In 2018, a group of surgeons and students from the Cardenal Herrera CEU University (UCHCEU) organized the MEDIPINAS2018 medical-surgical mission at the Santa Maria Josefa Hospital Foundation for patients without resources in Iriga City, Philippines. Outpatients were briefly instructed in postoperative care, and nursing staff did not provide wound care. A general surgeon visited the cases with complications. however, 25 (28.8%) of the 87 patients developed surgical wound infection (SSI), which is a very high rate compared to the 11% published by the WHO for low- and moderate-income countries1.
We reviewed the hospital’s infection prevention and surgical material sterilization protocols, which were correct. We found that the factors involved in the unusual rate of infection included the lack of knowledge of the population to correctly care for wounds, as well as the lack of clean water and basic material for wound care. It seemed necessary to adapt our protocols to the country and its social and sanitary conditions2. The strategies described in surgical infection prevention guidelines can prevent 60% of SSI3,4; therefore, we created an SSI prophylaxis project to apply in MEDIPINAS2019. The MEDIPINAS2019 surgical mission incorporated the “Recommendations for Zero Surgical Infection”, with the necessary modifications for it to function in a hospital with limited resources. Specifically, these included: intensified handwashing, the use of 2% alcoholic chlorhexidine with a swab to prepare the surgical field, and glycemic control in diabetic patients. Antibiotic prophylaxis was administered in clean-contaminated and contaminated surgery.
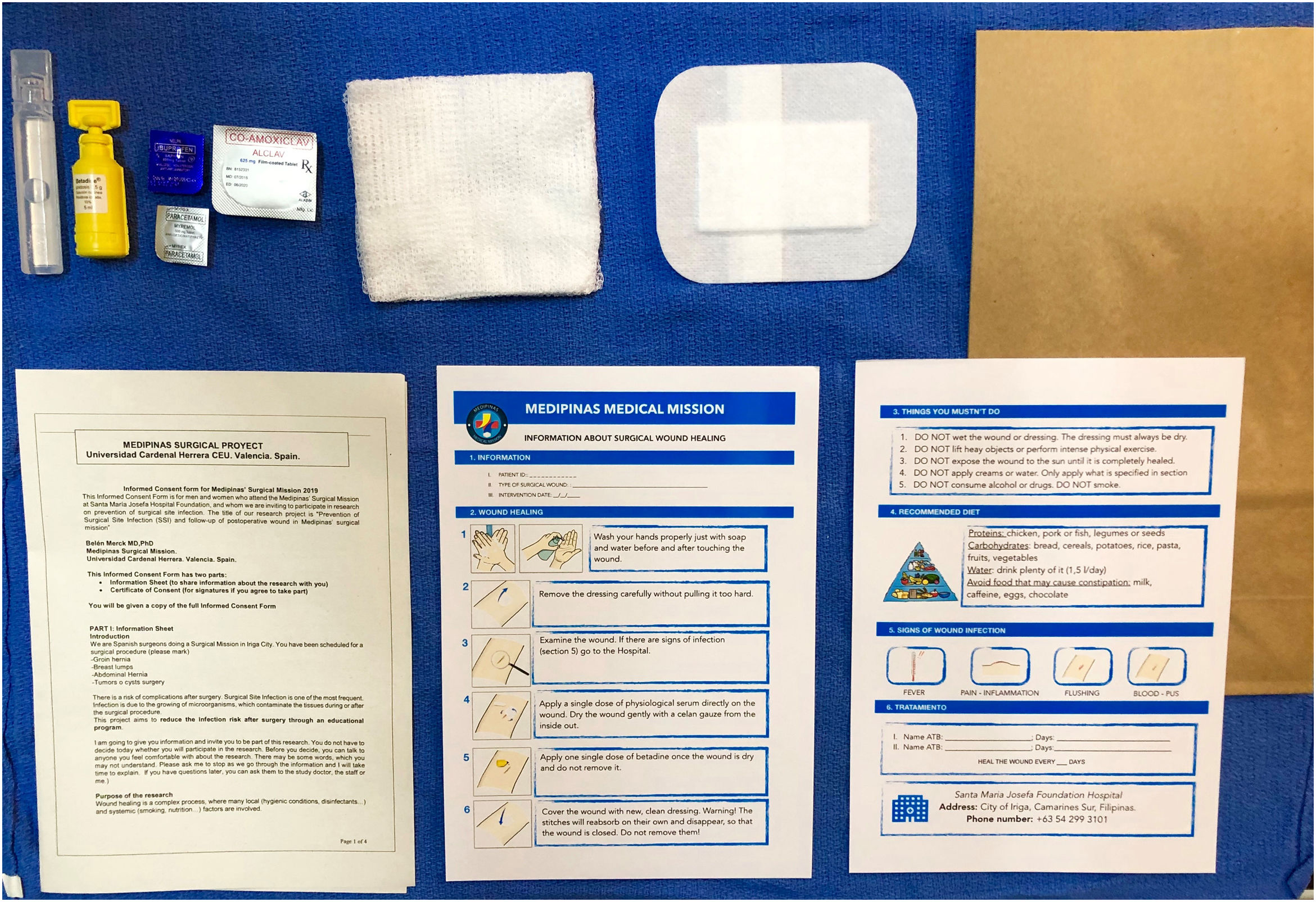
We designed a prospective study including patients who agreed to participate after being informed and signing an informed consent from in accordance with the WHO model. We created an information sheet, which was given to each patient after surgery. It explained surgical wound care and the warning signs of SSI. In addition, patients were given material for dressings (Fig. 1), analgesics (paracetamol, ibuprofen) and antibiotics for the treatment of the infection in those cases in which it was necessary, and healthcare education was provided.
An Apple® Numbers® spreadsheet application was used to follow the evolution of the surgical wound, which collected the patients’ clinical data as well as photographs of the surgical area before the incision, at the end of the operation and during check-ups. The use of a color code of the final state of the wound completed by Filipino nurses (green: not infected; yellow: resolved infection; red: active infection) (Fig. 2) facilitated the follow-up and treatment of each case. The ability to easily collect patient data and images during the various phases of surgical wound healing has been instrumental in cooperating with our Filipino colleagues. Although the use of the app for surgery and cooperation is not new5, the MEDIPINAS app stands out for having been created for a specific project, with minimal development cost and complexity. This project was approved by the Ethics Committee of the College of Health Sciences of the UCHCEU.
In MEDIPINAS2019, 108 patients were included, and 10 (9.7%) developed SSI. When we compared the results with MEDIPINAS2018, there were no significant differences in mean age, gender or type of interventions, but there were differences (P < .001) for SSI infection with a decrease of 19.1% in MEDIPINAS2019.
MEDIPINAS was created in 2016 to provide surgical treatment for patients who do not have access to surgery due to lack of resources or surgical specialists6. For the collaboration to succeed, one must avoid creating problems, as otherwise ‘the remedy is worse than the disease’7. Therefore, surgeries must be planned with consideration of the limitations in the area. In these rural areas, it is customary to consult with a healer for medical problems, which is cheaper than going to a doctor or a pharmacy. In the past, the use of hot infusions of leaves or herbs was shown to be detrimental to the surgical wounds of patients treated by our group. Medical professionals who participate in volunteer projects in other countries must be very respectful of local customs but must also provide patients with timely education8. We emphasized hand hygiene and wound cleaning, and it was essential to provide our patients with the material since most could not afford it. With this approach, we managed to reduce the SSI rate to less than 11%, which was our objective1. The app, which is very easy to use, contributed towards the collaboration with our Filipino colleagues.
In short, the application of the “Recommendations for Zero Surgical Infection” and the education of patients regarding how to clean the wound, providing material to treat the wound, together with the follow-up of nursing staff through visits and wound care when necessary, as well as the distant follow-up through the app, have all contributed to the lower rate of SSI in our series.
FundingThe MEDIPINAS Project was financed in 2019 with the Collaboration Grant from the Spanish Association of Surgeons (no ID, therefore not included on the platform), with contributions from the Universidad Cardenal Herrera CEU and, especially, many small contributions from individuals.
Please cite this article as: Merck B, Henarejos Pérez V, Villalonga Morales A, Barrasa Shaw A. Prevención de la infección del sitio quirúrgico mediante la educación de los pacientes: resultados de la misión médica MEDIPINAS. Cir Esp. 2022;100:247–249.