To analyse the indications, actions and results of the operations performed in the Cardiovascular Surgery Intensive Care Unit.
MethodsRetrospective analysis of consecutive non-selected adult patients operated in the ICU, with descriptive statistics. All operations performed were included.
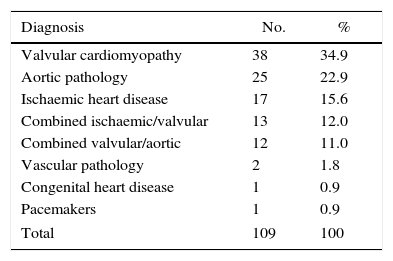
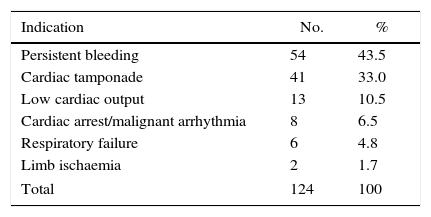
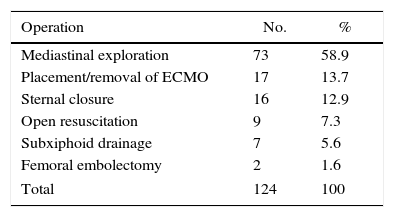
ResultsBetween 2008 and 2013, 3379 consecutive adult patients were operated upon. A total of 124 operations were performed in the ICU in 109 patients 70 male (64.2%) and 39 female (35.8%), with a mean age of 61.6 years (12–80). This represented 3.2% of all operations. During the study period, 185 patients (5.5%) were reoperated for postoperative bleeding/cardiac tamponade in the operating room. Previous interventions were for valvular heart disease (34.9%), aortic disease (22.9%), ischaemic heart disease (15.6%), combined valvular/ischaemic (12%), valvular/aorta (11%) and miscellaneous (3.6%). The indications for reoperation were: persistent bleeding 54 (43.5%), pericardial tamponade 41 (33%), low cardiac output 13 (10.5%), cardiac arrest/arrhythmia 8 (6.5%), respiratory insufficiency 6 (4.8%) and acute ischaemic limb 2 (1.7%). Operations performed were: mediastinal exploration 73 (58.9%), implant/removal of ECMO 17 (13.7%), sternal closure 16 (12.9%), open resuscitation 9 (7.3%), subxiphoid drainage 7 (5.6%) and femoral embolectomy 2 (1.6%). Overall mortality was 33%. There was one case of mediastinitis 0.9%, with no difference from patients operated in the regular operating room.
ConclusionsOperations in the ICU represent a safe, life-saving alternative in specific subgroups of patients. The risk of wound infection is not increased, unstable patients are not transferred and there is time savings.
Analizar las indicaciones, acciones y resultados de las operaciones realizadas en la Unidad de Cuidados Intensivos (UCI) de Cirugía Cardiovascular.
MétodosAnálisis retrospectivo de pacientes adultos consecutivos intervenidos en la Unidad de Cuidados Intensivos (UCI). Se incluyeron todas las intervenciones practicadas. Se realizó estadística descriptiva.
ResultadosEntre 2008 y 2013 se intervinieron 3379 pacientes adultos consecutivos. Se practicaron en la UCI 124 intervenciones en 109 pacientes, 70 hombres (64,2%) y 39 mujeres (35,8%) con un promedio de edad de 61,6 años (12-80). Ello ha representado un 3,2%. Durante el mismo periodo de tiempo, se intervinieron en quirófano 185 pacientes por taponamiento cardiaco/hemorragia postoperatoria (5,5%). Las intervenciones previas fueron por cardiopatía valvular (34,9%), patología aórtica (22,9%), cardiopatía isquémica (15,6%), valvular/isquémica (12%), valvular/de la aorta (11%) y miscelánea (3,6%). Las indicaciones de intervención fueron hemorragia persistente 54 (43,5%), taponamiento cardiaco 41 (33%), bajo gasto cardiaco 13 (10,5%), parada cardíaca/arritmias 8 (6,5%), insuficiencia respiratoria 6 (4,8%) e isquemia de extremidades 2 (1,7%). Las intervenciones fueron: exploración mediastínica 73 (58,9%), colocación/retirada de ECMO 17 (13,7%), cierre esternal 16 (12,9%), resucitación abierta 9 (7,3%), drenaje subxifoideo 7 (5,6%) y embolectomía femoral 2 (1,6%). La mortalidad fue 33%. Hubo un caso de mediastinitis (0,9%), sin diferencias con la tasa de infecciones profundas en pacientes no intervenidos en UCI.
ConclusionesLa intervención en UCI es una alternativa segura y de rescate en subgrupos específicos de pacientes. no incrementa el riesgo de infección, evita el transporte de pacientes inestables y permite ahorrar tiempo en la decisión quirúrgica postoperatoria.
Approximately 5%–8% of patients who undergo cardiac surgery require reoperation in the immediate postoperative period. The most frequent complications requiring intervention are: postoperative bleeding, cardiac tamponade, haemodynamic instability (cardiac arrest or arrhythmia), prolonged mechanical ventilation with tracheotomy, deferred sternal closure, and placement or removal of circulatory assist devices.1
In general, patients who require postoperative surgical techniques after cardiac surgery are transferred to the operating room in conditions of haemodynamic instability (hypotension, low cardiac output, persistent haemorrhage), which can aggravate the situation by increasing the risks inherent of reoperation. Furthermore, the disadvantage of the distance between the intensive care unit (ICU) and the cardiac surgery operating theatre must also be taken into account, as well as the time necessary to organise the surgical team outside the regular work schedule or on holidays. The minimum time for organising the operating room can oscillate between 1 or 2h in most hospitals, which can influence the final result. Only a limited number of hospitals have an appropriate design in which the ICU and the operating room are integrated into one unit.2
An alternative option to surgical exploration in the operating room is to operate in the ICU. This alternative is accepted in practice, although there are few data available about its use in our setting. The accumulated experience of surgical interventions in the ICU and the positive results have gradually increased its indication and encouraged its use instead of transferring patients with haemodynamic instability to the operating room.3
The objective of the present article is to present our department's experience with operations conducted in the ICU in patients with previous major cardiac surgery. We also present the results derived from this alternative versus conventional surgical exploration.
MethodsThis study is a retrospective analysis of consecutive adult patients who had undergone major surgery (sternotomy and thoracotomy with/without extracorporeal circulation) who required reoperation in the ICU. Data from the department's database were analysed with descriptive statistics.
The patients were operated on in accordance with operating room surgical protocol and the Resuscitation Guidelines by the European Association for Cardio-thoracic Surgery.4
DecisionThe decision to operate on a patient in the ICU should be made by the head surgeon or the surgeon with the most experience and responsibility.
DefinitionsMajor Cardiac SurgeryMajor cardiac surgery was defined as any intrathoracic or thoracoabdominal operation on the heart and large intrathoracic vessels, with or without extracorporeal circulation (e.g. myocardial revascularisation, pericardiectomy, correction of thoracic aneurysm).
Indications for ReoperationThe following conditions were considered indications for reoperation: persistent postoperative haemorrhage, cardiac tamponade, cardiac arrest or malignant arrhythmias, heart or respiratory failure that were refractory to medical treatment, retrosternal collections and cardiac oedema.
Postoperative HaemorrhageA haemorrhage required revision surgery when: postoperative discharge was 400mL/h in the first hour (200mL/m2), more than 300mL/h for 2h (150mL/m2/h×2–3h) or more than 200mL/h for 4h (100mL/m2/h×4h).5
Cardiac TamponadeCardiac tamponade was defined as the clinical situation that results from cardiac compression caused by effusion of fluid or accumulation of blood or clots in the pericardium, resulting in increased intrapericardial pressure, increased venous pressure and circulatory collapse, with a drop in systolic arterial pressure during inspiration.6
Open SternotomyOpen sternotomy was used for mediastinal packing with compresses if intrathoracic haemostasis was impossible to control. We also opted for deferred closure if it was impossible to perform thoracic closure due to dilatation of the cardiac cavities, and open sternum management was therefore necessary.7,8
Refractory Heart FailureThis refers to stage D heart failure, according to the classification proposed by the American College of Cardiology/American Heart Association. This includes patients with advanced structural heart disease and acute signs of heart failure at rest in spite of optimal medical treatment with intravenous inotropic drugs who would be candidates (given no contraindications) for other specialised therapeutic alternatives, such as heart transplantation, surgical ventricular restoration or mechanical circulatory support.9
Refractory Respiratory FailureRefers to situations in which hypoxaemia or hypercarbia cannot be corrected despite maximum invasive mechanical ventilation.
Hospital MortalityHospital mortality was defined as deaths in the operating room, within the first 30 days after the surgical procedure, or after the first 30 days if the patient remained hospitalised. Complications and mortality were reported in accordance with the guidelines by Akins et al.10
Equipment, Procedure and TechniqueWe followed the recommendations for the exploration of patients in cardiac arrest after cardiac surgery published by the European Association for Cardio-thoracic Surgery, which are applied to all types of ICU interventions.4
The procedure for ICU interventions was the same that is followed in the operating theatre, except that the patient remained in their hospital bed with ICU monitoring (ECG, BP, pulmonary arterial pressure, oxygen saturation). The surgical team included the surgeon and assisting surgeon and, when possible, surgical staff. Preparation included washing and dressing as in the operating room. An additional dose of antibiotic prophylaxis was administered. The operative site was prepared with iodine solution. Plastic surgical drapes covered selected skin areas in order to minimise skin exposure.
The procedures were done under general anaesthesia. A member of the ICU team stood at the head of the bed to administer medication and monitor the patient. The soft tissue and sternal edges were inspected, any clots present in the cavity were suctioned and the surgical sutures were inspected systematically. Any bleeding points were immediately controlled with sutures, metallic staples, electrocoagulation or haemostatic material, and chest drain tubes were reused. Once haemostasis was reached, the chest was closed normally with stainless steel wire for the sternum and closure by planes. Local instillation of antibiotic solution was not used to treat the surgical wound.
ResultsBetween 2008 and 2013, 3379 consecutive adult patients underwent major cardiac surgery. There were 124 reoperations done in 109 patients: 70 men (64.2%) and 39 women (35.8%). Mean age was 61.6 (12–80). In our setting, this represented 3.2%. During the same time period, 185 patients were treated in the OR for cardiac tamponade/postoperative bleeding, which was 5.5%.
The original interventions in this group that required reoperation in the ICU are shown in Table 1. The two patients with vascular pathology included in this table were treated for abdominal aortic aneurysm and haemorrhage of the supra-aortic trunks prior to stent placement. The indication for intervention in the ICU is described in Table 2. The most frequent causes for surgery in the ICU were persistent postoperative bleeding in 54 cases (43.5%) and cardiac tamponade in 41 (33%).
The surgical procedures conducted in the ICU are shown in Table 3. Since the most frequent indications were postoperative bleeding and cardiac tamponade, mediastinal exploration was done in 60.5% of cases. In 13.7% of patients, we proceeded with the placement or removal of circulatory support devices. All the procedures were completed in accordance with the standard surgical protocol of the Cardiovascular Surgery Department.
MortalityThe mortality rate of the series was 33% (36 cases). The causes of death of the patients in our series were: multiple organ failure, 27; malignant ventricular arrhythmia, 1; exsanguination, 2; massive haemoptysis, 1; cardiogenic shock, 2; and cerebrovascular accident, 2. None of the deaths were related with the surgical approach or having performed the operation in the ICU.
Infection of the Surgical WoundOne case of mediastinitis was detected, which represented 0.9% of the patients and 0.8% of the surgeries performed, which did not differ from the rate of deep infection among non-reoperated patients (0.7%). This rate is also equivalent to reports in the literature (1%–2%).11
DiscussionOperations after cardiac surgery have traditionally been done in the operating room, unless the situation was an extreme emergency, such as cardiac arrest. However, the transfer of patients to the operating theatre delays surgery, increases costs and involves mobilising patients in situations of haemodynamic instability.12
Life-saving emergency open chest resuscitation, as well as several other operations, can be done quickly in a well-equipped ICU with minimal morbidity and no mortality related with the procedure itself. Mortality is related with the pathology and underlying condition, although it can be argued that an emergency procedure can contribute to increased risk.
Essential prerequisites include a properly equipped ICU and staff that are capacitated to obtain adequate results when this aggressive procedure is used in patients who are in deteriorated conditions after the initial operation.13 Currently, it is fundamental to consider the recommendations of the European Association for Cardio-thoracic Surgery as part of the protocol in the intensive care setting in the postoperative period after cardiac surgery. The publication of these recommendations has confirmed the importance of an aggressive, structured approach in patients in unstable situations.4
One complication that is associated with increased morbidity and mortality is infection of the surgical wound. If the operation is done outside the standard operating room setting, increased incidence could be expected. The fear of an appreciable increase in the incidence of surgical wound infection could be considered a limiting factor in the decision-making process for reoperation in the ICU. Nevertheless, the rate of infection among patients reoperated in the ICU of this study was 0.9%, which is comparable to the rates observed among patients who were not operated on in the ICU (between 1% and 5%14,15). Moreover, these levels have not changed substantially in the last three decades.15 In our recent experience, the rate of deep infection of the surgical wound has been 0.7%. In addition, the mortality and postoperative complication rates are comparable to those reported in the literature.
The profile of the surgical interventions is very varied depending on the indication for the operation. For this reason, not all surgeries are comparable in terms of aggressiveness or impact. This series did not include 23 cases of surgical tracheotomy. Nonetheless, it is a surgical intervention that is perfectly defined and should not be underrated.
It is difficult to quantify an eventual benefit of ICU surgery due to the difficulties in the design of a controlled study with randomised assignation to treatment groups. However, while accepting limitations, the organisation of the operative field is immediate once the decision to operate has been made, without the need to wait for an available operating room, especially outside of scheduled work hours, as mentioned previously. Based on the retrospective experience presented here, surgical interventions done in the ICU can be considered a recommendable approach in critical patients after cardiac surgery, guided by common sense, reports in the literature, current recommendations and eventual economic benefits (although these were not analysed in this study). The number of publications about reoperations in the ICU continues to be very limited, although recent data by LaPar et al.15 confirm an acute reoperation rate of around 5%, which does not seem to have decreased with the passage of time, and with a safety profile similar to ours.
Although not an objective of this study, it should be mentioned that there are potential advantages from a cost-efficiency standpoint of a well-indicated reoperation in the ICU compared with transfer to the operating room. The need for the participation of other medical professionals and the occupation of an operating room are key points that should be considered from a financial standpoint, while also guaranteeing the safety of patients operated on in situ.
Study limitations. This is a single-centre, retrospective study with methodological implications and a possible loss of data. The profile of indications and operations is varied and involves groups that are small in size, which may influence the consideration of the results. Occasionally, the terms may seem confusing as the codes were mixed. However, it represents the activity during a period of five years, which is sufficient to offer a profile of the average patient requiring acute reoperation in this setting.
In conclusion, ICU operations in cardiac surgery patients or those with cardiovascular pathology susceptible to surgery have represented 3.2% of cases in the study period. The rate of deep infection of the surgical wound was 0.9%, which is comparable to the rate observed in the general surgical population not operated on in the ICU. No complications have been detected in relation with the operations having been performed in the intensive care setting.
Surgery in the ICU can be done safely in an appropriate setting with trained staff.
FundingNo economic support was received for this study.
Authorship/CollaboratorsStudy design (JFE, PC, ES, EQ, DP, CAM), data acquisition and collection (JFE, ES, EQ, PC, CD, GV, RC, DP), analysis and interpretation of the results (JFE, EQ, PC, CD, GV, DP, MC, MJ, JLP, CAM), writing of the article (JFE, EQ, ES, MJ, DP, CAM), critical review (JFE, ES, EQ, MC, DP, RC, SN, CB, JLP, MJ, JM) and approval of the final version (JFE, EQ, ES, CD, PC, GV, DP, MC, RC, SN, CB, JLP, MJ, JM, CAM).
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Encalada JF, Campelos P, Delgado C, Ventosa G, Quintana E, Sandoval E, et al. Reintervenciones en una Unidad de Cuidados Intensivos de Cirugía Cardiovascular. Cir Esp. 2016;94:227–231.
Part of the data from this article was presented at the 22nd National Conference of the Spanish Society of Thoracic-Cardiovascular Surgery, Santiago de Compostela, 18–20 June, 2014.