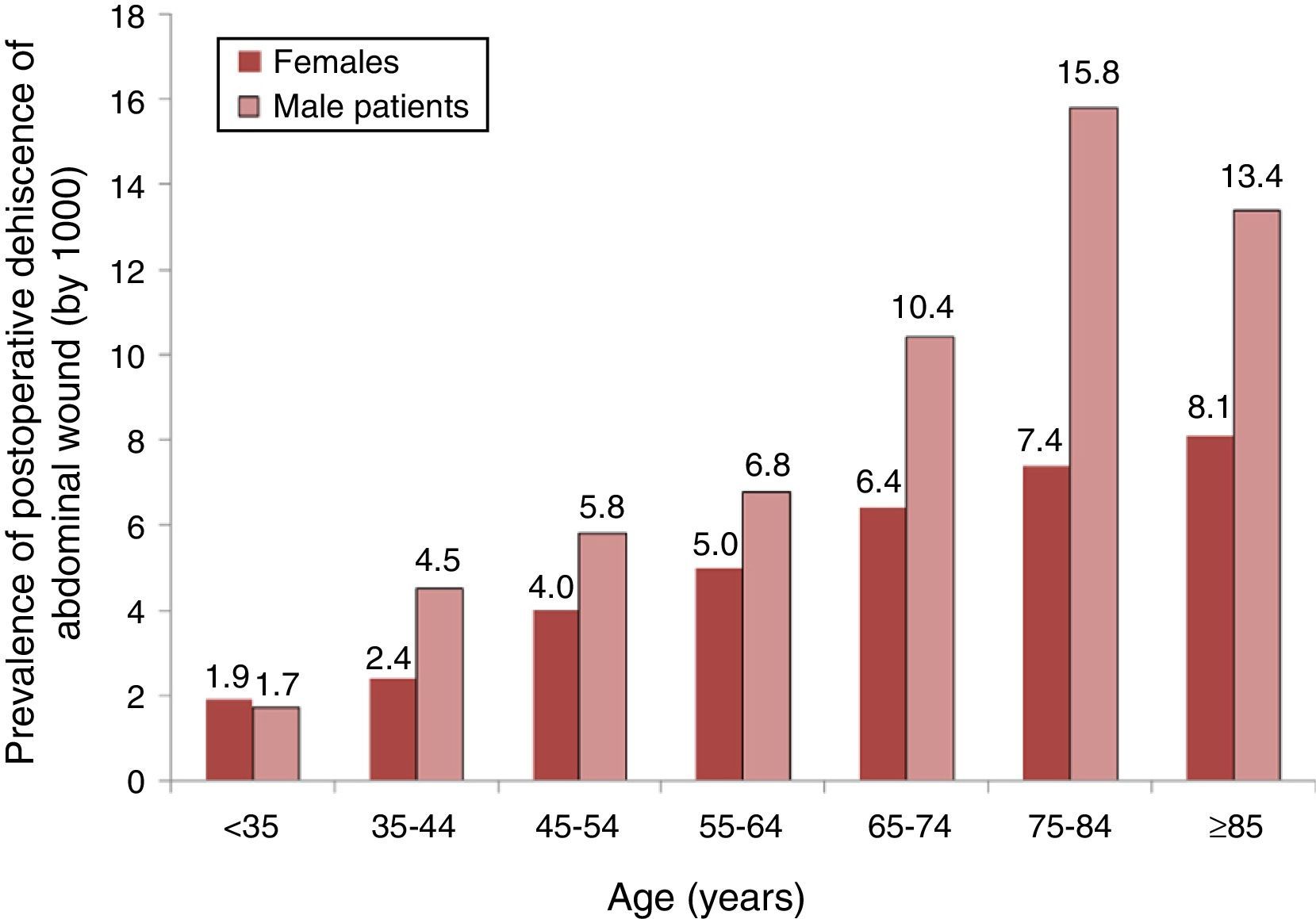
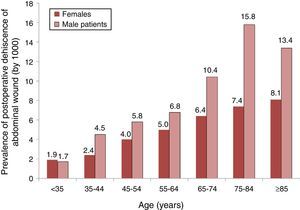
An analysis of the distribution of the prevalence of PWD (by 1000) according to groups of age and gender is shown in Fig. 1, were we can see that the prevalence increased with age in both genders but, from 35 years onwards, there was a higher prevalence among males.
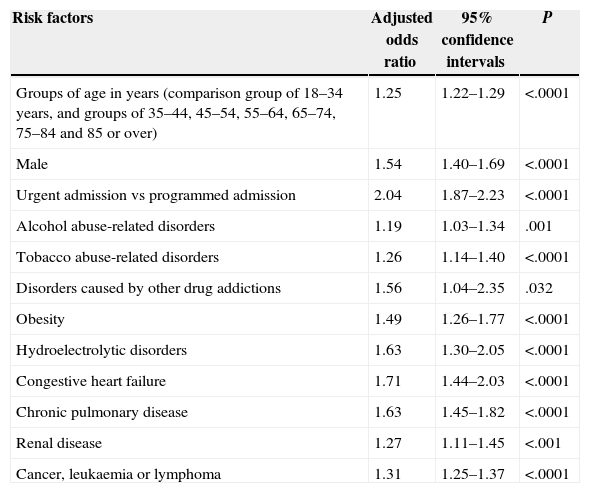
Risk of Postoperative Dehiscence of the Abdominal Wound or ScarTable 2 shows the results of the multivariate analysis and we can see that the risk factors are still age, male gender, urgent admission vs scheduled admission, alcohol abuse disorders, abuse of tobacco and other drug addictions, obesity, admission with hydroelectrolytic disorders, arrhythmias, congestive heart disease, renal disease and cancer.
Logistic Regression Model for Postoperative Dehiscence of Abdominal Wound Among Patients With Abdominal Surgery in Patients 18 Years of Age or Older Meeting the Inclusion and Exclusion Criteria of the AHRQ.
| Risk factors | Adjusted odds ratio | 95% confidence intervals | P |
|---|---|---|---|
| Groups of age in years (comparison group of 18–34 years, and groups of 35–44, 45–54, 55–64, 65–74, 75–84 and 85 or over) | 1.25 | 1.22–1.29 | <.0001 |
| Male | 1.54 | 1.40–1.69 | <.0001 |
| Urgent admission vs programmed admission | 2.04 | 1.87–2.23 | <.0001 |
| Alcohol abuse-related disorders | 1.19 | 1.03–1.34 | .001 |
| Tobacco abuse-related disorders | 1.26 | 1.14–1.40 | <.0001 |
| Disorders caused by other drug addictions | 1.56 | 1.04–2.35 | .032 |
| Obesity | 1.49 | 1.26–1.77 | <.0001 |
| Hydroelectrolytic disorders | 1.63 | 1.30–2.05 | <.0001 |
| Congestive heart failure | 1.71 | 1.44–2.03 | <.0001 |
| Chronic pulmonary disease | 1.63 | 1.45–1.82 | <.0001 |
| Renal disease | 1.27 | 1.11–1.45 | <.001 |
| Cancer, leukaemia or lymphoma | 1.31 | 1.25–1.37 | <.0001 |
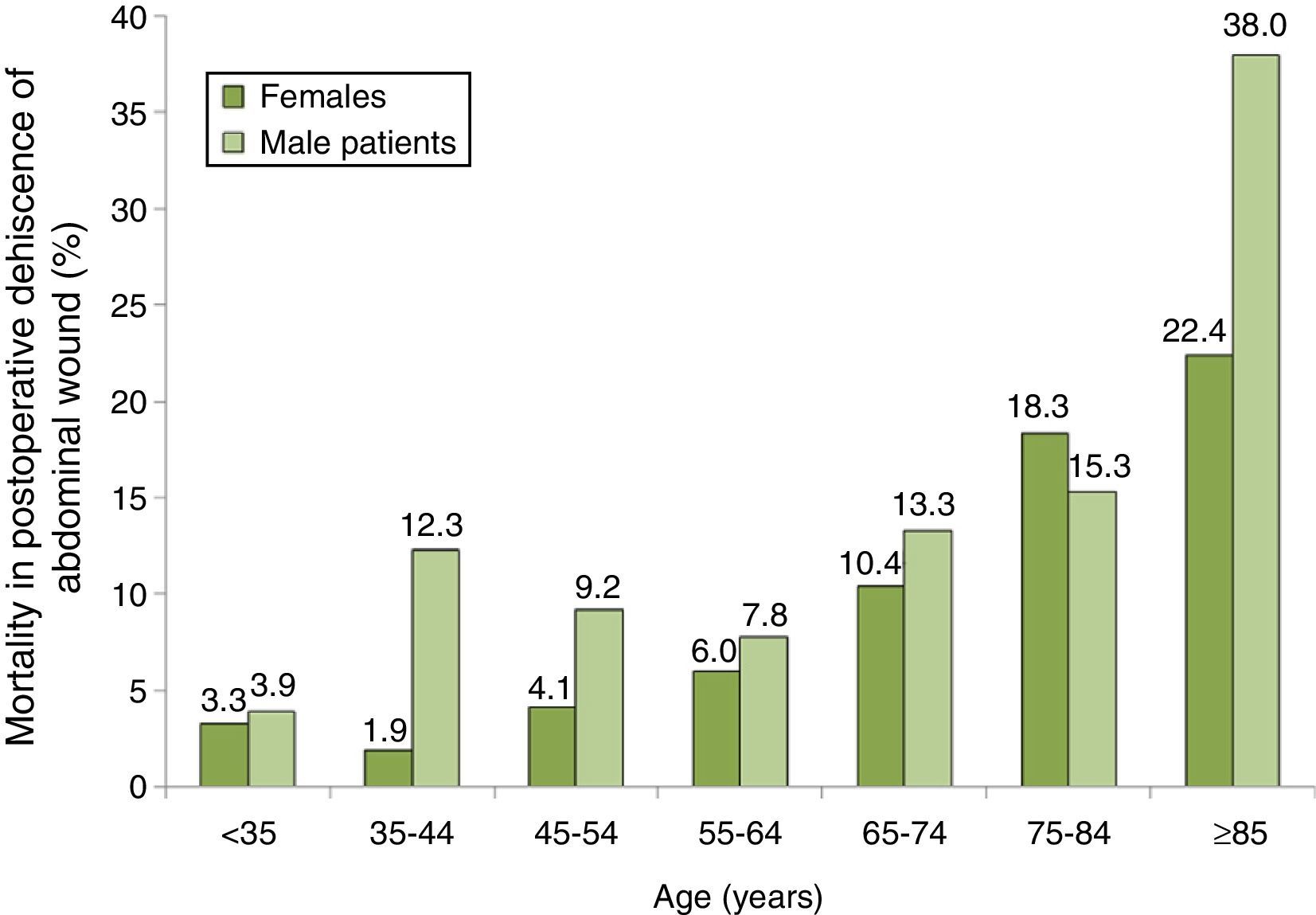
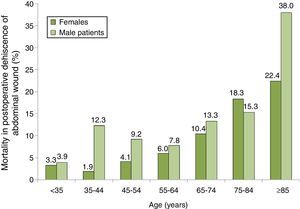
The distribution of mortality among patients with PWD according to their age and gender group is shown in Fig. 2, where we can see a progressive increase in mortality, especially among men. The group with the highest mortality was that of males 85 years or older with PWD, who had a mortality rate of 38.0%.
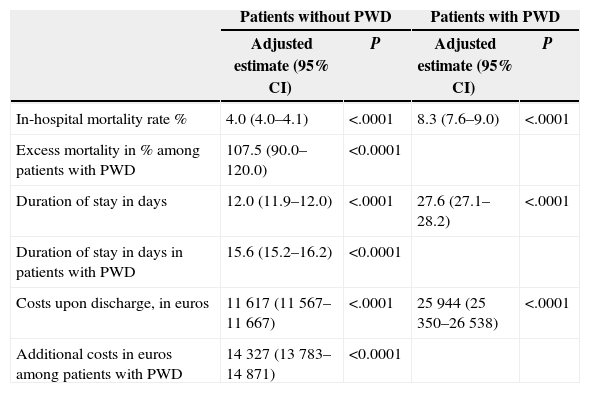
The multivariate analysis of covariance, which included age, gender, hospital group, type of admission, and all addictions and comorbidities mentioned above, is shown in Table 3, and demonstrated that among patients with abdominal surgery, those with PWD had an extraordinary excess of mortality, with an adjusted rate of 4.0% among those who did not have PWD and 8.3% among those who did: that is to say, a 2.1:1 ratio. Patients with PWD had a mean duration of stay of 15.6 days and an excess of costs of 14327 euros per discharge.
Excess of Mortality, Extension of Stays and Additional Costs Caused by Abdominal Postoperative Dehiscence Among Patients With Abdominal Surgery. Values Adjusted to the Multivariate Analysis of Covariance.
| Patients without PWD | Patients with PWD | |||
|---|---|---|---|---|
| Adjusted estimate (95% CI) | P | Adjusted estimate (95% CI) | P | |
| In-hospital mortality rate % | 4.0 (4.0–4.1) | <.0001 | 8.3 (7.6–9.0) | <.0001 |
| Excess mortality in % among patients with PWD | 107.5 (90.0–120.0) | <0.0001 | ||
| Duration of stay in days | 12.0 (11.9–12.0) | <.0001 | 27.6 (27.1–28.2) | <.0001 |
| Duration of stay in days in patients with PWD | 15.6 (15.2–16.2) | <0.0001 | ||
| Costs upon discharge, in euros | 11617 (11567–11667) | <.0001 | 25944 (25350–26538) | <.0001 |
| Additional costs in euros among patients with PWD | 14327 (13783–14871) | <0.0001 | ||
In several studies, the risk factors for PWD were analysed,1–4,8 predictive models have been prepared and validated,2,5–7 and their impact on postoperative mortality has been studied.3–9 In Spain, excellent scientific articles have been published on the incidence, risk factors, validation of predictive models and mortality of this postsurgical complication.4,7,8
We were surprised by the lack of studies of this complication as a safety marker of AHRQ for the patient. In the USA, it has been proven that the PWD marker has an excellent positive predictive value14 and its use has been recommended as a tool to measure compliance with the safety rules for surgical patients.14,15 We also found an absence of analysis on the impact of this marker in the excess mortality, the extension of stays and related additional costs.
We have limited the analysis to the variables applicable upon admission of the patient. Our results join those of many others on the importance of age, gender, type of admission, addictions and several comorbidities as risk factors of this complication. In the case of alcohol abuse disorders, our results match those of studies carried out in Spain and other countries mentioned above, justified by the impact of ethanol on the immune status of the surgical patient.16,17 Results also match for issues related to the use of tobacco, associated to the highest rate of postsurgical side effects.18,19 Other risk factors such as obesity, dehydration and chronic heart, pulmonary, renal and oncological diseases have been widely described in the reviews of this complication,2,3 and in the studies published in Spain.4,7,8
Our results indicate that this complication has an overwhelming impact on hospital mortality, with an excess of mortality of 107.5%, an undue extension of the stay of 15.6 days and an additional cost of 14327 euros.
Our study has several limitations. The data we have used are exclusively those stated in the CMBD, and were not supplemented with additional data about the patients. During the entire study we have used definitions of addiction disorders, PWD and the comorbidities as assigned by doctors in each centre, and codified and entered into the database by coders. Another limitation is the potential loss of information due to the fact that not all the data necessary for coders to fill out these codes or due to variability in the interpretation by coders appear on the patient's medical history. The strict inclusion and exclusion criteria for this marker of AHRQ eliminate all patients with a stay of less than 2 days, those with immunosuppression and obstetric patients, which may affect comparisons with other series.
Databases such as CMBD also have clear advantages. The data gathered are usually recorded in all hospital discharges and, by including all cases, they provide quite precise estimates of incidence, prevalence, comorbidities and mortality of diseases assisted at hospitals.20,21 These data can be analysed retrospectively, unlike other designs which required the collection of prospective information. Data collection for long periods and with a large number of patients, such as in this study, can be made relatively quickly and easily, and as the data are systematically collected, the reduction of costs is significant. In these studies there may be less selection biases, such as those caused by the refusal of patients or their legal representatives to sign consent and participate in the study.
Given the size of the sample and the diversity of hospitals, these results can be generalised and are not limited to patients admitted into one or a few hospital centres. The availability of costs for each GRD stratified by the groups of hospitals and for each year makes calculation of cost excesses for PWD easier. As far as we know, this is the first study calculating the excess of mortality, the extension of stays and the excess of costs attributable to PWD controlling a considerable number of variables upon admission.
Based on the results, a large number of preventive measures can be inferred, and not only those oriented to the importance of a proper surgical technique22 (including the prevention of infections23), but also others which are very important in the preoperative period, such as the control of weight and the patient's nutritional status, and abstinence from tobacco,24 alcohol25 and other drugs, and from brief advice to transfer to rehabilitation centres if necessary. All these measures contribute to a decrease in the excess of mortality in these patients, to improve their quality of life after discharge (decreasing the burden of problems suffered by patients and their families), and to make more efficient use of health resources.
FundingThis study was funded with the aid of: (a) Subventions for the funding of Biomedical Research and Healthcare Sciences in Andalucía for the year 2013. Health and Social Affairs Department of the Board of Andalucía (PI−0271-2013), and (b) Governmental Department for the National Drugs Plan (Aid 2009I017, Project G41825811).
Conflict of InterestThe authors declare that there are no conflicts of interest.
Please cite this article as: Gili-Ortiz E, González-Guerrero R, Béjar-Prado L, Ramírez-Ramírez G, López-Méndez J. Dehiscencia de la laparotomía y su impacto en la mortalidad, la estancia y los costes hospitalarios. Cir Esp. 2015;93:444–449.