Brito et al.1 treated patients with supraclavicular lymph node involvement using multimodal therapy with curative intent (chemotherapy [CTx], surgery and radiotherapy). With this method, they obtained better results than in patients who presented distant disease that was not supraclavicular. These results led to the review and modifications of the American Joint Committee on Cancer (AJCC-TNM) classification. Since its sixth edition, metastases in the ipsilateral supraclavicular lymph nodes have ceased to be considered distant metastases (M1) and have been classified as locoregional disease (N3c).2,3 To this day, the debate continues and no consensus has been reached for the treatment of these patients.
Likewise, contralateral axillary involvement should be considered stage IV and therefore the treatment of these patients should be palliative.4 However, there is a hypothesis that dissemination to the contralateral axilla could occur by the lymphatic pathway, therefore locoregional curative treatment would be justified.5 Therefore, the management of this situation is not standardized and must be individualized for each patient.
We present a controversial clinical case using multimodal treatment, associating surgery of a metastatic breast carcinoma with contralateral and ipsilateral supraclavicular lymph nodes.
A 57-year-old woman presented with a 10cm ulcerated tumor infiltrating the skin and chest wall of the right breast. Mammography, magnetic resonance imaging with gadolinium contrast and core-needle biopsy diagnosed the mass as invasive ductal carcinoma (IDC) of the right breast with ipsilateral and contralateral axillary lymph node involvement (cT4c cN1c M1). Immunohistochemistry study reported: estrogen receptors (ER) +++, progesterone receptors (PR) +, cerbB2 ++ (positive FISH), Ki 67 20%.
After 8 cycles of CTx with docetaxel, trastuzumab and pertuzumab with good radiological response, radical mastectomy was performed with right and left axillary lymph node dissection. The pathology study of the piece reported an IDC lesion measuring 3.5×3cm (RE −, RP −, cerb B2 +++ and Ki 67 30%), grade 1, N + (1/14) and an invasive lobular carcinoma measuring 2×1.5cm (RE −, RP −, cerbB2 −, Ki 67 5%–10%). The axillary lymphadenectomy dissection revealed bilateral lymph node involvement: 1/14 in the right axilla and 4/24 in the left axilla.
The patient did not receive radiotherapy due to limited mobility of the right glenohumeral joint and followed adjuvant treatment with trastuzumab-pertuzumab every 21 days.
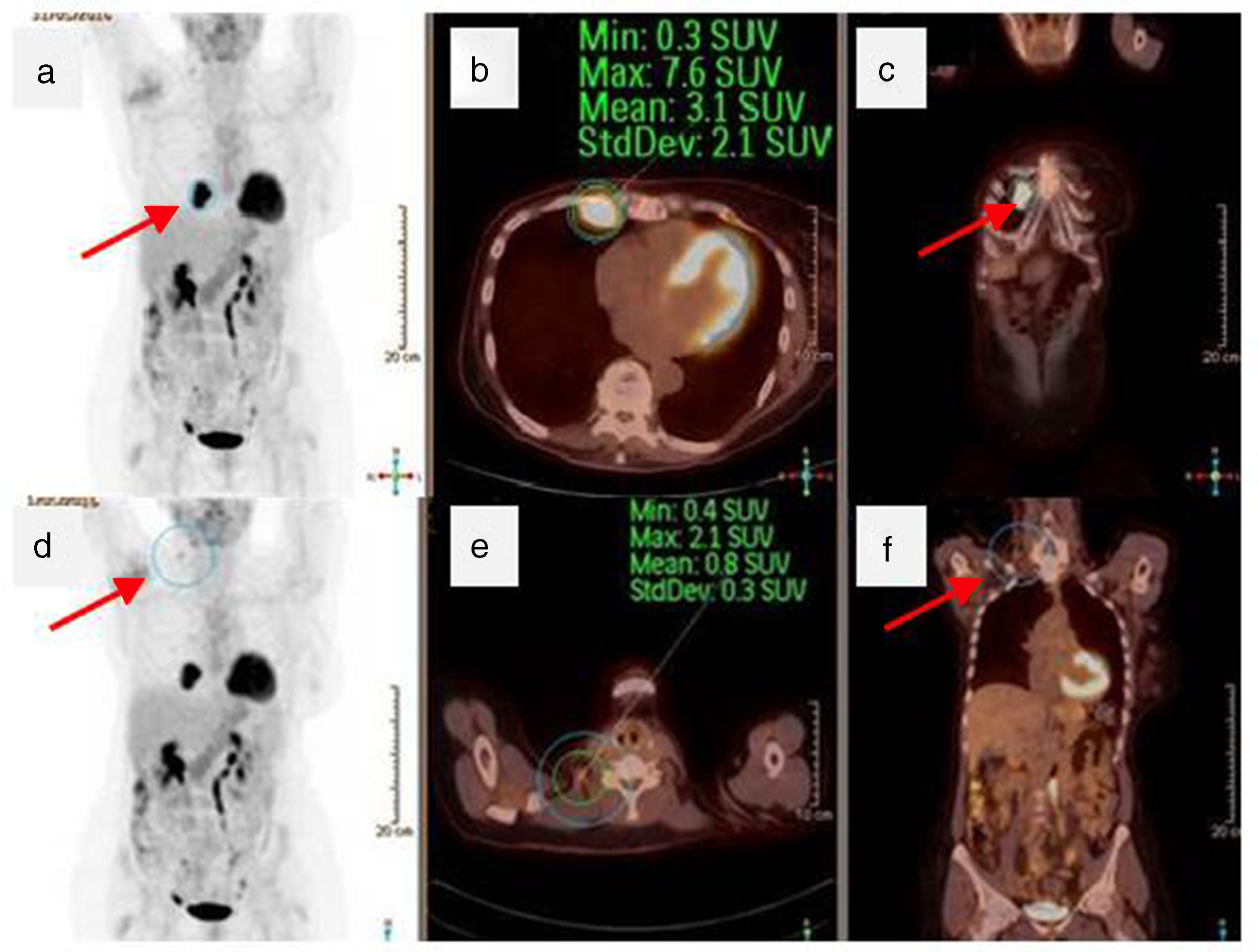
Positron emission tomography/computed tomography (PET/CT) one year after surgery (Fig. 1) detected right supraclavicular lymph node and internal mammary involvement, confirmed by fine-needle aspiration. The internal mammary ultrasound detected nodal involvement with a hypoechoic lesion measuring 4×3×4cm.
Total-body PET/CT: (a) coronal PET image showing hyperuptake of the internal breast (arrow); (b) axial PET/CT showing the same lesion (circle); (c) coronal PET/CT image with the lesion in white (arrow); (d) coronal PET view with hyperuptake in the right supraclavicular region; (e) axial PET/CT slice demonstrating the same involvement (circle); (f) coronal PET/CT showing right cervical hyperuptake in white (arrow).
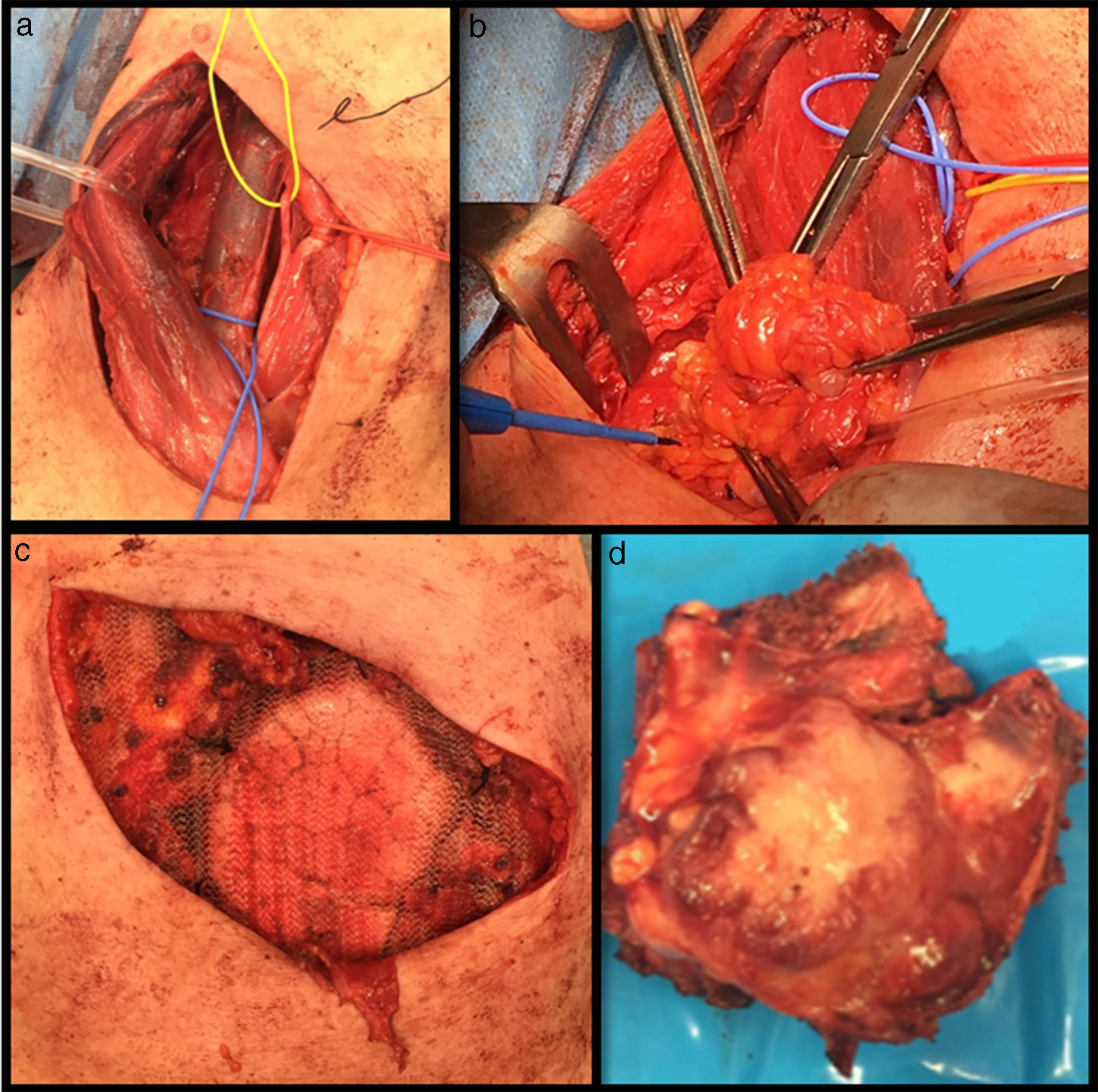
Three cycles of CTx were administered with TDM1 (trastuzumab emtansine) and subsequent PET/CT showed a decrease in size and right supraclavicular lymph node metabolism (SUV 2.1, previously 3.3), but increased internal mammary metabolism (SUV 7.6, previously 7) compared to the previous study. Surgical intervention was performed one month after the end of CTx, involving functional right lateral cervical dissection, excision of the internal mammary chain lesion and 5th, 6th and 7th anterior costal arches due to macroscopic involvement of the intercostal muscles. The wall defect was covered with a double-sided mesh (Fig. 2). The patient progressed favorably and was discharged on the 5th postoperative day.
The pathological anatomy of the internal mammary chain lesion revealed a metastasis measuring 5×1.6cm, with involvement of soft tissues (striated muscle and fibrous-fatty tissue) by lobular carcinoma, with no bone involvement, free resection margins and immunohistochemistry: RE −, RP −, cerbB2 −, Ki 67 5%–10%. From the cervical lymph node dissection, 52 lymphadenopathies were isolated with no tumor involvement. The patient currently continues with adjuvant CTx with TDM1 and is disease-free 9 months after the intervention.
There are numerous publications that evaluate the results of radiotherapy in the involvement of the internal and supraclavicular mammary arteries6,7; however, the role of surgery has not yet been studied.8 In the review of the literature, there is a study that included patients with recurrence of the disease at the supraclavicular level where surgery was part of the treatment and concluded that surgical excision of these supraclavicular lymph nodes would be a prognostic factor for overall survival.9
The negative pathology results of the lymph nodes removed in the cervical lymphadenectomy could be explained by a complete response to CTx that was already evident in the re-evaluation PET after the end of the last cycle, where there was a decrease in metabolic activity.
Although locoregional therapy is not standard in the treatment of de novo stage IV cancers, it is usually used as a palliative treatment.10 In this group of patients, this would be the case by including surgery in multimodal treatment for better control of the disease. There are authors who defend that patients with advanced tumor disease and certain cancer subtypes, such as luminal-like or Her2, can be offered local treatment with surgery or radiotherapy when this means better control of the primary tumor or the regional involvement in order to improve overall survival.10 In cases in which radiotherapy cannot be applied, as in our patient, surgery would be the option for better locoregional control of the disease.
Please cite this article as: de Andrés Gómez A, Villalba Ferrer F, Navarro Moratalla C, Guijarro Jorge R, Fuster Diana C. Tratamiento quirúrgico de la recidiva supraclavicular y a nivel de la mamaria interna por un carcinoma de mama. Cir Esp. 2018;96:241–244.