New technological advances have enabled the development of single-port laparoscopic surgery. This approach began with cholecystectomy and subsequently with other abdominal surgeries. However, few publications on laparoscopic liver surgery have described the use of complete single-port access. We present our initial experience of a single-port laparoscopic hepatectomy.
Materials and methodsBetween May 2012 and December 2013, 5 single-port laparoscopic hepatectomies were performed: 1 for benign disease and 4 for colorectal liver metastases. The lesions were approached through a 3–5cm right supraumbilical incision using a single-port access device. All the lesions were located in hepatic segments II or III. Four left lateral sectorectomies and 1 left hepatectomy were performed.
ResultsMedian operative time was 135min. No cases were converted to conventional laparoscopic or open surgery. The oral intake began at 18h. There were no postoperative complications and no patients required blood transfusion. The median hospital stay was 3 days. The degree of satisfaction was very good in 4 cases and good in 1. Patients resumed their normal daily activities at 8 days.
DiscussionSingle-port laparoscopic hepatectomy is safe and feasible in selected cases and may reduce surgical aggression and offer better cosmetic results. Comparative studies are needed to determine the real advantages of this approach.
Los avances tecnológicos han permitido el desarrollo de la cirugía laparoscópica por incisión única, iniciada con la colecistectomía y usada, posteriormente, para abordar otras enfermedades abdominales. Sin embargo, la cirugía hepática laparoscópica por puerto único es excepcional. Se presenta la experiencia inicial en cirugía hepática por incisión única.
Material y métodoEntre mayo de 2012 y diciembre de 2013 se intervino a 5 pacientes mediante abordaje laparoscópico por incisión única. La indicación quirúrgica fue por enfermedad benigna en un caso y maligna en 4. Para la colocación del dispositivo de puerto único se practicó una incisión supraumbilical derecha de 3–5cm. En todos los casos las lesiones estaban situadas en los segmentos II o III hepáticos. Se realizaron 4 seccionectomías laterales izquierdas y una hepatectomía izquierda.
ResultadosEl tiempo operatorio fue de 135min. No hubo casos de conversión a cirugía laparoscópica convencional ni a cirugía abierta. La dieta oral se inició a las 18h. No hubo complicaciones postoperatorias ni necesidad de transfusión sanguínea. La estancia hospitalaria mediana fue de 3 días. El grado de satisfacción fue muy bueno en 4 casos y bueno en uno y los pacientes retornaron a las actividades de la vida diaria a los 8 días.
DiscusiónLa cirugía hepática laparoscópica por incisión única es segura y factible en casos seleccionados y podría aportar menor agresión quirúrgica y mejores resultados estéticos. Se requieren estudios comparativos para determinar las ventajas reales de este abordaje.
The first laparoscopic liver resection in the world was performed in 1992,1 and the first in Spain took place in 2000.2 Laparoscopic liver surgery is a safe and feasible technique,3–5 however, for years it was used exclusively for minor resections.6 Greater experience of surgical groups coupled with technological advances have contributed to an expansion of prescriptions for major resections7 and malignant disease.8–11
Constantly advancing minimally invasive surgery and research in NOTES have enabled development of single-port laparoscopic surgery. This is another step toward progress in conventional laparoscopic surgery, and with miniports, further minimizing surgical invasiveness. Its theoretical advantages could be: earlier recovery, less postoperative pain, shorter hospital stay and better cosmetic results. Single-port laparoscopic surgery was first applied to procedures such as cholecystectomy12 and appendectomy13 and has subsequently been extended to other fields such as bariatric surgery, colon surgery or splenectomy.14–16 Its application in liver surgery is reduced today to publications of clinical case series.17–21
This is a report on our initial experience in single-port laparoscopic liver surgery where we discuss the technique's feasibility, incision size, postoperative complications, postoperative pain, length of stay, need for blood transfusion, pathological results, satisfaction and return to activities of daily living in patients undergoing this approach.
Materials and MethodsPatientsBetween May 2012 and December 2013 surgery was performed on 5 64-year-old patients, 3 men and 2 women (27–79 age range). Informed consent was obtained from all patients. Surgical indication was benign disease in 1 case (hydatid cyst) and malignant disease in 4 (hepatic metastases of colorectal cancer). The average number of lesions was 1 (1–2) and 24mm (7–62) in diameter located in hepatic segments II or III. Patient characteristics are described in Table 1.
Clinical Characteristics of Patients Undergoing Single-Port Liver Surgery.
| Case | Age | Gender | Pathology | ASA | Lesion site (segment) | Number of lesions | Maximum size (mm) |
| 1 | 27 | M | Hydatid cyst | I | II–III | 1 | 62 |
| 2 | 64 | F | M1 CRC | II | III | 1 | 24 |
| 3 | 61 | F | M1 CRC | II | II | 1 | 7 |
| 4 | 79 | M | M1 CRC | III | II–III | 2 | 15 |
| 5 | 67 | M | M1 CRC | III | III | 1 | 30 |
CRC, colorectal cancer; F, female; M, male.
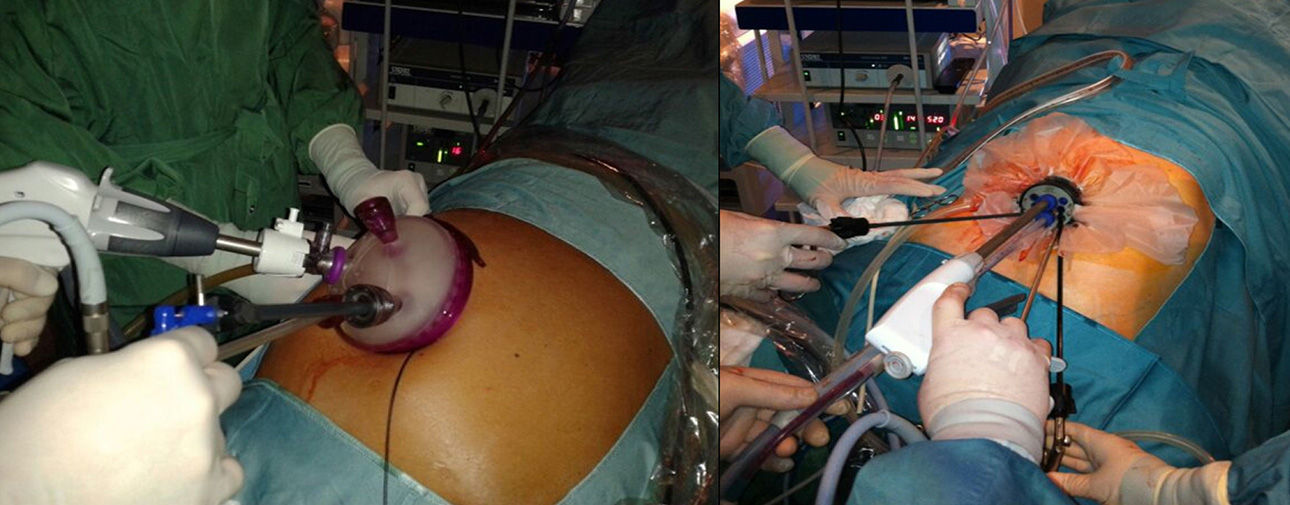
Patients were in supine position with legs spread apart and anti-Trendelenburg position. A right supraumbilical transverse incision was performed within the anterior sheath, and anterior rectus muscle laceration was performed to place the single-port device (GelPoint® Applied Medical, CA, USA, or Endocone® K. Storz, Tuttlingen, Germany). The GelPoint® disposable device was used to place 5 ports freely through the gel, and the multichannel and inventoried Endocone® device was used to work through its 8 different diameter channels (Fig. 1). Ten millimeter optics with 30° angle were used. Pneumoperitoneum pressure was set at 12mmHg. Intraoperative ultrasonography was performed in all cases.
Four left lateral sectionectomies (segments II and III) were performed and 1 left hepatectomy in 1 case with a 30mm lesion in segment III in close contact with the left portal vein, forcing resection of segment IV.
Lateral sectionectomies included left hepatic lobe mobilization, sectioning the round, falciform and left triangular ligaments. Hepatic transection began with the harmonic scalpel (Ultracision®, Ethicon Endosurgery, Johnson and Johnson Ltd., Cincinnati, OH, USA) for the first 0.5–1cm of liver surface and from this depth, vessels were dissected with ultrasonic dissector (CUSA® Integra Life Sciences Corporation, Cincinnati, OH, USA), and coagulated with monopolar dissector (Tissuelink®, EndoFB3.0 FloatingBall, Medtronic Advanced Energy, LLC, Minnesota, USA) or Ultracision®. The sectioning of portal pedicles in segments II and III and left suprahepatic vein was performed using a linear mechanical stapler with vascular load (45mm ETS, Linear Cutter, Ethicon Endosurgery Inc., Cincinnati, USA).
For the left hepatectomy, the left hepatic lobe was mobilized, sectioning the round, falciform and left triangular ligaments. Intra-Glissonian approach was used for cholecystectomy and left hilar pedicle dissection, clamping the left hepatic artery and left portal branch (hem-o-lok® Ligation System, Teleflex Medical EOM, North Carolina, USA). Liver transection was performed in the same manner described above. At the intrahepatic level, the left hepatic duct and the left hepatic vein were sectioned and clamped with a vascular mechanical stapler.
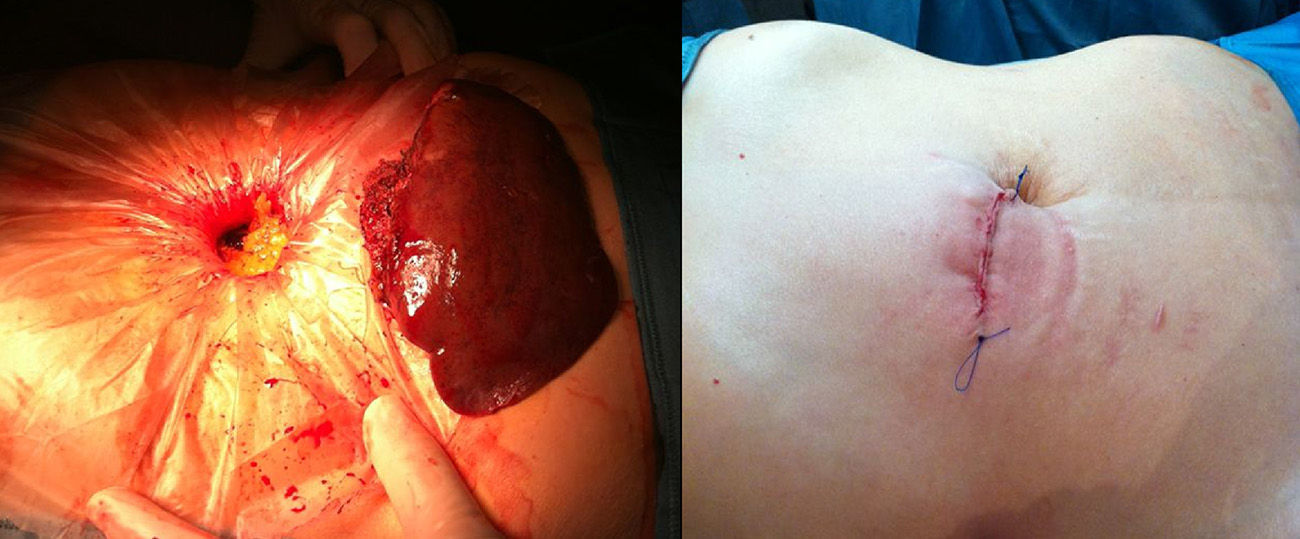
Liver transection was performed in all cases without preparation for hilar occlusion; rigid instruments were used. Hemostasis with monopolar coagulation and hemostatic sponge was revised (TachoSil® medicated sponge, Takeda-Nycomed Austria GmbH, Linz, Austria). A drain was left in 2 cases by the surgeon's subjective decision. The surgical specimen was extracted by the single incision and laparotomy was closed in layers with absorbable sutures in peritoneum and nonabsorbable for the anterior sheath (Fig. 2).
A record was entered for incision size, surgery time and if there was a need for conversion.
Postoperative ManagementAfter surgery, patients received analgesic treatment by epidural catheter with levobupivacaine 0.125% plus fentanyl 2mL (1mcg/mL) at 8–10mL/h or IV treatment with tramadol infusion 400mg plus haloperidol 5mg at 11mL/h, as decided by the anesthesiologist. Paracetamol 500mg/6h was administered as added conventional IV treatment plus dexketoprofen 50mg/8h and morphine sc 5mg/8h if VAS>3. Time of analgesia administration by epidural catheter or by IV infusion and the need for rescue analgesia were assessed (by days). Postoperative pain was measured by visual analog scale (VAS) from 0 to 10 during the first 3 postoperative days, up to 24h after stopping treatment by epidural catheter for applicable cases.
Oral intake start was recorded (by hours) after completion of surgery. Postoperative complications were recorded based on the Clavien–Dindo classification, need for blood transfusion as assessment of intraoperative and postoperative bleeding, and average stay in days.
During the first outpatient monitoring visit, the degree of esthetic satisfaction by categories (poor, fair, good or very good) was assessed and recorded (by days) at the time patients went back to most activities of daily living. Histological diagnosis and surgical margins of lesions were reviewed.
Here are the results from variables including median and range.
ResultsSingle port surgery was completed in all cases. There was no conversion to conventional laparoscopy or open surgery. Incision at the right supraumbilical level was 5cm (3–5 range). Intraoperative ultrasound ruled out other lesions. Operative time was 135min (120–210 range).
Three of the 5 patients received epidural catheter analgesic treatment for 24h (24–48h range), and 2 were treated with continuous infusion IV analgesia for 36h (24–48h range). No patients required rescue analgesics. Postoperative pain according to the VAS scale for pain was 0.8 (0–1.9 range) at first postoperative day, 1.2 (0–1.8 range) at second day, and 0 (0–1 range) on the third day after hepatectomy.
Patients began oral feeding at 18h (12–18h range). There were no postoperative complications based on the Clavien–Dindo classification. Hospital stay was 3 days (3–4 range) and none of the patients needed blood transfusion.
Degree of satisfaction was very good in 4 cases and good in 1, and recovery of daily activities occurred at 8 days (5–8 range). Diagnoses were confirmed histologically and resection margins were negative (Table 2).
Results.
| Case | Incision (cm) | Surgical technique | Single-port device | Surgery time (min) | Pain 24h after surgery (VAS) | Pain 72h after surgery (VAS) | Hospital stay (days) | Surgical margin (mm) | Level of satisfaction |
| 1 | 4 | LLS | Endocone® | 135 | 1.9 | 0 | 3 | 4 | Good |
| 2 | 3 | LLS | Endocone® | 180 | 0.3 | 0 | 3 | 1 | Very good |
| 3 | 5 | LLS | GelPoint® | 120 | 0.8 | 0 | 3 | 25 | Very good |
| 4 | 5 | LLS | GelPoint® | 120 | 0 | 0 | 4 | 5 | Very good |
| 5 | 5 | LH | GelPoint® | 210 | 1.2 | 1 | 4 | 20 | Very good |
LH, left hepatectomy; Hosp, hospital; Postop, postoperative; LLS, left lateral sectionectomy.
Laparoscopic liver surgery is a feasible technique providing less surgical aggression and better cosmetic results. This has made it well accepted by most surgeons.
Some groups have published their experience with single port surgery in different surgical fields, but most are case series reporting few cases. Randomized studies are needed to confirm its theoretical advantages.
Hepatic single port surgery is not widespread, and limited to isolated cases. Initial publications are on benign lesions and subsequently expand to treating malignant disease such as metastasis and hepatocellular carcinoma, with results similar to those of conventional laparoscopy.21,17,22–24
In 2000 we started laparoscopic liver surgery at our center, initially with benign lesions, subsequently covering a larger range of indications. Currently, all left lateral sectionectomies are treated with minimally invasive surgery,25 given favorable anatomical conditions in this sector, as well as some limited resections and major hepatectomy in selected cases.
In 2009, we started using single-incision laparoscopic cholecystectomy.26 This allowed to acquire enough training to develop single-port liver surgery from 2012.27
Our initial experience shows that single port technique is feasible and safe in selected cases. In all cases the surgery was completed without conversion to conventional laparoscopic surgery or open surgery and no complications were reported. Mean operative time was 153min, similar to that described in other publications.18–21 Time invested on left hepatectomy lengthens the average time spent in our cases; 138min are for left side sectionectomy.
From the histological point of view, metastatic colorectal carcinoma resection margins were all negative allowing adequate oncologic resection of the lesions.
One limitation of this approach is based on the technical difficulty of the lack of space and triangulation through a single-port. Therefore, we have developed multiple articulated instruments to facilitate surgery. In our experience, it is essential to use articulated instruments, because when a right supraumbilical incision is performed the proper working angle is available on the surface of the left liver lobe allowing a linear transection be performed with rigid instruments.
Robotics can solve the triangulation and discomfort problems of single port surgery. There have been some cases of liver resections by single-port robotic surgery28,29 but its high cost makes it unavailable in most centers.
In conclusion, hepatic single-port surgery is safe and feasible and according to our initial experience, indicated for lesions located in the left hepatic lobe without contraindication for laparoscopic surgery. It may reduce surgical aggression and provide better cosmetic results. However, more comparative studies are needed to prove it.
Conflict of InterestThe authors declare having no conflict of interest.
Please cite this article as: Camps Lasa J, Cugat Andorrà E, Herrero Fonollosa E, García Domingo MI, Sánchez Martínez R, Vargas Pierola H, et al. Abordaje laparoscópico por incisión única del hígado izquierdo: experiencia inicial. Cir Esp. 2014;92:589–594.
Some information contained in this paper was delivered as an oral presentation at the IX Congrés de la Societat Catalana de Cirurgia [IX Congress of the Catalan Society of Surgery], October 17–18, 2013 and in video format at the XIX National Surgery Meeting, Burgos, October 23–25, 2013. A summary has been sent to the 2014 National Surgery Congress, Madrid.