An occult pneumothorax is found in 2%–15% trauma patients. Observation (without tube thoracostomy) in these patients presents still some controversies in the clinical practice. The objective of the study is to evaluate the efficacy and the adverse effects when observation is performed.
MethodsA retrospective observational study was undertaken in our centre (university hospital level II). Data were obtained from a database with prospective registration. A total of 1087 trauma patients admitted in the Intensive Care Unit from 2006 to 2013 were included.
ResultsIn this period, 126 patients with occult pneumothorax were identified, 73 patients (58%) underwent immediate tube thoracostomy and 53 patients (42%) were observed. Nine patients (12%) failed observation and required tube thoracostomy for pneumothorax progression or haemothorax. No patient developed a tension pneumothorax or experienced another adverse event related to the absence of tube thoracostomy. Of the observed patients 16 were under positive pressure ventilation, in this group 3 patients (19%) failed observation. There were no differences in mortality, hospital length of stay or intensive care length of stay between the observed and non-observed group.
ConclusionObservation is a safe treatment in occult pneumothorax, even in pressure positive ventilated patients.
Alrededor del 2–15% de los pacientes politraumatizados presentan un neumotórax oculto. La aplicación del tratamiento conservador (observación) en la práctica clínica diaria aún sigue siendo controvertido. Nuestra hipótesis es que es factible realizar un tratamiento conservador. El objetivo de este estudio es evaluar la eficacia y los efectos adversos del tratamiento conservador del neumotórax oculto en nuestro medio.
MétodosEstudio observacional retrospectivo (análisis de base de datos con registro prospectivo) realizado en un hospital universitario de nivel II. Inclusión de 1.087 pacientes politraumatizados mayores de 16 años ingresados en el área de críticos desde 2006 hasta 2013.
ResultadosEn este periodo, 126 pacientes presentaron neumotórax oculto, en 73 (58%) se decidió observación. En 9 pacientes (12%) fracasó la observación (precisaron colocación de drenaje pleural) por aumento del neumotórax o aparición de hemotórax. De los pacientes observados, 16 fueron ventilados bajo presión positiva. En este grupo fracasó la observación en 3 pacientes (19%). Ningún paciente presentó neumotórax a tensión u otro problema relacionado con la ausencia de drenaje. No hubo diferencias entre grupos (observación vs drenaje) respecto a mortalidad, estancia hospitalaria ni estancia en la unidad de críticos.
ConclusiónEl tratamiento de elección de los pacientes con neumotórax oculto es la observación clínica. Este tratamiento también es factible en los pacientes ventilados bajo presión positiva.
Occult pneumothorax (OCPT) is a pneumothorax that is diagnosed by computerised tomography (CT), without previous clinical suspicion or identification by thoracic X-ray. In polytrauma patients the use of thoracic CT is becoming increasingly frequent, so that more cases of OCPT are being diagnosed. Its current prevalence stands at 2%–15% of cases.1
Considering that pleural drainage is associated with up to 22%–30% of complications,2,3 conservative treatment is becoming more widespread. It is important to know the degree to which conservative treatment is safe and effective, especially in patients treated using positive pressure ventilation (PPV). In Spain no prospective studies have evaluated the safety and efficacy of conservative treatment in our area.
The main aim of our study is to evaluate the efficacy and adverse effects of conservative treatment of OCPT in our area. Secondarily it aims to discover the prevalence of OCPT and to identify the incidence and indications for thoracic drainage in these patients.
MethodsA retrospective revision (data recorded prospectively) of polytrauma patients over the age of 16 years old diagnosed with OCPT and admitted to the critical care section of our hospital (a level II teaching hospital) from March 2006 to December 2013.
The Treatment of Patients With Occult PneumothoraxAll polytrauma patients who are admitted to our hospital are subjected to a thoracic X-ray (as part of their primary examination) which is analysed by the on-duty team. If pneumothorax or haemothorax is found a pleural drain is put into place. Thoracic CT is used if a thoracic injury is found or suspected. Abdominal CT is used when there is a clinical suspicion that haemodynamically stable patients have an abdominal injury. OCPT is diagnosed if thoracic or abdominal CT shows a pneumothorax that was not detected in the initial thoracic X-ray. The decision to drain OCPT is taken by the on-duty team, which is composed of professionals in General Surgery, Anaesthesiology or Intensive Care and Orthopaedics. The following factors were considered criteria for drainage: the concomitant presence of haemothorax, large pneumothorax, haemodynamic instability or if the patient required emergency surgery for another reason. We considered that the other patients could be treated conservatively, regardless of whether they are under ventilator support.
Definition of VariablesThe following variables were recorded: age, sex, trauma mechanism, severity of trauma according to the Injury Severity Score (ISS), hospital stay, stay in the Intensive Care Unit (ICU), mortality rate during admission, type of OCPT treatment (drainage or conservative), drainage complications (poor positioning, loss, infection of the insertion point or bleeding secondary to insertion), complications with the conservative treatment (the appearance of tension pneumothorax) and the success rate of conservative treatment. Conservative treatment was considered to have failed if pleural drainage had to be put into place during the hospital admission.
Statistical AnalysisDescriptive analysis of quantitative data was performed using central and dispersion tendency measurements according to normality criteria. The comparative study between qualitative variables was performed according to the chi2 or Fisher's test and quantitative variables according to Student's t-test or the Kolmogorov–Smirnov test. P<.05 was considered to be the statistically significant value. The Stata® 12.1 program was used to analyse data.
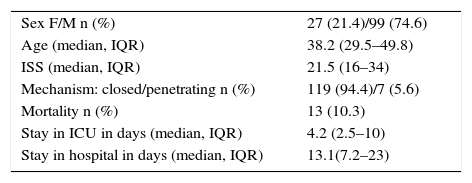
ResultsDuring the years 2006–2013 1087 polytrauma patients were recorded as admitted to the critical or semi-critical care sections of our hospital. 126 (11.6%) of these presented OCPT. The demographic characteristics of the cohort are shown in Table 1. The majority presented closed trauma (94%). They were patients with severe multiple trauma with a median ISS of 22.
Characteristics of the Cohort of Polytrauma Patients.
| Sex F/M n (%) | 27 (21.4)/99 (74.6) |
| Age (median, IQR) | 38.2 (29.5–49.8) |
| ISS (median, IQR) | 21.5 (16–34) |
| Mechanism: closed/penetrating n (%) | 119 (94.4)/7 (5.6) |
| Mortality n (%) | 13 (10.3) |
| Stay in ICU in days (median, IQR) | 4.2 (2.5–10) |
| Stay in hospital in days (median, IQR) | 13.1(7.2–23) |
M: men; ISS: Injury Severity Score; W: women; IQR: interquartile range.
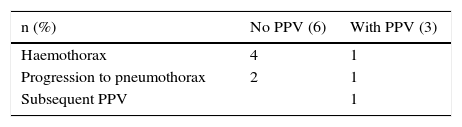
It was decided to observe 73 (58%) of the 126 patients with OCPT; 16 of these patients were under PPV. None presented tension pneumothorax or any other problems associated with the absence of drainage. In the group under observation, 9 patients required pleural drainage (failure of observation in 12%). Eight cases required the insertion of pleural drainage due to the appearance of haemothorax (5 patients, 55%) or because a check-up X-ray showed pneumothorax (3 patients, 34%). One patient was fitted with a prophylactic pleural drainage prior to surgery for a lower limb fracture. In the subgroup of ventilated patients, the failure rate of conservative treatment was 19% (3 patients) compared to the 11% in the non-ventilated group. (This difference between groups is not statistically significant [P=.401].) Table 2 shows that the indications for subsequent drainage were the same in the groups of ventilated and unventilated patients.
It was decided to insert pleural drainage as an initial treatment in 53 patients (42%). The indications for drainage were: haemothorax (22 patients, 42%), prior to emergency surgery (7 patients, 13%), large size shown by thoracic CT (3 patients, 6%) or haemodynamic instability (2 patients, 4%). In 9 patients (17%) the indication was because they were under PPV. The other 10 cases (19%) were unventilated patients who did not require drainage.
Three patients presented complications associated with the drainage (6%), 2 due to insertion of the drain into the subcutaneous tissue and one case of loss of the drainage after a few hours. The 3 cases required repositioning of the drainage.
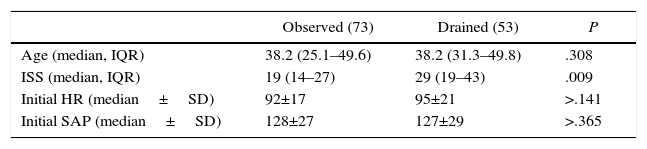
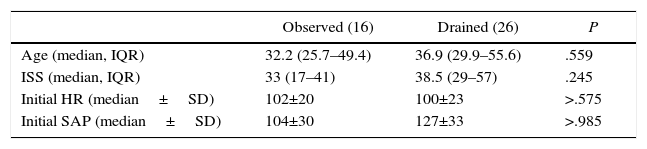
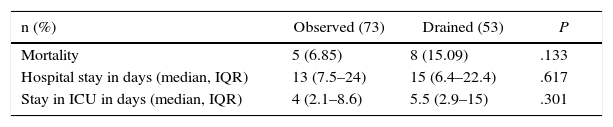
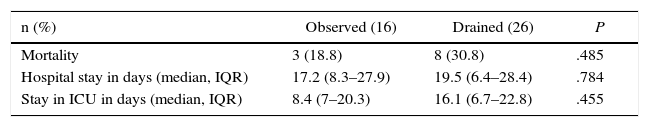
There were no differences between the groups of drained vs observed patients in terms of their age or initial haemodynamic stability. Nevertheless, the group of drained patients had a higher ISS (P=.009) (see Table 3). Table 4 shows that in the subgroup of ventilated patients there was also no differences between those observed or drained. No statistically significant differences were found regarding mortality, hospital stay or stay in the ICU between the patients initially observed or drained (see Table 5), although the group of drained patients did present higher mortality (15% vs 6.8%), although we attribute this to their higher initial ISS. Nor were there any statistically significant differences between these parameters in the subgroup of ventilated patients (see Table 6).
Comparison Between Groups.
| Observed (73) | Drained (53) | P | |
|---|---|---|---|
| Age (median, IQR) | 38.2 (25.1–49.6) | 38.2 (31.3–49.8) | .308 |
| ISS (median, IQR) | 19 (14–27) | 29 (19–43) | .009 |
| Initial HR (median±SD) | 92±17 | 95±21 | >.141 |
| Initial SAP (median±SD) | 128±27 | 127±29 | >.365 |
SD: standard deviation; HR: heart rate; ISS: Injury Severity Score; SAP: systolic arterial pressure; IQR: interquartile range.
Comparison of Groups Within the Subgroup of Ventilated Patients.
| Observed (16) | Drained (26) | P | |
|---|---|---|---|
| Age (median, IQR) | 32.2 (25.7–49.4) | 36.9 (29.9–55.6) | .559 |
| ISS (median, IQR) | 33 (17–41) | 38.5 (29–57) | .245 |
| Initial HR (median±SD) | 102±20 | 100±23 | >.575 |
| Initial SAP (median±SD) | 104±30 | 127±33 | >.985 |
SD: standard deviation; HR: heart rate; ISS: Injury Severity Score; SAP: systolic arterial pressure; IQR: interquartile range.
Results per Group Within the Subgroup of Ventilated Patients.
| n (%) | Observed (16) | Drained (26) | P |
|---|---|---|---|
| Mortality | 3 (18.8) | 8 (30.8) | .485 |
| Hospital stay in days (median, IQR) | 17.2 (8.3–27.9) | 19.5 (6.4–28.4) | .784 |
| Stay in ICU in days (median, IQR) | 8.4 (7–20.3) | 16.1 (6.7–22.8) | .455 |
IQR: interquartile range; ICU: Intensive Care Unit.
The prevalence of OCPT in polytraumata patients in our series is 11.6%, which agrees with other publications (2%–15%).1 There has been widespread discussion as to whether OCPT really are occult or if they were not correctly evaluated by the on-duty team that treated the polytrauma patient. However, there are a series of cases in which expert radiologists examined the X-rays in question retrospectively and only identified about 10% of the OCPT.4,5 It is hard to identify pneumothorax in polytrauma patients as the initial X-ray has to be taken with the patient lying down. Radiography in this position is less sensitive in detecting a pneumothorax than when the patient is standing, although there are some signs which help to identify it.6 The concomitant presence of subcutaneous emphysema is associated with the presence of pneumothorax, although the majority of patients with OCPT do not show subcutaneous emphysema in the X-ray.7 In our series only 22 patients (17%) presented associated subcutaneous emphysema.
Thoracic CT is the imaging test of choice for the identification of OCPT, although thoracic ultrasound examination may also be useful. However, it is currently unclear whether the definition of OCPT also covers cases of pneumothorax diagnosed using thoracic ultrasound.8,9 In our series the majority of the OCPT were identified by thoracic CT, although 22 cases (17%) were identified by abdominal CT. Abdominal CT has an OCPT identification rate higher than 90%.10–12
The current published rates of drainage in cases of OCPT run from 12%–59%,1 and they are somewhat higher in cases of penetrating trauma.13 Our overall rate stands at 42%, although it is 86% in patients with penetrating trauma (6 of 7 patients). This is probably due to the high rate of associated haemothorax (76%) in penetrating trauma. The current overall failure rates of conservative treatment (observation) run from 6% to 11%.1 The most frequent causes of failure are the progression of the pneumothorax and the appearance of haemothorax. Given that OCPT rarely progress unless the patient is treated using PPV, the majority of studies centre on this group. In our study we present an overall conservative treatment failure rate of 12%, and a rate of 19% in patients under PPV. This agrees with other publications (14%–31% in patients under PPV).1,14
In a prospective randomised study of patients under PPV in 1993 Enderson et al.15 found a conservative treatment failure rate of 53% (8 of 15 patients) while 20% (3 of 15 patients) had tension pneumothorax in the observation group. Nevertheless, in subsequent prospective randomised studies in patients under PPV the rate of tension pneumothorax is far lower (<2%).14,16 We had no case of tension pneumothorax, although in our hospital there is still a strong tendency to drain OCPT in patients under PPV (20%). In the latest randomised studies undertaken with patients under PPV the respiratory distress rates, hospital stay, stay in the ICU and mortality are similar in both groups (observation vs drainage), so that management using observation is considered to be safe.14 In our series, in the ventilated patients subgroup no significant differences were found respecting hospital stay, stay in the ICU or mortality. The latest Eastern Association for the Surgery of Trauma guide (EAST 2011) recommends that OCPT cases be placed under observation if the patients are stable, regardless of whether or not they are ventilated.17
The following factors were identified as predictive of the failure of conservative treatment: pneumothorax progression, the appearance of respiratory distress,1 a higher “revised trauma score”, multisystemic trauma14 and sustained ventilation. Kirpatrick et al.3 concluded that observation is safe in patients intubated for an operation, but that up to one third of patients who are intubated for more than one week eventually require drainage. In our case conservative treatment failed in only 3 ventilated patients, and in all 3 cases drainage commenced a few hours after intubation.
Neither the size nor the location of the pneumothorax has been associated with the failure of conservative treatment. In 1998 Wolfman et al.18 published the finding that small anterior OCPT could be successfully observed (81%). A revision in 2006 concluded that although small pneumothorax could be observed, there was no evidence showing what had to be done with larger OCPT.19 However, it is hard to define what constitutes a small pneumothorax because the volume of the pneumothorax is not routinely quantified in clinical practice. De Moya's group tried to create volumetric methods using multidetector CT20 as well as a predictive score for failure21 according to the size and position of the pneumothorax.
In our centre we do not measure the size of OCPT or assess the location, so that we do not take these variables into account for treatment. Our study is limited by the fact that we only included patients with severe multiple trauma who were closely monitored during their hospitalisation. All of them are monitored continuously and a thoracic X-ray is taken every day. The less severe patients admitted to a normal ward are not treated by PPV, so that it is considered to be safe to manage them conservatively with radiological checks. We believe it to be advisable to keep these patients in observation for at least 24h after admission and to check them by X-ray before deciding to discharge them.
We conclude that the treatment of choice for OCPT is clinical observation, and that this is also feasible in patients ventilated under positive pressure.
Conflict of InterestThe authors have no conflict of interest to declare.
The authors would like to thank Andrea Campos, Mireia Figueroa and Marta Alberich for their help in data gathering, without which this work would not have been possible.
Please cite this article as: Llaquet Bayo H, Montmany Vioque S, Rebasa P, Navarro Soto S. Resultados del tratamiento conservador en pacientes con neumotórax oculto. Cir Esp. 2016;94:232–236.
Some of the data in this study were presented as an oral communication in the 29th National Surgery Congress held in Madrid in November 2012 under the title “Results of conservative treatment in polytraumatised patients with occult pneumothorax”.