Entamoeba histolytica is a protozoan that is transmitted through the fecal–oral route in areas of high-incidence, such as Asia, South Africa, South America or Central America. Amoebae invade the colon wall and can cause disease, ranging from asymptomatic to invasive colitis and even pleural, cardiac, cerebral or hepatic involvement,1 with liver involvement being the most frequent manifestation outside the colon. However, less than one-third of patients with invasive amoebiasis have concomitant colitis and liver abscess.2 When the liver is affected, it usually presents as a single abscess, frequently in the right hepatic lobe. Amoebic abscesses typically have significant potential for necrosis and a risk of rupture to the abdominal cavity, pleura or pericardium. The diagnosis is confirmed with serological tests, such as ELISA and PCR (positive in more than 90% of cases), the detection of antigens in feces, or the microbiological analysis of the affected tissue (which has a low sensitivity).3 Ultrasound and computed tomography (CT) can support the suspected diagnosis and provide information in case of complications.
We present the case of a 39-year-old man with no history of interest (no liver disease, and serologies were negative for hepatitis) and no recent trips abroad, who went to the Emergency Department of another hospital due to pain in the right upper quadrant that had been progressing over the previous week and fever of up to 39°C, with no diarrhea or other accompanying symptoms. Blood cultures were taken and an abdominal ultrasound was performed, which showed an abscess in liver segment VII measuring 32mm×23mm. Since the patient lacked an epidemiological history, the initial suspected diagnosis was pyogenic abscess, and empirical antibiotic therapy was started with Piperacillin/Tazobactam.
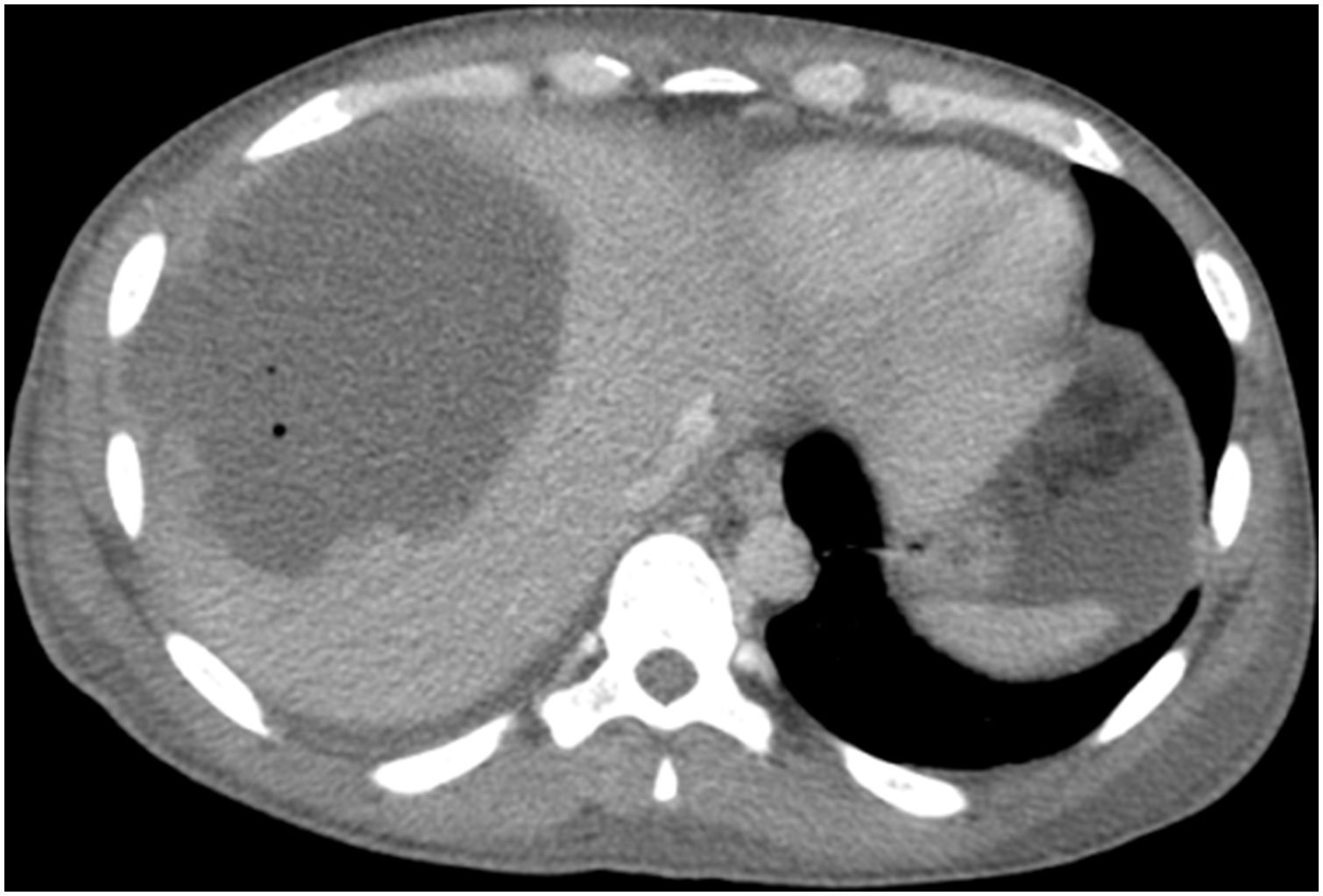
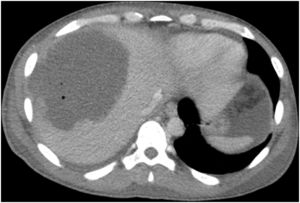
After 48h, an abdominal CT scan showed that the abscess had increased in size to 54mm×41mm, so percutaneous drainage was performed. Due to symptoms of acute abdomen, the abdominal CT was later repeated, which showed abscess growth to 130mm×95mm (Fig. 1) and distension of the ascending and transverse colon as well as free fluid without pneumoperitoneum. Surgeons decided to operate immediately, finding a perforation in the ascending colon. Right hemicolectomy was performed with terminal ileostomy and mucosal fistula, as well as surgical drainage of the hepatic abscess. During the postoperative period, the patient presented multiple organ failure and liver failure, so the surgeons decided to re-operate. Necrosis was observed in liver segments V, VI and VII, requiring necrosectomy and placement of drains in the liver abscess bed. Although the initial blood cultures were negative, new blood cultures and cultures of intraoperative samples grew Enterococcus faecium and Candida spp. Serology for E. histolytica was also positive. With these results, the treatment was modified to Meropenem, with the addition of Metronidazole, Fluconazole and Vancomycin. Since the situation of multiple organ failure persisted, the patient was transferred to our medical center for assessment by the Hepatobiliary and Pancreatic Surgery team. A new urgent surgery was indicated, during which another right hepatic necrosectomy was performed with temporary closure of the abdominal wall. Subsequently, the patient showed a tendency toward stabilization, which allowed us to intervene again and complete the right hepatectomy, extended to segment IVb due to extensive hepatic necrosis (Fig. 2), as well as proceeding with the wall closure. Reconstruction of the tract at that time was ruled out given the situation of sepsis. During the postoperative period, the septic symptoms improved with slow recovery of liver function, and Paromomycin was administered as eradication therapy. The microbiological analyses of the surgical specimens from the colon and liver abscess were positive for E. histolytica. The patient is currently alive, asymptomatic and has correct liver function one year later.
Although 90% of liver abscesses are pyogenic in origin, we should not forget that the remaining 10% are amoebic in origin. In addition, even though the incidence of amoebiasis is low in our country, autochthonous cases are increasing in frequency. Therefore, this disease should be considered in the initial study of any liver abscess, especially if it is a single abscess in the right hepatic lobe that shows negative cultures and does not improve with empirical antibiotic therapy.4
Without treatment, mortality is very high, but with adequate treatment the cure rate exceeds 90%.2 The management of an amoebic abscess is mainly based on antibiotic treatment with Metronidazole, followed by a luminal amebicide. Nevertheless, the evolution toward severe intra-abdominal sepsis, which frequently has associated bacterial superinfection as in this case, may require urgent surgery to control the septic focus.5,6 Percutaneous or surgical drainage is indicated only if the abscess is refractory to medical treatment, greater than 5cm, located in the left hepatic lobe, presents rupture with extension to the peritoneal, pericardial or pleural cavities, or has an uncertain etiology.7–9 Factors for a poor prognosis include the presence of hyperbilirubinemia, malnutrition, large or multiple abscesses, or central nervous system involvement.3,10
It is important for surgeons to know the biological markers of severe sepsis in order to choose the most appropriate time for and type of surgical intervention. In turn, these cases require multidisciplinary management that frequently motivates the referral of these patients to tertiary hospitals for optimal management and monitoring.
Please cite this article as: Serrano M, Lladó L, Ramos E, Lopez-Gordo S, Bravo A. Hepatectomía derecha y hemicolectomía derecha por necrosis hepática y perforación cólica causadas por Entamoeba histolytica. Cir Esp. 2019;97:412–413.