To evaluate the efficacy, safety and clinical and oncological results of colonic stents in the initial therapeutic strategy of obstructive left colon cancer.
MethodsDescriptive and ambispective study (2008–2018) of patients with clinical and radiological diagnosis of neoplastic obstruction of the left colon in whom a colonic stent was indicated, analyzing the following groups: palliative stent, stent as bridge to surgery and urgent surgery in case of stent failure or complications.
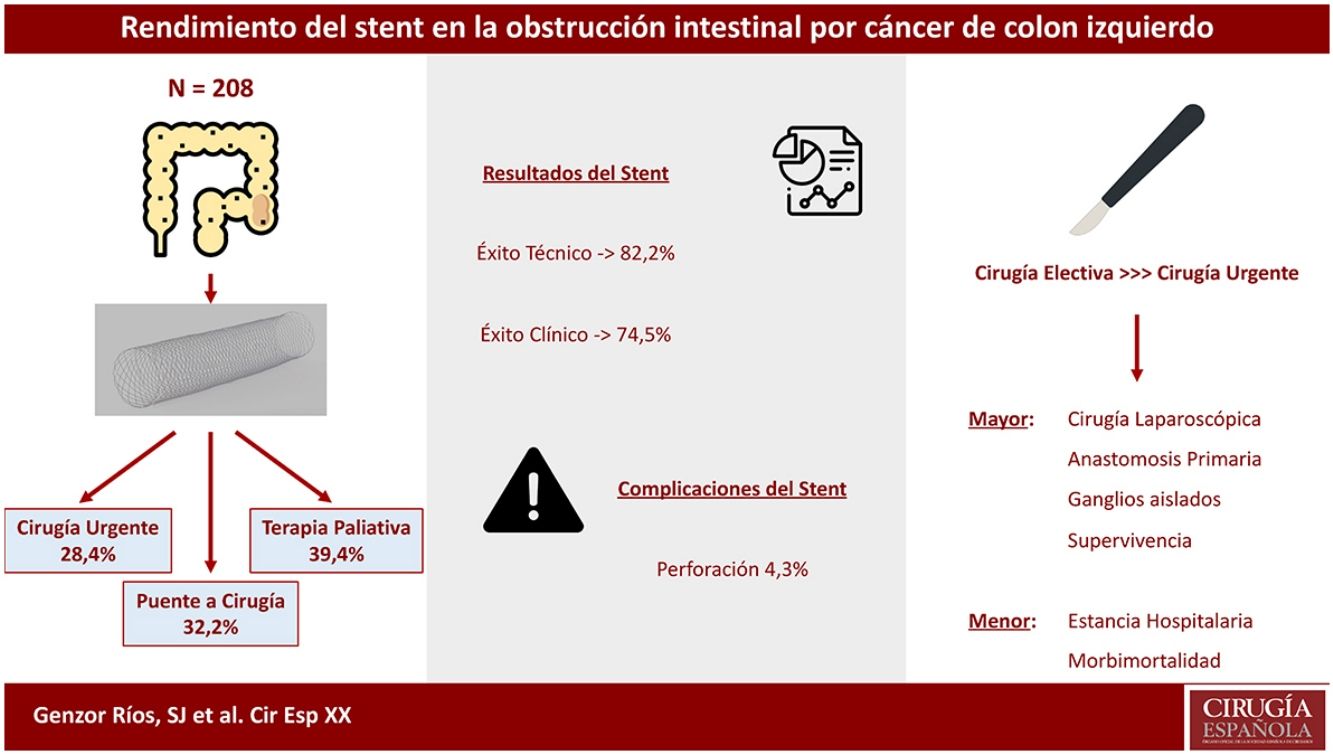
ResultsThe study included 208 patients. The technical and clinical success rates were 82.2% and 74.5%, respectively, with associated perforation in 4.3% of the sample. In 32.2%, the stent was placed as bridge to surgery, while 28.4% required urgent surgical intervention. The stent was placed with palliative intent in 39.4%. The proportion of laparoscopic surgery, oncological resection, primary anastomosis and lymph nodes resected were higher in patients undergoing elective surgery than in urgent surgery, with shorter postoperative stay and less severe postoperative morbidity and mortality. Stage II–III patients with oncological tumor resection who underwent elective surgery had increased survival compared to those who underwent urgent surgery (P = .001).
ConclusionsInitial treatment of neoplastic obstruction of the left colon with a stent is an effective strategy in elective surgery and avoids permanent colostomy in palliative patients, although complications or stent failure lead to urgent surgery in almost one-third of patients.
Evaluar la eficacia, seguridad y resultados clínicos y oncológicos del stent colónico en la estrategia terapéutica inicial de la obstrucción intestinal por cáncer de colon izquierdo.
MétodosEstudio descriptivo y ambispectivo (2008–2018) de pacientes con diagnóstico clínico y radiológico de obstrucción neoplásica de colon izquierdo en los que se indicó colocación de stent, analizando los grupos de stent paliativo, stent como puente a cirugía y cirugía urgente por fallo o complicaciones del stent.
ResultadosEl estudio incluyó 208 pacientes. La tasa de éxito técnico y clínico fue del 82,2% y 74,5%, respectivamente, asociando perforación en el 4,3% de la muestra. En el 32,2% el stent se comportó como puente a cirugía, mientras que el 28,4% de los pacientes precisaron intervención quirúrgica urgente. En el 39,4% el stent fue colocado con intención paliativa. La proporción de cirugía laparoscópica, resección oncológica, anastomosis primaria y ganglios obtenidos fue superior en los pacientes sometidos a cirugía electiva frente a la urgente, siendo menor la estancia postoperatoria y la morbimortalidad postoperatoria grave. Los pacientes en estadio II–III con resección tumoral oncológica intervenidos de forma programada presentaron mayor supervivencia frente a aquellos intervenidos de urgencia (p = 0,001).
ConclusionesEl tratamiento de la oclusión neoplásica de colon izquierdo mediante stent supone una estrategia eficaz para operar de forma electiva un número importante de pacientes y evita la colostomía en pacientes paliativos, aunque las complicaciones o el fracaso de la técnica conllevan cirugía urgente en casi un tercio de los pacientes.
The therapeutic approach to intestinal obstruction due to colorectal cancer (CRC) is focused on 2 fundamental aspects: quickly and effectively resolving the intestinal occlusion; and obtaining the best oncological results.
Stent placement was first proposed as a treatment for neoplastic colon obstruction a quarter of a century ago.1 This strategy made it possible to treat the obstruction as a “bridge therapy” to conventional elective surgery with primary anastomosis after preparation of the colon, allowing for a minimally invasive approach to be used2 with lower overall costs and morbidity than urgent surgery.3 In addition, in advanced cases, it represented a palliative treatment that would prevent colostomy.4
The effectiveness of the procedure exceeds 70%–80% in most series,5 and the most important secondary complications are perforation, stent migration and tumor obstruction of the device. Perforation is the most serious of these, with a mortality rate of up to 20%–30%,6 which has led to the suspension of clinical trials.7,8
The oncological results are controversial when stents are used as a bridge to surgery versus urgent surgery, and some studies have registered a higher rate of local recurrence.9,10 However, no meta-analysis performed to date has demonstrated differences in the long-term survival of these patients.11,12
Therefore, and given the methodological heterogeneity of the reports in the literature, the objective of this study was to describe and analyze the efficacy, safety, and clinical and oncological results in patients with neoplastic obstruction of the left colon who were candidates for initial treatment with a stent at a tertiary hospital, analyzed according to the therapeutic strategy: urgent surgery, bridge therapy or palliative therapy. The oncological outcome of the therapeutic process is described for each of these study groups.
MethodsA descriptive, observational, uncontrolled and ambispective study (retrospective between 2008 and 2015 and prospective from 2016 to 2018) of successive patients diagnosed clinically and radiologically by abdominal CT scan with intestinal obstruction due to cancer of the left colon between the splenic angle and upper rectum, for which the initial indicated treatment was stent placement. Patients were treated at a tertiary teaching hospital with an area of influence of 400,000 inhabitants.
Excluded from the study were patients with extra-colonic neoplastic or benign obstruction, patients who were hemodynamically unstable (systolic blood pressure, SBP < 90 mmHg) and patients with clinical or radiological evidence of perforation (pneumoperitoneum, abscess or cecal pneumatosis).
In all cases, the radiological procedure was performed by the Interventional Radiology Unit at the hospital after obtaining informed consent for the technique. A bare-metal stent (Wallflex®, Boston Scientific, Natick, Massachusetts, United States) measuring 90–120 mm in length and 25 mm in diameter was implanted transrectally.
Technical success was defined as the proper placement and expansion of the stent, surpassing the tumor, while clinical success was the clinical and radiological resolution of the obstruction 48 h later. Likewise, clinical performance was defined and quantified as the final rate of patients of the series who were candidates for the procedure, experienced clinical success and no complications, and who thereby avoided urgent surgery.
The causes of failure and evolutionary complications secondary to stent implantation were recorded. Early stent-related complications were those that occurred during the first two weeks after the procedure. Cases with clinical success were discussed in the Hospital CRC Committee, indicating elective surgery or palliative therapy with or without systemic treatment. In the case of elective surgery, the procedure was performed by surgeons of the Coloproctology Surgery Unit, while patents requiring urgent surgery were treated by general surgeons from the on-call teams.
The 30-day postoperative surgical morbidity rate was recorded according to the Clavien-Dindo scale,13 and the American Joint Committee on Cancer classification14 was using for tumor staging.
All patients were clinically monitored by the Medical Oncology and Surgery Departments, following the protocol established at the hospital. The standard mean oncological follow-up was 5 years, and the mean of our series was 2.5 years. For the survival study, the period between the obstructive episode and death was monitored, with censoring of the data of those patients who were still alive at the end of the follow-up period.
The following variables were recorded: a) epidemiological: age, sex and tumor location; b) technical: technical success, clinical success and complications; c) treatment type: bridge therapy, palliation and urgent surgery; d) surgical: rate of laparoscopic surgery, rate of oncological resection, rate of primary anastomosis, days of hospital stay, and morbidity and mortality; and e) oncological: tumor stage, lymphadenopathies and 3- and 5-year survival rates.
For the statistical analysis, the IBM SPSS Statistics 24® program was used, with a descriptive study of the variables. The mean was calculated for normally distributed variables with the Kolmogorov–Smirnov test, while the median was calculated for those that were not. In the comparative study of the variables, the Student’s t test, ANOVA and Mann–Whitney U test were applied for quantitative variables, and the chi-squared was used for qualitative variables. Kaplan Meier curves and the log-rank test were used for the survival analysis. The multivariate survival analysis was performed with a Cox regression model, and the result was expressed as a hazard ratio (HR). Results with a P value <.05 were considered statistically significant.
The study was evaluated and approved by the Hospital Ethics Committee.
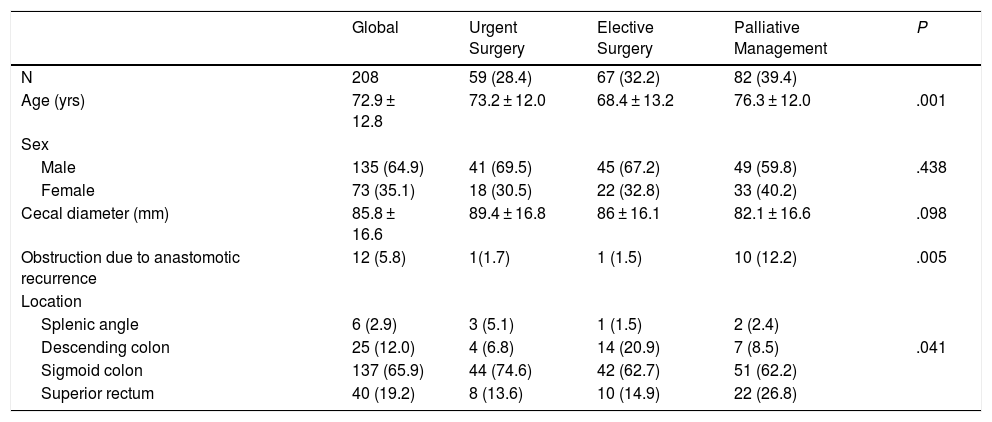
Results208 patients were included. The baseline characteristics of the sample are shown in Table 1: the average patient age was 72, with a predominance of males. Tumor obstruction was specifically located in the sigmoid colon and rectum, with an average cecal diameter of 85 mm.
Epidemiological Variables of the Sample.
| Global | Urgent Surgery | Elective Surgery | Palliative Management | P | |
|---|---|---|---|---|---|
| N | 208 | 59 (28.4) | 67 (32.2) | 82 (39.4) | |
| Age (yrs) | 72.9 ± 12.8 | 73.2 ± 12.0 | 68.4 ± 13.2 | 76.3 ± 12.0 | .001 |
| Sex | .438 | ||||
| Male | 135 (64.9) | 41 (69.5) | 45 (67.2) | 49 (59.8) | |
| Female | 73 (35.1) | 18 (30.5) | 22 (32.8) | 33 (40.2) | |
| Cecal diameter (mm) | 85.8 ± 16.6 | 89.4 ± 16.8 | 86 ± 16.1 | 82.1 ± 16.6 | .098 |
| Obstruction due to anastomotic recurrence | 12 (5.8) | 1(1.7) | 1 (1.5) | 10 (12.2) | .005 |
| Location | .041 | ||||
| Splenic angle | 6 (2.9) | 3 (5.1) | 1 (1.5) | 2 (2.4) | |
| Descending colon | 25 (12.0) | 4 (6.8) | 14 (20.9) | 7 (8.5) | |
| Sigmoid colon | 137 (65.9) | 44 (74.6) | 42 (62.7) | 51 (62.2) | |
| Superior rectum | 40 (19.2) | 8 (13.6) | 10 (14.9) | 22 (26.8) | |
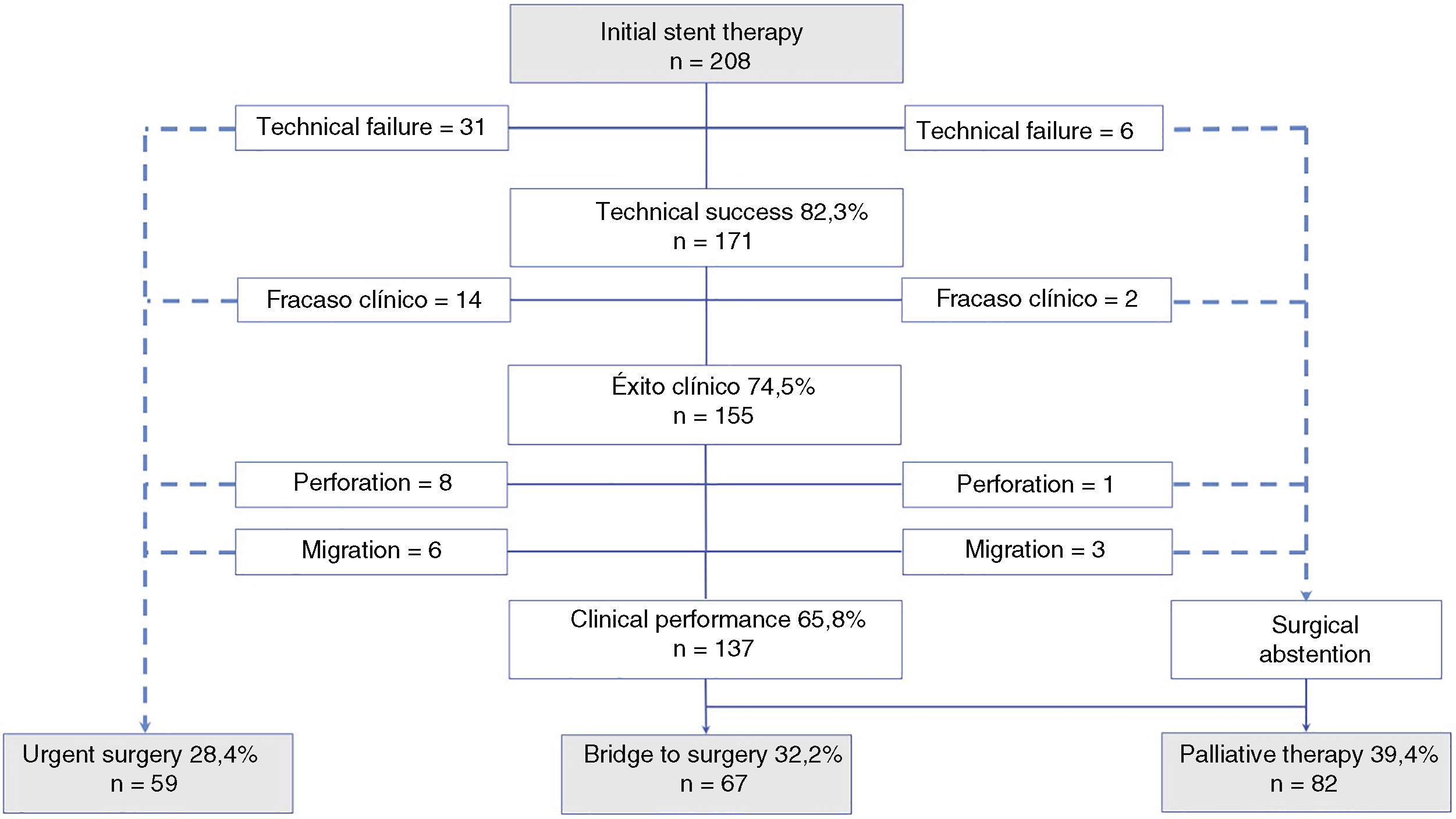
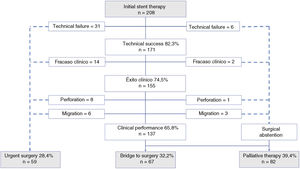
Fig. 1 is a flowchart of the patients in the series, which shows a technical success rate of 82.3% (171) and a clinical success rate of 74.5% (155), with a clinical yield of 65.8% (137) of the sample. In this final group of patients, 48.9% (67) were candidates for “bridge therapy” to elective surgery, and in 51.1% (70) the stent treatment was considered a definitive palliative therapy. The median hospital stay after stent placement, excluding patients who required urgent surgery and those in whom elective surgery was performed during admission, was 6 days.
Flow diagram of patients with neoplastic obstruction of the left colon who were candidates for initial stent treatment. Terapia inicial con stent = Initial stent therapy; Fracaso técnico = Technical failure; Perforación = Perforation; Migración = Migration; Puente a cirugía = Bridge to surgery; Cirugía urgente = Urgent surgery; Abstención quirúrgica = Surgical abstention; Terapia paliativa = Palliative therapy; Rendimiento clínico = Clinical performance; Éxito técnico = Technical success. CAMBIAR LOS “,” A “.”.
Larger mean cecal diameter was observed in patients with clinical failure compared to those who had clinical success (P = .032). The other variables associated with failure of the technique were age (P = .012) and the tumor being located in the splenic angle (P = .002).
59 patients (28.4%) underwent urgent surgical treatment due to failure of the technique or the appearance of specific complications. There were 18 cases (8.6%) of early postoperative complications: perforation in 9 cases (4.3%) and stent migration in 9 (4.3%), which led to urgent surgery in 14 patients. In the case of perforation, one death was recorded within 30 days (33%; 3). Late complications appeared in 18.3% (15) of the palliative treatment group.
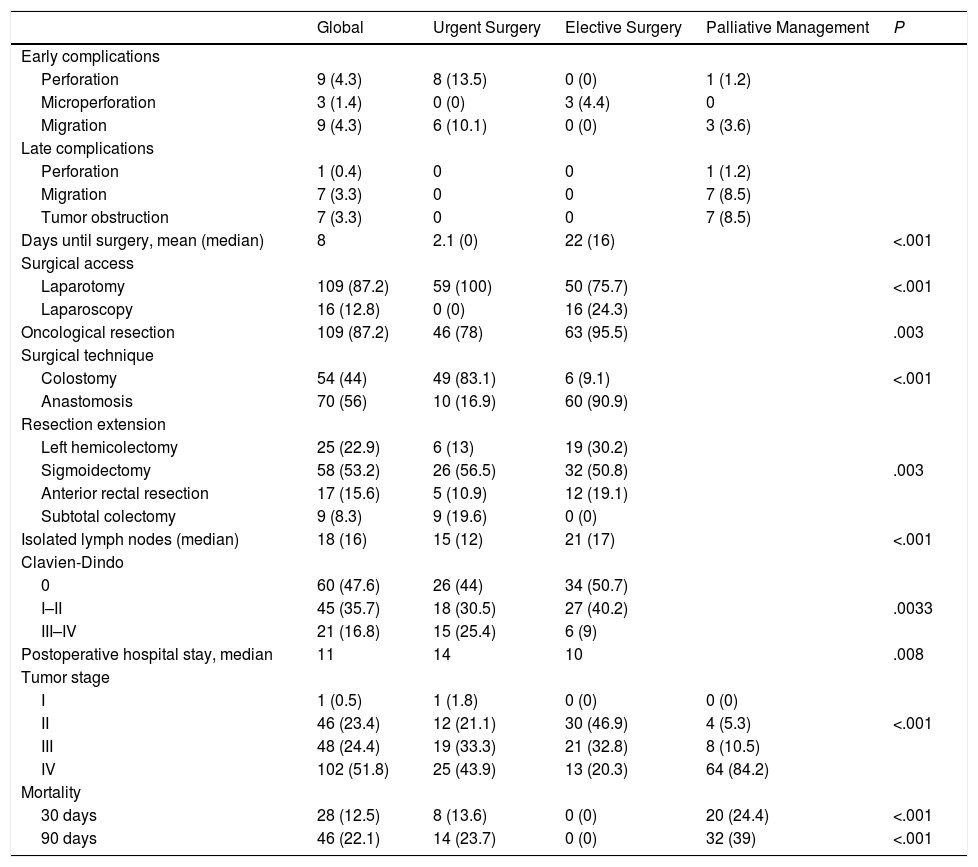
Regarding the surgical variables (Table 2), 24.3% of the patients from the elective surgery group were treated laparoscopically: one intervention was performed with optimal criteria for oncological radicality in 95% of cases versus 78% of the urgent surgery group, with a mean number of isolated lymphadenopathies in both groups of 21 and 15, respectively. Likewise, the primary anastomosis rate was much higher in the elective surgery group (90.9%) compared to the urgent surgery group (16.9%), where 5 colorectal anastomoses were performed after intraoperative colonic lavage as well as 4 ileorectal anastomoses. The average time elapsed until elective surgery was 16 days. Severe morbidity (Clavien III–IV) was significantly lower in the elective surgery group (9%) compared to urgent surgery (25.4%). A mortality rate (Clavien V) of 13.6% was obtained in urgent surgery versus 0% in elective surgery. Anastomotic dehiscence was recorded in 11% (1) of patients treated by urgent surgery and 2.9% (2) of the patients who underwent scheduled treatment. In all cases, the differences obtained between the 2 surgical groups were statistically significant.
Variables for Clinical, Surgical and Oncological Results.
| Global | Urgent Surgery | Elective Surgery | Palliative Management | P | |
|---|---|---|---|---|---|
| Early complications | |||||
| Perforation | 9 (4.3) | 8 (13.5) | 0 (0) | 1 (1.2) | |
| Microperforation | 3 (1.4) | 0 (0) | 3 (4.4) | 0 | |
| Migration | 9 (4.3) | 6 (10.1) | 0 (0) | 3 (3.6) | |
| Late complications | |||||
| Perforation | 1 (0.4) | 0 | 0 | 1 (1.2) | |
| Migration | 7 (3.3) | 0 | 0 | 7 (8.5) | |
| Tumor obstruction | 7 (3.3) | 0 | 0 | 7 (8.5) | |
| Days until surgery, mean (median) | 8 | 2.1 (0) | 22 (16) | <.001 | |
| Surgical access | <.001 | ||||
| Laparotomy | 109 (87.2) | 59 (100) | 50 (75.7) | ||
| Laparoscopy | 16 (12.8) | 0 (0) | 16 (24.3) | ||
| Oncological resection | 109 (87.2) | 46 (78) | 63 (95.5) | .003 | |
| Surgical technique | <.001 | ||||
| Colostomy | 54 (44) | 49 (83.1) | 6 (9.1) | ||
| Anastomosis | 70 (56) | 10 (16.9) | 60 (90.9) | ||
| Resection extension | .003 | ||||
| Left hemicolectomy | 25 (22.9) | 6 (13) | 19 (30.2) | ||
| Sigmoidectomy | 58 (53.2) | 26 (56.5) | 32 (50.8) | ||
| Anterior rectal resection | 17 (15.6) | 5 (10.9) | 12 (19.1) | ||
| Subtotal colectomy | 9 (8.3) | 9 (19.6) | 0 (0) | ||
| Isolated lymph nodes (median) | 18 (16) | 15 (12) | 21 (17) | <.001 | |
| Clavien-Dindo | |||||
| 0 | 60 (47.6) | 26 (44) | 34 (50.7) | .0033 | |
| I–II | 45 (35.7) | 18 (30.5) | 27 (40.2) | ||
| III–IV | 21 (16.8) | 15 (25.4) | 6 (9) | ||
| Postoperative hospital stay, median | 11 | 14 | 10 | .008 | |
| Tumor stage | <.001 | ||||
| I | 1 (0.5) | 1 (1.8) | 0 (0) | 0 (0) | |
| II | 46 (23.4) | 12 (21.1) | 30 (46.9) | 4 (5.3) | |
| III | 48 (24.4) | 19 (33.3) | 21 (32.8) | 8 (10.5) | |
| IV | 102 (51.8) | 25 (43.9) | 13 (20.3) | 64 (84.2) | |
| Mortality | |||||
| 30 days | 28 (12.5) | 8 (13.6) | 0 (0) | 20 (24.4) | <.001 |
| 90 days | 46 (22.1) | 14 (23.7) | 0 (0) | 32 (39) | <.001 |
As for the tumor stage, 51.8% belonged to stage IV and 23.4% and 24.4% to stages II and III, respectively. A progressively higher proportion of stage IV patients has been observed in the different resulting therapeutic strategies: elective surgery (20.3%), urgent surgery (43.9%) and palliation (84.2%).
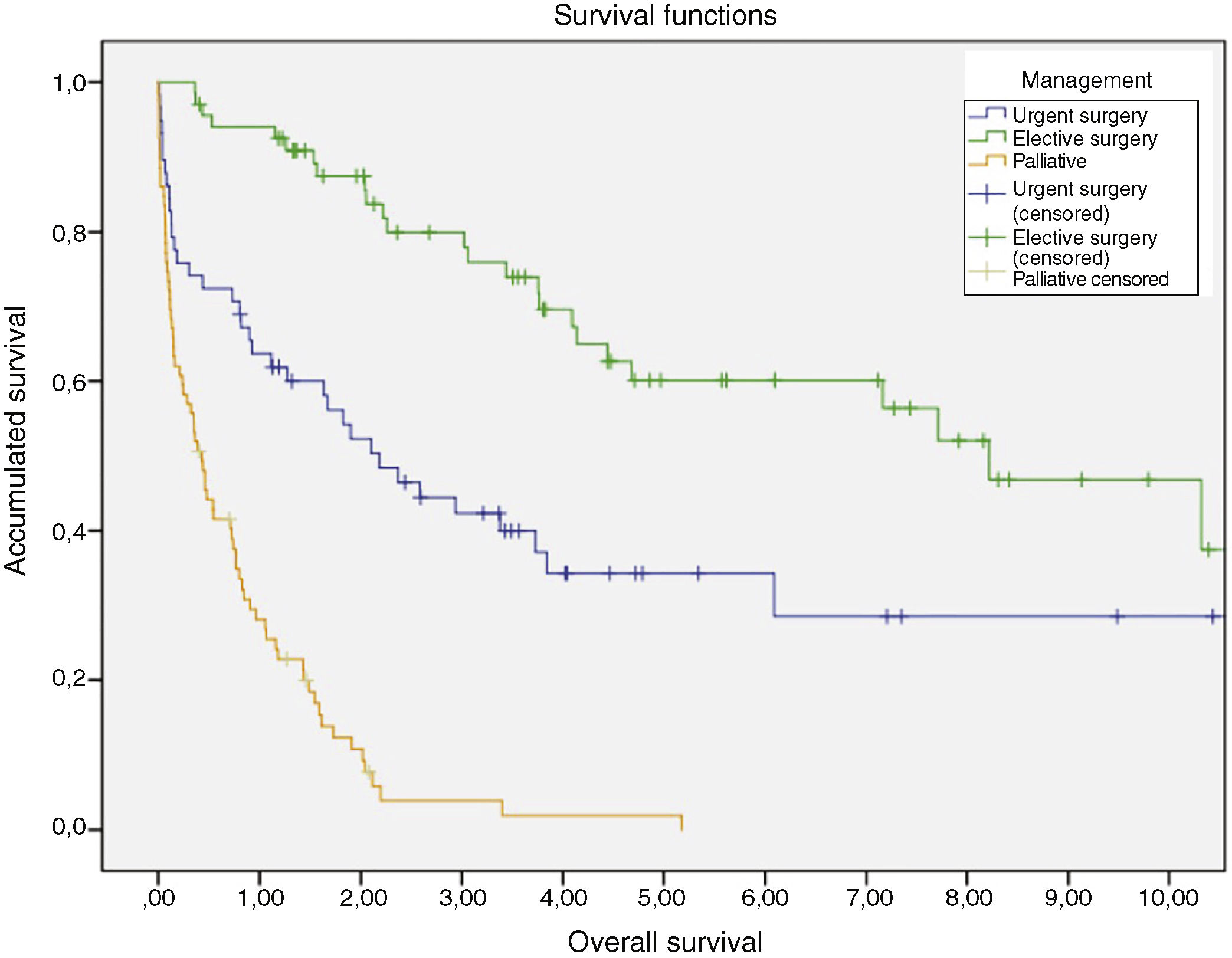
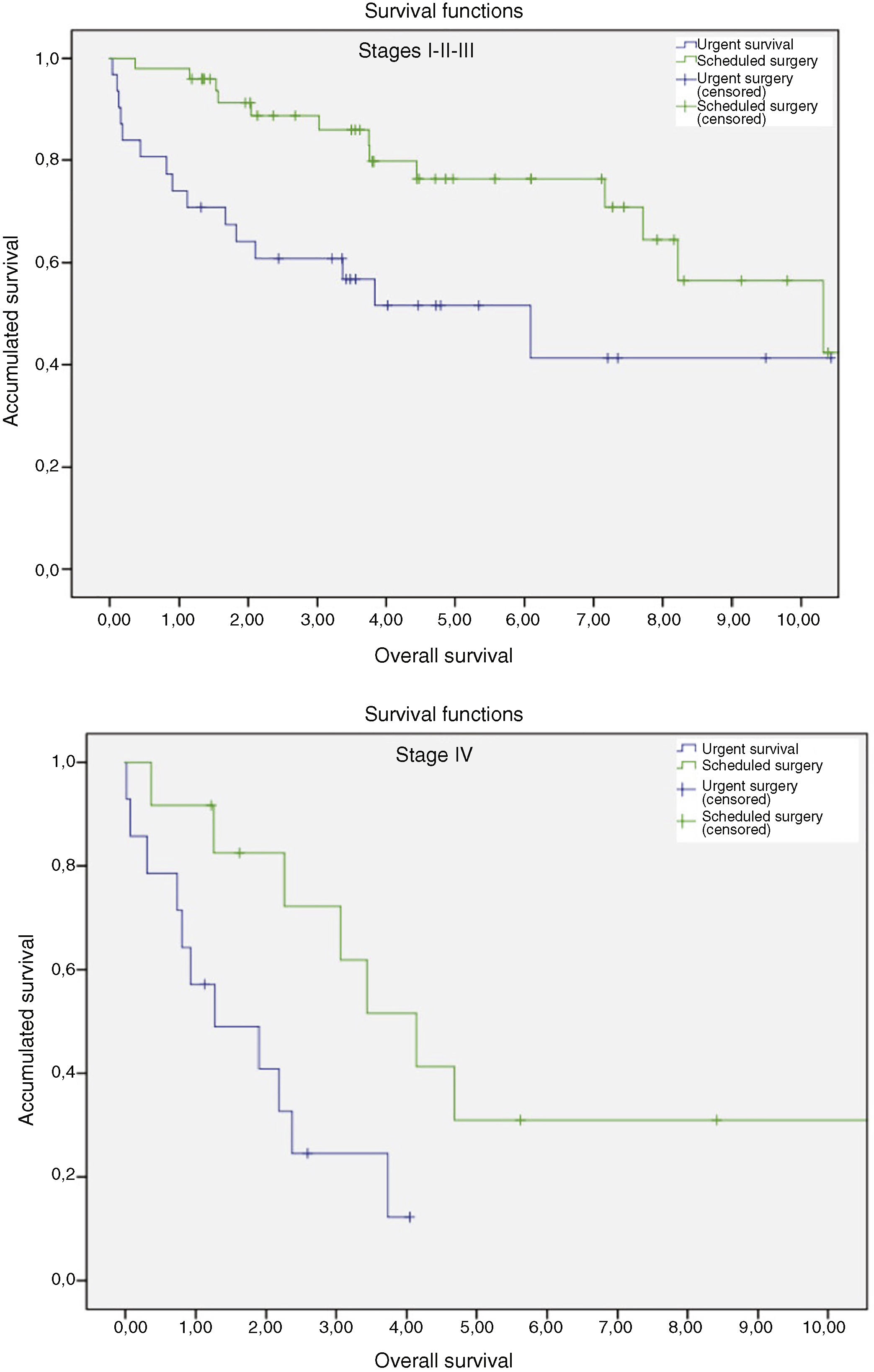
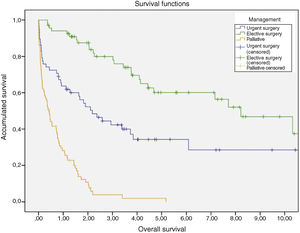
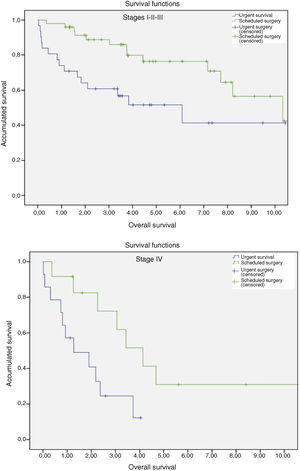
Survival rates were compared between the urgent and scheduled surgery groups, and patients in stage IV were excluded: the highest survival rate was in the group with stent placement as a bridge to surgery (log-rank 11,784; p = 0.001). The time elapsed between stent insertion and elective surgery did not influence the oncological outcome. A multivariate Cox survival model was generated for patients receiving urgent versus scheduled treatment, which showed that stage IV and age (increased risk per decade) were the only factors associated with poorer survival (HR 2.771; 95%CI 1.516–5.065; p = 0.001 and HR 1.634; 95%CI 1.211–2.204; p = 0.001, respectively). The data and survival curves are shown in Figs. 2 and 3. The median survival in patients with palliative management was 8.4 months.
Survival curves according to management. Funciones de supervivencia = Survival functions; Supervivencia global = Overall survival; Supervivencia acumulada = Accumulated survival; Manejo = Management; Cirugía urgente = Urgent surgery; Cirugía urgente-censurado = Urgent surgery (censored); Cirugía electiva = Elective surgery; Cirugía electiva-censurado = Elective surgery (censored); Paliativo = Palliative; Paliativo-censurado = Palliative censored.
Survival curves after urgent surgery versus elective surgery in patients with oncological tumor resection, according to stages. Funciones de supervivencia = Survival functions; Estadios = Stages; Supervivencia acumulada = Accumulated survival; Supervivencia global = Overall survival; Estadio = Stage; Cirugía urgente = Urgent survival; Cirugía programada = Scheduled surgery; Cirugía urgente-censurado = Urgent surgery (censored); Cirugía programada-censurado = Scheduled surgery (censored). CAMBIAR LOS “,” A “.”.
The use of colonic stents as a therapeutic alternative to emergency surgery is a well-known and widely-discussed option in the literature. However, there are still controversies regarding its generalized use due to the disparity of criteria proposed by different studies, the limited number of published series and the lack of methodologically appropriate studies, as demonstrated by the suspension of certain clinical trials,9,15 meta-analysis results and conclusions of the systematic reviews of the literature.5,12,16
Currently, there is not enough evidence to recommend the use of stents over other techniques, although the conclusions of the guidelines by the World Society of Emergency Surgery 2017 indicate that the use of stents as a bridge therapy provides obvious clinical benefits compared to urgent surgery, although they argue that more studies are necessary to evaluate their superior oncological results.17
Therefore, given the heterogeneity of the data provided in the literature, the lack of specific results and their difficult interpretation, the aim of our study was to analyze the actual future of intestinal obstruction management with stents by monitoring the evolution of all patients from admission to resolution of symptoms in terms of the 3 established groups.
In our opinion, as it is a single-center and numerically important series, it allows us to compare the different controversies, results and published recommendations with greater ‘realism’. The technical and clinical success rate obtained of 80–90% is consistent with reports from retrospective studies18,19 and even improves upon the rates published in meta-analyses and clinical trials.16,20 However, if we consider the ‘real’ clinical effectiveness of the procedure expressed by clinical performance, a 65.8% rate is obtained, representing patients who benefited from stent placement. We have not had experience with other types of metallic stents, such as the TTS-SMS (super-flexible through-the-scope self-expandable metallic stent) made of nitinol, which has been shown to improve the technical success rate and which, in addition, is recommended as a safe alternative for splenic angle and proximal colonic neoplastic obstructions.21
Regarding the end points of the process (urgent surgery, bridge therapy and palliation), which are difficult to compare in most of the published studies, each one represents approximately one-third of the sample. More than one-quarter of the series (28.4%) required urgent surgery due to complications of the procedure, failure to insert the stent or persistence of obstructive symptoms.
Although 8.6% of early complications were recorded in association with the technique (perforation and migration), this rate is consistent with the references. Our perforation rate of 4.3% is lower than reports in similar series4,18,22 and certain clinical trials.8,15 In an analysis of the Spanish ANACO workgroup on 1111 patients who had undergone surgery for left colon cancer,23 it was reported that the stent was positioned in 63 patients with a perforation rate similar to our study (4.8%). Asymptomatic perforation was observed in 1.4% of our series during elective surgery, although macroscopic alterations in the colon of some 23% have been described after stent insertion.24
In patients with elective surgery, a greater proportion of anastomosis, laparoscopic surgery and isolated nodes were found than in urgent surgery, while morbidity, mortality and hospital stay were lower. These results are consistent and, in many cases, are better than those from meta-analyses,5,12,16 where it is shown that the results of the stent placement as a bridge to elective surgery improve over those of urgent surgery.25
Regarding the oncological outcome, our study has shown statistically significant differences in the 3- and 5-year survival rates of these groups, with better results in the elective surgery group. However, there are experimental and retrospective series that attribute a greater risk of local and distant recurrence to the stent group as a bridge to surgery.26,27 Taking into account that the age and proportion of stage IV patients was higher in the group of emergency surgery patients, the surgical and oncological results may have been negatively influenced by this fact, as well as the high postoperative mortality obtained (13.6%).
In 70 patients who were candidates for palliative management, obstruction was resolved by stenting and no further surgery was proposed. The European Society of Gastrointestinal Endoscopy guidelines from 201428 recommend stenting over any other procedure in this type of patients, given the lower morbidity and better quality of life by avoiding stoma. In our series, the 40% mortality rate after 90 days in these patients makes the less invasive option preferable. The rate of late complications obtained in this group (migration, obstruction and perforation) was significantly lower than published reports4 despite having presented an average survival of more than 8 months, which is enough time for these complications to occur.
Although this is an extensive and systematized series, one limitation of the study is the ambispective nature, which could generate a selection bias in the retrospective field. In addition, in patients in whom the procedure could have been indicated, urgent surgery may have been performed for other reasons, such as the surgeon factor or the unavailability of the technique. The groups analyzed arise from the same cohort of patients, so the comparison between elective and urgent surgery may lack external validity.
With the results obtained and in line with the existing literature, we can confirm that the initial treatment of neoplastic obstruction of the left colon with stent in indicated cases is currently a technique with a high clinical success rate that avoids a large percentage of colostomies, which improves per se and as a “bridge therapy” the results obtained with urgent surgery. However, there is a significant proportion of patients with complications after the technique or failure that require urgent surgical intervention.
It is necessary to carry out new well-designed prospective studies that analyze long-term oncological results in detail in order to establish the best treatment option individually.
ConclusionThe treatment of neoplastic obstruction of the left colon with stents is an effective strategy to electively treat a significant number of patients, although failure or complications of the technique require urgent surgery in a significant percentage of cases.
The successful use of the technique as a bridge therapy reduces postoperative morbidity and mortality and improves quality of life by avoiding colostomy. Patients with technical or clinical failure of the procedure have worse clinical and oncological outcomes than those who underwent the procedure and had deferred surgery.
However, considering the overall context based on reports in the literature, clinical guidelines and our own clinical experience, there is currently not enough evidence today for standardized stent use over other therapeutic strategies, except for palliative patient care.
FundingThis study has received no specific funding from public, commercial or nonprofit organizations.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Genzor Ríos SJ, González-Nicolás Trébol MT, Aguirre Prat N, Cantalejo Díaz M, Rodríguez Artigas JM, Medrano Peña J, et al. Stent performance in obstructive left colon cancer. Unicentric and cross-sectional study. Cir Esp. 2019;97:397–404.