Delirium is a frequent complication in elderly patients after urgent abdominal surgery.
MethodsProspective study of consecutive patients aged ≥ 65 years who had undergone urgent abdominal surgery from 2017−2019. The following variables were recorded: age, sex, ASA, physiological state, cognitive impairment, frailty (FRAIL Scale), functional dependence (Barthel Scale), quality of life (Euroqol-5D-VAS), nutritional status (MNA-SF), preoperative diagnosis, type of surgery (BUPA Classification), approach and diagnosis of postoperative delirium (Confusion Assessment Method). Univariate and multivariate analyses were performed to analyze the correlation of these variables with delirium.
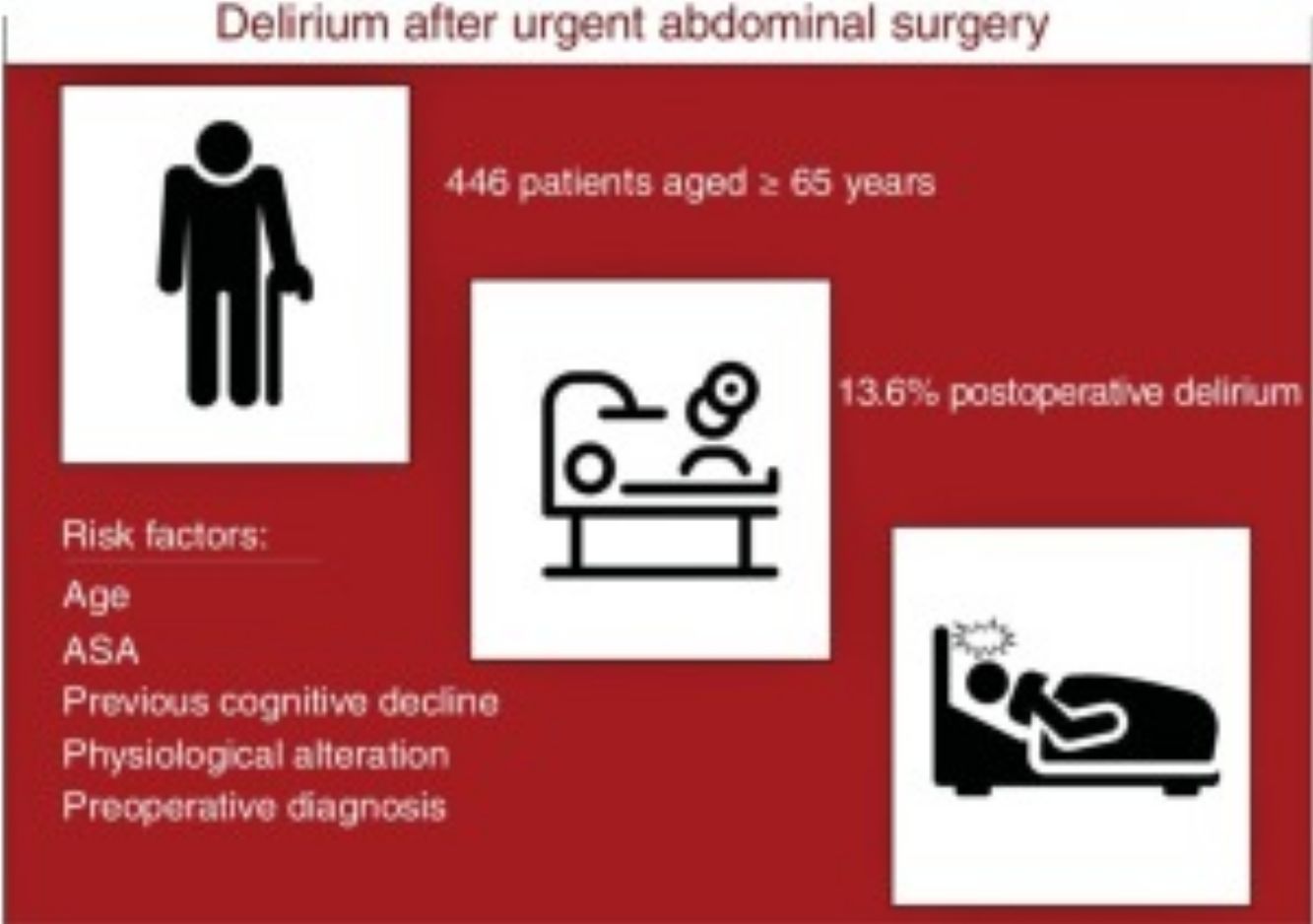
ResultsThe study includes 446 patients with a median age of 78 years, 63.6% were ASA ≥ III and 8% had prior cognitive impairment. 13.2% were frail and 5.4% of the patients had a severe or total degree of dependence. 13.6% developed delirium in the postoperative period. In the univariate analysis, all the variables were statistically significant except for sex, type of surgery (BUPA) and duration. In the multivariate analysis the associated factors were: age (P < .001; OR: 1,08; 95% CI: 1,038-1,139), ASA (P = .026; OR: 3.15; 95% CI: 1.149-8.668), physiological state (P < .001; OR: 5.8; 95% CI: 2.176-15.457), diagnosis (P = .006) and cognitive impairment (P < .001; OR: 5.8; 95% CI: 2.391-14.069).
ConclusionThe factors associated with delirium are age, ASA, physiological state in the emergency room, preoperative diagnosis and prior cognitive impairment.
El delirium es una complicación frecuente en pacientes ancianos intervenidos de cirugía abdominal urgente.
MétodosEstudio prospectivo que incluye pacientes consecutivos ≥ 65 años intervenidos de cirugía abdominal urgente entre 2017 y 2019. Se registró: edad, sexo, ASA, estado fisiológico, deterioro cognitivo, fragilidad (escala de Frail), dependencia funcional (escala de Barthel), calidad de vida (Euroqol-5D-EVA), estado nutricional (MNA-SF), diagnóstico preoperatorio, tipo de cirugía (clasificación BUPA), vía de abordaje y diagnóstico de delirium postoperatorio (Confusion Assessment Method). Se realizó un analysis univariante y multivariante para analizar la relación de estas variables con el delirium.
ResultadosEl estudio incluye 446 pacientes con una median de edad de 78 años; el 63,6% eran ASA ≥ III y el 8% presentaban un deterioro cognitivo previo. El 13,2% eran frágiles y el 5,4% de los pacientes tenían un grado de dependencia grave o total. Un 13,6% desarrollaron delirium en el postoperatorio. En el analysis univariante todas las variables son estadísticamente significativas salvo el sexo, el tipo de cirugía (BUPA) y la duración. En el analysis multivariante los factores asociados fueron: la edad (p < 0,001; OR: 1,08 [IC 95%: 1,038-1,139]), el ASA (p = 0,026; OR: 3,15 [IC 95%: 1,149-8,668]), la alteración fisiológica (p < 0,001; OR: 5,8 [IC 95%: 2,176 15,457]), el diagnóstico (p = 0,006) y el deterioro cognitivo (p < 0,001; OR: 5,8 [IC 95%: 2,391-14,069]).
ConclusiónLos factores asociados al delirium son la edad, el ASA, la alteración fisiológica a su llegada a urgencias, el diagnóstico preoperatorio y el deterioro cognitivo previo.
Acute confusional state or delirium is an acute, fluctuating disorder, characterized by deterioration of cognitive function, decreased level of consciousness, attention disorders and increased or decreased psychomotor activity.1 It is a frequent complication of hospitalized elderly patients, including those who have undergone surgical treatments, and it has been related to increased postoperative stay, morbidity and mortality.2 Today’s longer life expectancy and better quality of life have led to a change in the type of patients undergoing urgent abdominal surgery. Currently, 20%-30% of the population is over the age of 65 (and this percentage is expected to increase in coming decades), and after urgent surgery these patients have a higher risk of presenting postoperative delirium.3–6 Even so, delirium is generally an underdiagnosed complication, especially in surgical patients, which is why it does not always receive adequate treatment.7
The objective of this study is to analyze the incidence and factors associated with postoperative delirium in patients aged 65 or older who underwent urgent abdominal surgery at our hospital. Knowledge of these factors can help identify patients with a higher risk of developing delirium in the postoperative period in order to diagnose and treat it early.
MethodsOur prospective study included elderly patients aged 65 or older who had undergone urgent abdominal surgery at a third-level hospital between January 2017 and January 2019.
Variables AnalyzedA prospective database was designed to collect the demographic variables and different risk factors of the patients during hospitalization. The following were recorded: age, sex, ASA,8 physiological status of the patient upon arrival to the emergency room, previous comorbidity (renal failure, COPD, heart failure, liver failure, acute myocardial infarction), previous cognitive impairment, frailty (using the FRAIL scale),9 functional dependence (Barthel scale10), quality of life (Euroqol-5D-EVA11), nutritional status (MNA-SF12), preoperative diagnosis, type of surgery (BUPA13), surgical approach (open or laparoscopic) and the development of postoperative delirium. For the diagnosis of delirium, the Confusion Assessment Method14 (CAM) was used.
Statistical AnalysisFirst of all, a univariate analysis was performed to analyze the association between postoperative delirium and the different variables evaluated. Subsequently, among the variables that presented a statistically significant association, those with a greater number of events were selected, and a multivariate analysis was performed. For this, the SPSS 22.0 program was used; a P value of <.05 was considered statistically significant.
Ethical AspectsThe study was approved by the Ethics Committee of our hospital. An anonymized database was created to register the variables. All patients agreed to participate in the study and signed a specific informed consent form.
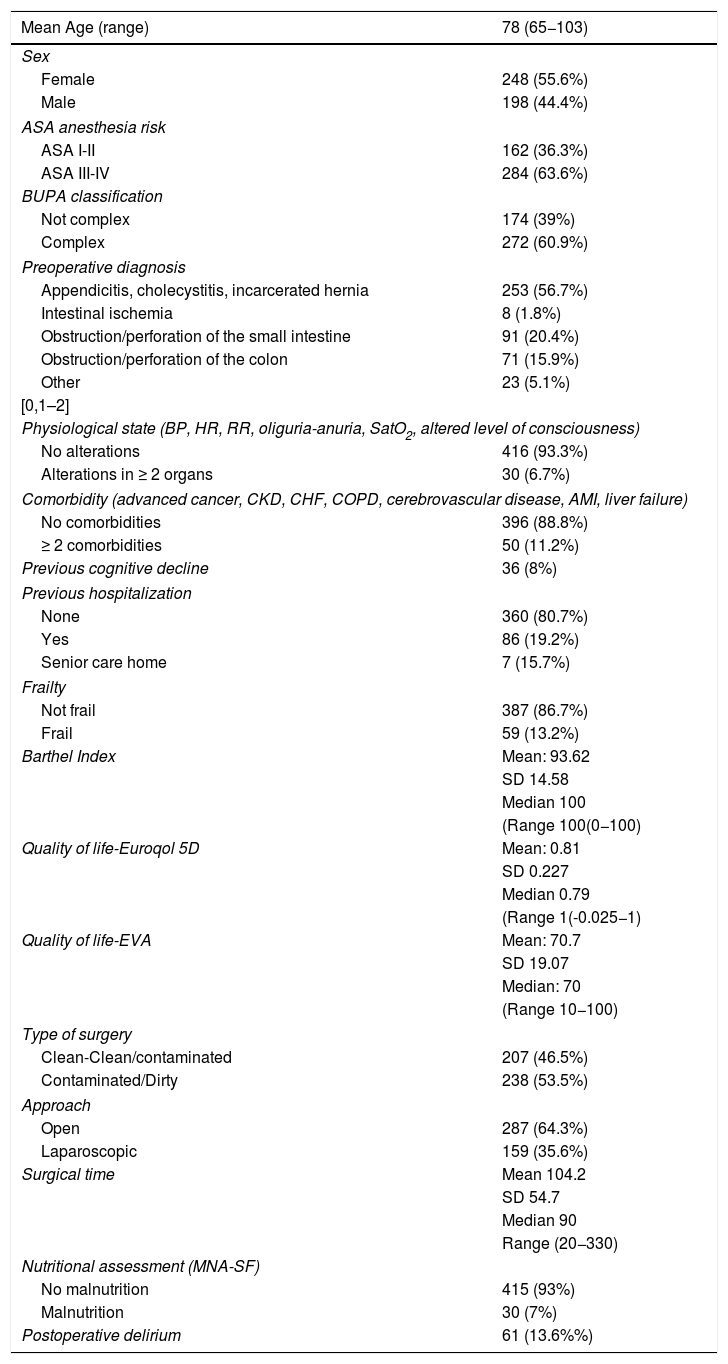
ResultsDemographic VariablesDuring the study period, 446 patients over the age of 65 underwent urgent abdominal surgery. Median age was 78 (Table 1); 63.7% were ASA patients ≥ III; 8% of the patients had cognitive impairment prior to the operation; 13% of the patients were frail; 5.4% were severely or totally dependent, and 94.6% were independent or mildly-moderately dependent. Malnutrition was detected preoperatively in 6.7% of the patients. The incidence of delirium in elderly patients undergoing urgent abdominal surgery was 13.6% (61 patients).
Demographic Data of the Study Patients (n = 446).
| Mean Age (range) | 78 (65−103) |
|---|---|
| Sex | |
| Female | 248 (55.6%) |
| Male | 198 (44.4%) |
| ASA anesthesia risk | |
| ASA I-II | 162 (36.3%) |
| ASA III-IV | 284 (63.6%) |
| BUPA classification | |
| Not complex | 174 (39%) |
| Complex | 272 (60.9%) |
| Preoperative diagnosis | |
| Appendicitis, cholecystitis, incarcerated hernia | 253 (56.7%) |
| Intestinal ischemia | 8 (1.8%) |
| Obstruction/perforation of the small intestine | 91 (20.4%) |
| Obstruction/perforation of the colon | 71 (15.9%) |
| Other | 23 (5.1%) |
| [0,1–2] | |
| Physiological state (BP, HR, RR, oliguria-anuria, SatO2, altered level of consciousness) | |
| No alterations | 416 (93.3%) |
| Alterations in ≥ 2 organs | 30 (6.7%) |
| Comorbidity (advanced cancer, CKD, CHF, COPD, cerebrovascular disease, AMI, liver failure) | |
| No comorbidities | 396 (88.8%) |
| ≥ 2 comorbidities | 50 (11.2%) |
| Previous cognitive decline | 36 (8%) |
| Previous hospitalization | |
| None | 360 (80.7%) |
| Yes | 86 (19.2%) |
| Senior care home | 7 (15.7%) |
| Frailty | |
| Not frail | 387 (86.7%) |
| Frail | 59 (13.2%) |
| Barthel Index | Mean: 93.62 |
| SD 14.58 | |
| Median 100 | |
| (Range 100(0−100) | |
| Quality of life-Euroqol 5D | Mean: 0.81 |
| SD 0.227 | |
| Median 0.79 | |
| (Range 1(-0.025−1) | |
| Quality of life-EVA | Mean: 70.7 |
| SD 19.07 | |
| Median: 70 | |
| (Range 10−100) | |
| Type of surgery | |
| Clean-Clean/contaminated | 207 (46.5%) |
| Contaminated/Dirty | 238 (53.5%) |
| Approach | |
| Open | 287 (64.3%) |
| Laparoscopic | 159 (35.6%) |
| Surgical time | Mean 104.2 |
| SD 54.7 | |
| Median 90 | |
| Range (20−330) | |
| Nutritional assessment (MNA-SF) | |
| No malnutrition | 415 (93%) |
| Malnutrition | 30 (7%) |
| Postoperative delirium | 61 (13.6%%) |
COPD: chronic obstructive pulmonary disease; HR: heart rate; RR: respiratory rate; AMI: acute myocardial infarction; CHF: congestive heart failure; CKD: chronic kidney disease; BP: blood pressure; Sat O2: oxygen saturation.
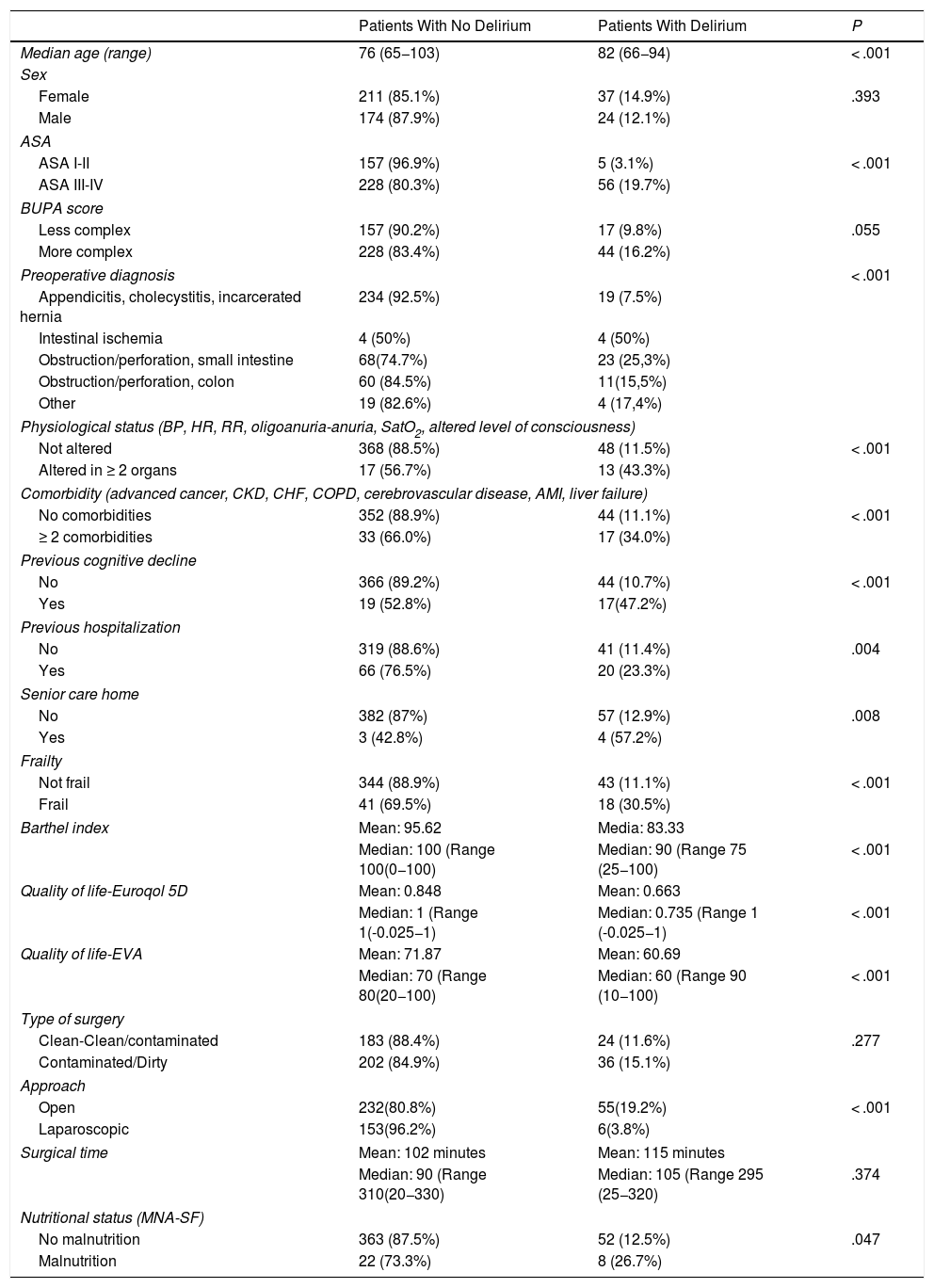
We conducted a univariate analysis of the recorded variables, and their correlation with the appearance of delirium was determined (Table 2). All the variables presented a statistically significant association, except for sex (P = .39), type of surgery (according to the BUPA classification) (P = .055) and the duration of the surgical intervention (P = .37).
Univariate Analysis of Factors Associated With Postoperative Delirium.
| Patients With No Delirium | Patients With Delirium | P | |
|---|---|---|---|
| Median age (range) | 76 (65−103) | 82 (66−94) | < .001 |
| Sex | |||
| Female | 211 (85.1%) | 37 (14.9%) | .393 |
| Male | 174 (87.9%) | 24 (12.1%) | |
| ASA | |||
| ASA I-II | 157 (96.9%) | 5 (3.1%) | < .001 |
| ASA III-IV | 228 (80.3%) | 56 (19.7%) | |
| BUPA score | |||
| Less complex | 157 (90.2%) | 17 (9.8%) | .055 |
| More complex | 228 (83.4%) | 44 (16.2%) | |
| Preoperative diagnosis | < .001 | ||
| Appendicitis, cholecystitis, incarcerated hernia | 234 (92.5%) | 19 (7.5%) | |
| Intestinal ischemia | 4 (50%) | 4 (50%) | |
| Obstruction/perforation, small intestine | 68(74.7%) | 23 (25,3%) | |
| Obstruction/perforation, colon | 60 (84.5%) | 11(15,5%) | |
| Other | 19 (82.6%) | 4 (17,4%) | |
| Physiological status (BP, HR, RR, oligoanuria-anuria, SatO2, altered level of consciousness) | |||
| Not altered | 368 (88.5%) | 48 (11.5%) | < .001 |
| Altered in ≥ 2 organs | 17 (56.7%) | 13 (43.3%) | |
| Comorbidity (advanced cancer, CKD, CHF, COPD, cerebrovascular disease, AMI, liver failure) | |||
| No comorbidities | 352 (88.9%) | 44 (11.1%) | < .001 |
| ≥ 2 comorbidities | 33 (66.0%) | 17 (34.0%) | |
| Previous cognitive decline | |||
| No | 366 (89.2%) | 44 (10.7%) | < .001 |
| Yes | 19 (52.8%) | 17(47.2%) | |
| Previous hospitalization | |||
| No | 319 (88.6%) | 41 (11.4%) | .004 |
| Yes | 66 (76.5%) | 20 (23.3%) | |
| Senior care home | |||
| No | 382 (87%) | 57 (12.9%) | .008 |
| Yes | 3 (42.8%) | 4 (57.2%) | |
| Frailty | |||
| Not frail | 344 (88.9%) | 43 (11.1%) | < .001 |
| Frail | 41 (69.5%) | 18 (30.5%) | |
| Barthel index | Mean: 95.62 | Media: 83.33 | |
| Median: 100 (Range 100(0−100) | Median: 90 (Range 75 (25−100) | < .001 | |
| Quality of life-Euroqol 5D | Mean: 0.848 | Mean: 0.663 | |
| Median: 1 (Range 1(-0.025−1) | Median: 0.735 (Range 1 (-0.025−1) | < .001 | |
| Quality of life-EVA | Mean: 71.87 | Mean: 60.69 | |
| Median: 70 (Range 80(20−100) | Median: 60 (Range 90 (10−100) | < .001 | |
| Type of surgery | |||
| Clean-Clean/contaminated | 183 (88.4%) | 24 (11.6%) | .277 |
| Contaminated/Dirty | 202 (84.9%) | 36 (15.1%) | |
| Approach | |||
| Open | 232(80.8%) | 55(19.2%) | < .001 |
| Laparoscopic | 153(96.2%) | 6(3.8%) | |
| Surgical time | Mean: 102 minutes | Mean: 115 minutes | |
| Median: 90 (Range 310(20−330) | Median: 105 (Range 295 (25−320) | .374 | |
| Nutritional status (MNA-SF) | |||
| No malnutrition | 363 (87.5%) | 52 (12.5%) | .047 |
| Malnutrition | 22 (73.3%) | 8 (26.7%) | |
COPD: chronic obstructive pulmonary disease; HR: heart rate; RR: respiratory rate; AMI: acute myocardial infarction; CHF: congestive heart failure; CKD: chronic kidney disease; BP: blood pressure; Sat O2: oxygen saturation.
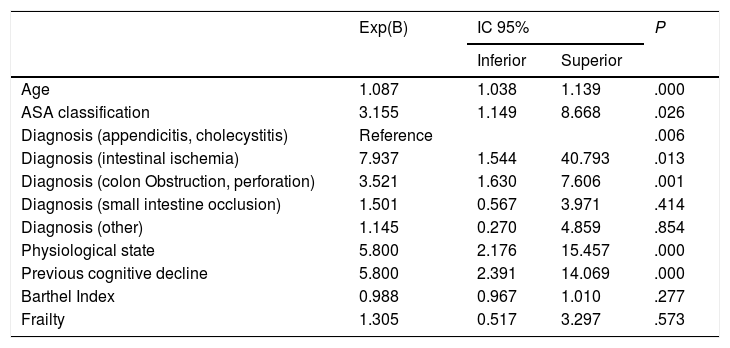
Subsequently, a multivariate analysis was performed (Table 3). The factors associated with delirium were: age (P < .001; OR: 1.08 [95% CI: 1.038–1.139]), ASA ≥III (P = .026; OR: 3.15 [95% CI: 1.149–8.668]), physiological alteration upon arrival at the emergency department (P < .001; OR: 5.8 [95% CI: 2.17–15.45]), preoperative diagnosis (P = .006), and intestinal ischemia, which was the diagnosis more closely associated with delirium (OR 7.9 [95% CI: 1.54–40.79]) and previous cognitive deterioration (P<.001; OR 5.8 [95% CI: 2.39–14]).
Multivariate Analysis of Factors Associated With Postoperative Delirium.
| Exp(B) | IC 95% | P | ||
|---|---|---|---|---|
| Inferior | Superior | |||
| Age | 1.087 | 1.038 | 1.139 | .000 |
| ASA classification | 3.155 | 1.149 | 8.668 | .026 |
| Diagnosis (appendicitis, cholecystitis) | Reference | .006 | ||
| Diagnosis (intestinal ischemia) | 7.937 | 1.544 | 40.793 | .013 |
| Diagnosis (colon Obstruction, perforation) | 3.521 | 1.630 | 7.606 | .001 |
| Diagnosis (small intestine occlusion) | 1.501 | 0.567 | 3.971 | .414 |
| Diagnosis (other) | 1.145 | 0.270 | 4.859 | .854 |
| Physiological state | 5.800 | 2.176 | 15.457 | .000 |
| Previous cognitive decline | 5.800 | 2.391 | 14.069 | .000 |
| Barthel Index | 0.988 | 0.967 | 1.010 | .277 |
| Frailty | 1.305 | 0.517 | 3.297 | .573 |
In contrast, comorbidity, frailty, nutritional status, and functional dependence were not statistically associated with delirium in the multivariate analysis.
DiscussionThe appearance of postoperative delirium is an increasingly frequent and more commonly studied complication because, due to increased life expectancy and less invasive procedures, a growing percentage of elderly patients are undergoing urgent surgery.5 The incidence of delirium in patients over the age of 65 treated with urgent abdominal surgery at our hospital was 13.6%. This percentage falls within the range published by several studies of elderly patients after both scheduled and urgent surgery, which is around 15%;2 however, percentages can vary between 3% and 27%, and even up to 50% in patients over 80.15
Delirium is a multifactorial pathology, in which patient-specific and intercurrent factors can be identified.16 Our study has identified patient age, ASA classification ≥ III and previous cognitive impairment as patient-related factors.
Age is a known risk factor. There are multiple studies that support the relationship between a higher percentage of delirium at an older age or after the age of 70. One of the most complete publications is a retrospective study from 201817 from Annals of Surgery, with 2168 patients admitted by the surgery service. This study concluded that age is the main associated factor, more so than previous functional status or history of cerebrovascular disease.
Another associated patient-specific factor is the ASA physical status classification system. In our study, patients with an ASA ≥ III18 had a higher risk of developing postoperative delirium. This concurs with other studies, such the Raats group study from 2015,19 which concluded that, in addition to patient age and previous decline, patients with higher ASA have a higher risk of postoperative delirium. Similarly, the patient’s previous cognitive impairment or dementia is another known factor that predisposes them to developing delirium; in our study, 47.2% of patients with previous deterioration developed delirium, compared to 10.7% of those without. Although dementia and delirium can present similar symptoms16 and are sometimes difficult to differentiate postoperatively, the causes are different: delirium is an acute and potentially reversible state, while the origin of dementia is generally organic and irreversible.
In a second group, we have found factors that precipitate or favor the appearance of delirium. All the patients in our study underwent urgent surgery and required postoperative hospitalization, so this cannot be considered a factor, but the physiological alteration that patients presented upon arrival to the emergency room and the preoperative diagnosis were found to be related factors in the multivariate analysis.
The physiological alteration upon arrival to the emergency department reflects the hemodynamic impact of the process on the patient, and the greater the alteration, the greater the risk of developing delirium later. A similar situation occurs with preoperative diagnosis, where pathologies that require more aggressive surgeries (intestinal ischemia or colon occlusion) pose a greater risk compared to less aggressive surgeries (acute appendicitis or small intestine occlusion). Both factors refer to the severity of the intercurrent process for which patients are being treated and how this poses a greater risk for patients.
Other studies also refer to the physiological alteration15 of patients or to the severity of the diagnosis and the surgery required (major surgery versus minor surgery) and the development of delirium. Following this result, it could be argued that less invasive surgeries or treatments (laparoscopy, endoscopy, etc) could reduce surgical aggression and, consequently, the development of delirium. In our study, patients who underwent laparoscopy had an incidence of 3.8% versus 19.2% in open surgery. However, this data is biased because the diagnoses were not the same and, therefore, these two groups are not comparable. It would be interesting to conduct a prospective study, selecting a single indication in order to compare patients with urgent laparoscopic procedures versus open surgery in order to assess the effect on delirium.
There are a number of limitations to consider when analyzing our study. Mainly, certain variables were not included, such as postoperative complications or the medication administered during the postoperative period, which in other studies have been associated with the development of delirium. Another possible limitation is that the days of hospital stay until the onset of delirium were not taken into account. Some publications17 refer an average of 4–5 days of hospitalization; this is an interesting fact, but it can also be biased, since it excludes patients undergoing less aggressive surgeries who may be discharged before developing delirium, and it also excludes patients who die in the immediate postoperative period, generally after being treated for a serious pathology. We also did not register other variables that were associated in other studies, such as prior alcoholism20 (abstinence during admission increases risk of delirium) or factors that cause patients to become more disoriented, such as prolonged ICU care or visual/hearing deficiencies. We believe it would be appropriate to include these variables in future studies on this matter.
Lastly, there is no consensus among the various studies when it comes to specifying the age of the patients included. In our study, we selected patients over the age of 65,21,22 since this age is currently used in epidemiological records as the beginning of old age when considering the legal retirement age. On the contrary, other studies include all surgically treated patients or select those older than 70 or 80, which may limit the ability to make comparisons.18,23
However, this study presents a large, homogeneous series of patients who had all been treated surgically at the same hospital, with objective diagnostic criteria based on international classifications and registered prospectively. Most studies on delirium in surgical patients are based on retrospective analyses, generally elective surgery, mainly colorectal, or mix urgent and elective patients. For this reason, this study provides a more objective view of the development of delirium in patients undergoing urgent general surgery. Although the main risk factors cannot be modified (age, ASA, diagnosis, etc) and therefore cannot be altered to reduce the incidence, knowledge of these factors does allow us to identify patients at higher risk, thereby facilitating early diagnosis and treatment while avoiding other associated complications.
FundingThe authors have received no specific funding for this study from public, commercial or non-profit sectors.
Conflict of InterestsAll the authors meet the criteria of the International Committee of Medical Journal Editors (ICMJE) and have no conflicts of interests.
Please cite this article as: Sánchez Acedo P, Eguaras Córdoba I, Zazpe Ripa C, Herrera Cabezón J, Tarifa Castilla A. Estudio prospectivo de los factores asociados al delirium en el postoperatorio de la cirugía abdominal urgente. Cir Esp. 2020;98:450–455.