Several studies have evaluated the effect of liposuction or abdominoplasty on metabolic health, including insulin resistance, with mixed results. Many overweight patients, with no marked obesity, are recommended to undergo liposuction combined with abdominoplasty, but no study has evaluated the effectiveness of combining the two procedures on metabolic health.
MethodsThe present prospective cohort study compares the metabolic parameters of 2 groups of normoglycemic Hispanic women without obesity. The first group underwent liposuction only (LIPO), while the second group had combined liposuction and abdominoplasty (LIPO + ABDO).
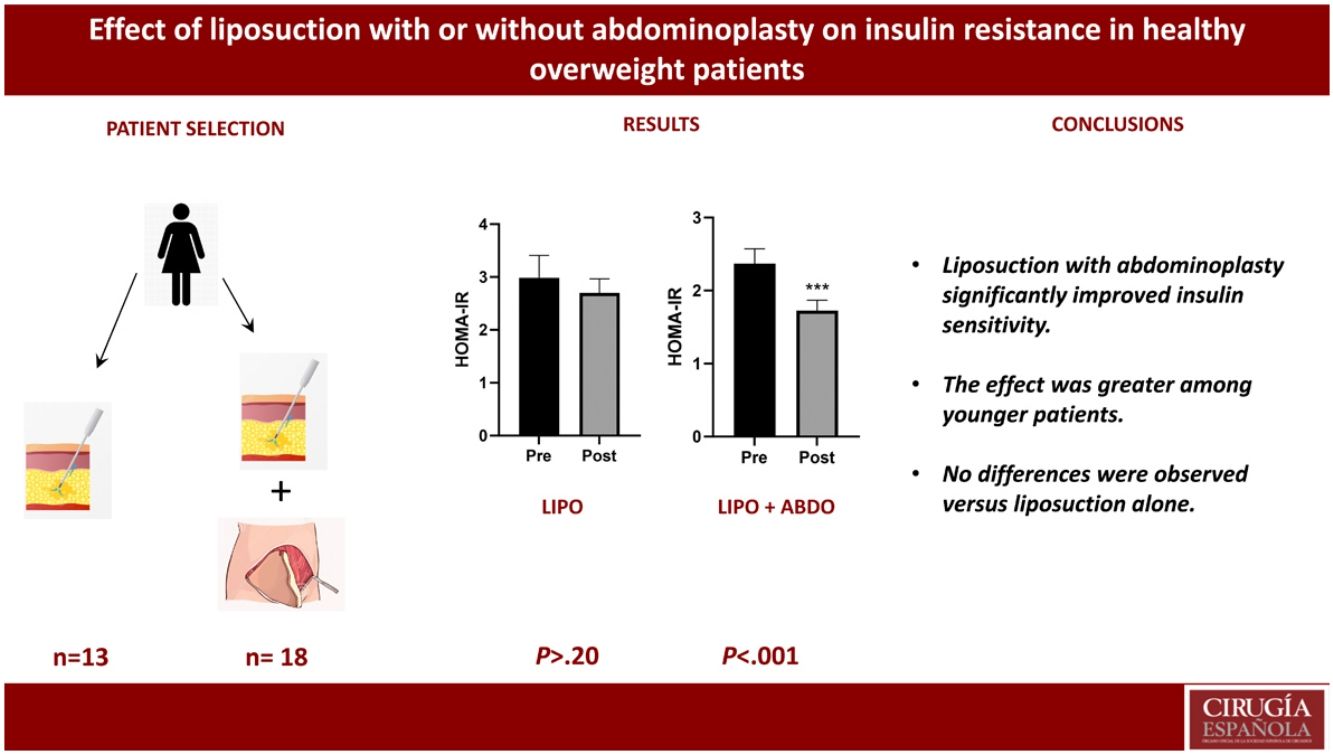
ResultsA total of 31 patients were evaluated, including 13 in the LIPO group and 18 in the LIPO + ABDO group. The 2 groups had similar HOMA-IR before surgery (P > 0.72). When tested 60 days after surgery, women in the LIPO group had similar HOMA-IR compared to their preoperative levels (2.98 ± 0.4 vs 2.70 ± 0.3; P > .20). However, the LIPO+ABDO group showed significantly reduced HOMA-IR values compared to their preoperative levels (2.37 ± 0.2 vs 1.73 ± 0.1; P < .001). In this group, this decrease also positively correlated with their preoperative HOMA-IR (Spearman r = 0.72; P < .001) and, interestingly, we observed a negative correlation between the age of the subjects and the drop in HOMA-IR after surgery (Spearman r = −0.56; P < .05). No changes were observed in the other biochemical parameters that were assessed.
ConclusionsThese data suggest that, when combined with abdominoplasty, liposuction does improve insulin resistance in healthy Hispanic females. More studies are warranted to address this possibility.
Varios estudios han evaluado el efecto de la liposucción o de la abdominoplastia sobre la salud metabólica, incluyendo la resistencia a la insulina, con resultados mixtos. A varias pacientes con sobrepeso, sin obesidad marcada se les recomienda el procedimiento de liposucción combinado con abdominoplastia sin que exista publicada evidencia alguna sobre la efectividad de combinar ambos procedimientos en la salud metabólica.
MétodosEl presente estudio prospectivo de cohorte evaluó el cambio en la resistencia a la insulina y otros parámetros metabólicos en dos grupos de mujeres hispanoamericanas normoglucémicas con sobrepeso. Las pacientes del primer grupo fueron sometidas a liposucción únicamente (LIPO), mientras que el segundo grupo fue sometido a liposucción con abdominoplastia (LIPO + ABDO).
ResultadosUn total de 31 pacientes fueron evaluadas, incluyendo a 13 con LIPO y 18 con LIPO + ABDO; ambos grupos mostraron HOMA-IRs prequirúrgicos similares (P > .72). En las del grupo LIPO evaluadas 60 días después del procedimiento, se observaron HOMA-IRs similares a sus niveles prequirúrgicos (2.98 ± 0.4 vs. 2.70 ± 0.3, P > .20); las del grupo LIPO + ABDO, sin embargo, mostraron HOMA-IR significativamente reducidos a comparación de sus índices prequirúrgicos (2.37 ± 0.2 vs. 1.73 ± 0.1, P < .001). También en este grupo, esta reducción se correlacionó positivamente con el valor prequirúrgico de HOMA-IR (P < .001) y, de manera interesante, se observó una correlación negativa entre la edad de la paciente y el grado de disminución en el HOMA-IR tras la cirugía (Spearman r = −0.56, P < .05). No se observaron cambios en los otros parámetros bioquímicos evaluados.
ConclusionesLos datos de este estudio sugieren que cuando es combinada con abdominoplastia, la liposucción mejora la resistencia a la insulina en pacientes hispanoamericanas. Se requieren de estudios adicionales para probar dicha posibilidad.
For several years now, being overweight or obese is one of the most common preventable risk factors for the appearance of a multitude of diseases around the world. In 2016, 1.9 billion adults were overweight, 650 million of which were obese.1 Obesity can be defined as excessive and chronic accumulation of adipose tissue as a result of long-term energy imbalance, in which caloric intake exceeds energy expenditure.2 Dysfunctions in the physiology of adipose tissue have been observed in patients with obesity, which have also been related to a higher risk of developing metabolic and/or cardiovascular complications in these patients.3 Specifically, a correlation has been clearly established between the percentage of adipose mass and insulin resistance.4 Even in patients with a normal body mass index (BMI), the percentage of body fat has been shown to correlate with insulin resistance.5 Likewise, in patients treated with bariatric surgery, body fat percentage has been identified as a determining factor in insulin resistance, regardless of BMI.6
Liposuction and abdominoplasty are procedures whose direct objective is to reduce the mass of this tissue.7 The effect of direct reduction of adipose tissue using liposuction (with or without abdominoplasty) on insulin sensitivity has been evaluated on several occasions; however, the results have been mixed, and some studies have found significant improvement with the procedure, while others have reported no effect.8 According to another meta-analysis analyzing the effect of large-volume liposuction on insulin sensitivity in patients with obesity, one limitation of previous studies has been the failure to systematically compare the effect of liposuction versus abdominoplasty or liposuction with abdominoplasty.9 Another limitation is that the patients included in these studies already had different degrees of obesity, possibly with associated comorbidities. The volumes extracted also varied considerably depending on the patient, the surgeon and even current regulations.10 Consequently, a considerable number of the subjects studied continued to have high levels of adipose mass, and many individuals with obesity present alterations in the homeostasis of adipose tissue,11 which may further hinder possible improvements in metabolic health after the surgical procedure. Furthermore, little is known about the metabolic effect of surgical fat extraction in apparently healthy, although overweight, patients.
Our study demonstrates the resulting effects of liposuction with or without abdominoplasty (LIPO or LIPO + ABDO) on different metabolic parameters, including insulin sensitivity, in a group of normoglycemic, overweight patients who underwent these procedures.
MethodsPatient characteristicsWe designed a prospective, single-center observational cohort study at a hospital in Mexico City, selecting apparently healthy female patients who underwent a complete pre-surgical protocol before either liposuction (LIPO) or liposuction and abdominoplasty (LIPO + ABDO), as appropriate, following the evaluation criteria of the Matarasso scale.12 According to this scale, patients who were classified as type I or II underwent liposuction, whereas those who were classified as type III or IV underwent abdominoplasty with liposuction. The inclusion criteria were: normotensive and normoglycemic female patients, BMI ≤ 30 kg/m2, laboratory work-up results within normal parameters, and no medical history of chronic or degenerative disease. During postoperative follow-up, there was no evidence of infection or dehiscence, and stitches were removed after an average of 15 days.
Metabolic parameters evaluatedIn both groups of patients, we collected data for BMI, waist-hip ratio (WHR), as well as both preoperative and 60-day post-op serum levels of glucose, insulin, cholesterol and triglycerides (Table 1). Preoperative and postoperative HOMA-IR values were calculated for each patient. The HOMA-IR (homeostatic model assessment for insulin resistance) consists of a mathematical model that evaluates insulin resistance using 2 simple laboratory parameters: fasting glucose and insulin. It assesses whether there is a peripheral “blockade” or resistance to the action of insulin, indirectly evaluating the function of the pancreatic beta cells.13
Preoperative patient parameters (mean ± SD) and P of the difference between both groups. BMI: body mass index (kg/m2); WHR: waist-to-hip ratio; HOMA-IR: homeostatic model assessment for insulin resistance.
| Parameter | LIPO (N = 13) | LIPO + ABDO (N = 18) | P |
|---|---|---|---|
| Age | 34.38 ± 3.6 | 38.28 ± 2.0 | .0757 |
| Weight (kg) | 64.5 ± 1.9 | 71.14 ± 1.9 | .0246 |
| BMI (kg/m2) | 25.01 ± 0.3 | 26.77 ± 0.6 | .0403 |
| ICC | 0.89 ± 0.02 | 0.85 ± 0.02 | .0869 |
| LIPO volume (mL) | 2185 ± 127 | 1811 ± 119 | .1055 |
| Flap weight (g) | NA | 997 ± 122 | NA |
| Fasting glucose (mg/dL) | 86 ± 5 | 86 ± 7 | .9855 |
| Fasting insulin (mU/mL) | 13.98 ± 1.9 | 11.2 ± 1 | .5868 |
| HOMA-IR | 2.98 ± 0.4 | 2.37 ± 0.2 | .7298 |
| Triglycerides (mg/dL) | 181 ± 10 | 142 ± 14 | .614 |
| Cholesterol (mg/dL) | 212 ± 5 | 195 ± 7 | .1495 |
| Uric acid (mg/dL) | 4.14 ± 0.1 | 4.24 ± 0.1 | .5738 |
The anthropometric and laboratory data of each group were evaluated with the Shapiro-Wilk normality test. The comparison between groups of preoperative versus postoperative data that met with normal distribution was performed using a paired t-test; otherwise, the Wilcoxon sign test was used. Comparisons of baseline values between the LIPO and LIPO + ABDO groups were performed using unpaired t-tests or Mann-Whitney tests. Post hoc correlational analyses of the difference pre- versus postoperative HOMA-IR index versus different parameters measured in patients before surgery using the Spearman test. In all cases, a P value <.05 was considered a significant difference.
ResultsA total of 31 female patients were included in the present study and divided into 2 groups. The LIPO group included 13 patients (mean age 32 [26–39] years; preoperative BMI 25.1 ± 0.3 kg/m2) who underwent liposuction. The LIPO + ABDO group consisted of 18 patients with a median age of 36 (32–47) years and preoperative BMI of 26.77 ± 0.6 kg/m2 who underwent liposuction with abdominoplasty. The preoperative BMI of the second group was slightly higher (P < .05) than the first, while both groups were similar in terms of age and all biochemical parameters measured (Table 1). When measured 60 days after surgery, BMI and WHR had decreased significantly in both groups compared to preoperative values (Fig. 1). Afterwards, the lipid profiles were evaluated, yet we observed no significant changes in cholesterol or triglyceride levels (Fig. 2). When fasting glucose levels were analyzed, however, we noted a slight decrease in the LIPO group but not in the LIPO + ABDO group (Fig. 3A-B). Basal insulin remained similar in the LIPO group, while it decreased significantly in the LIPO + ABDO group (t(17) = 4.55, P < .001; Fig. 3C-D).
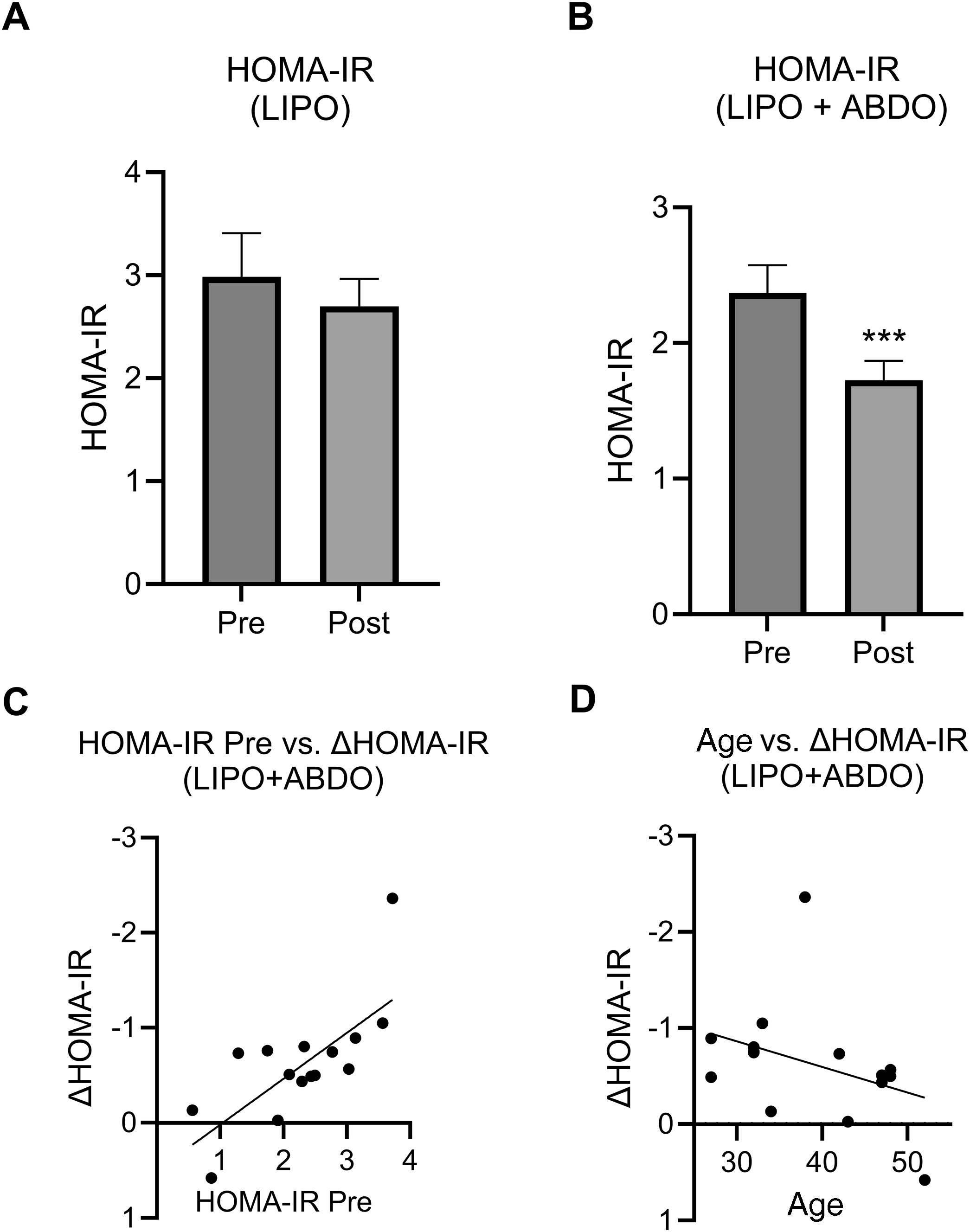
Lastly, changes in insulin resistance were evaluated with the HOMA-IR, which showed that the preoperative values were similar between the 2 groups (2.17 [1.96–3.61] vs 2.47 [1.87–3.06]) for LIPO and LIPO + ABDO, respectively; Mann-Whitney U = 108, P > .72; Table 1). In patients in the LIPO group, insulin resistance levels were similar 60 days after the procedure compared to their preoperative levels (2.17 [1.96–3.61] vs 2.33 [2.08–3.36] for pre-op and post-op HOMA-IR, respectively; P > .20) (Fig. 4A), which suggests that liposuction did not improve insulin sensitivity in these patients. However, this same analysis performed in patients in the LIPO + ABDO group showed a clear improvement (2.37 ± 0.2 vs 1.73 ± 0.1 for the pre-op and post-op HOMA-IR, respectively; P < .001) (Fig. 4B). Subsequently, in this group of patients, Spearman correlation tests were performed between the improvement in the HOMA-IR and the different anthropometric and laboratory parameters that were measured, finding that said improvement strongly correlated with preoperative HOMA-IR (Spearman r = 0.72; P < .001) (Fig. 4C). Also interestingly, the degree of improvement in the HOMA-IR was inversely related to the age of the patient (Spearman r = −0.56; P < .05) (Fig. 4D), suggesting that younger patients who underwent the LIPO + ABDO procedure experienced greater improvements in insulin sensitivity.
Insulin resistance before surgery and 60 days after surgery expressed with the HOMA-IR value in the LIPO (A) and LIPO + ABDO (B) groups; C) Correlation between the postoperative drop in HOMA-IR of patients in the LIPO + ABDO group and their preoperative HOMA-IR; D) Correlation between patient age of the LIPO + ABDO group and the drop in their HOMA-IR after surgery.
This study has evaluated different metabolic parameters in women who had undergone either liposuction alone (LIPO) or liposuction with abdominoplasty (LIPO + ABDO), both before surgery and 60 days later. Prior to the procedure, all patients were apparently healthy, normotensive, and slightly to moderately overweight. Their fasting glucose and insulin levels were within normal parameters, and their lipid profiles showed values at the upper limit. When evaluated 2 months after surgery, no improvement was observed in cholesterol levels or triglyceride levels. These data agree with the results of a recent meta-analysis of the effect of surgical fat removal on different metabolic parameters.14 Regarding the glycemic profile, however, the results presented herein show that LIPO + ABDO significantly improves insulin sensitivity, evaluated with the HOMA-IR after 60 days; no differences were observed in the LIPO group. Furthermore, in the patients in the LIPO + ABDO group, a moderate correlation was observed between the age of the patients and the pre versus post difference in the HOMA-IR index, suggesting that the younger the patients were, the greater their insulin sensitivity after the procedure.
A recent meta-analysis analyzed the effect of surgical fat removal on the metabolic profile, by either liposuction or abdominoplasty. This study evaluated different markers, including proinflammatory cytokines, adiponectin and triglycerides, in addition to insulin sensitivity. Interestingly, the authors found that only fasting insulin and HOMA-IR improved significantly.14 However, the studies included in the analysis that found significant improvement were mainly limited to those evaluating insulin sensitivity after the removal of large amounts of fat in obese women15–17 or in male patients,18 whereas the studies in overweight Hispanic women showed little or no improvement.19–21 Similarly, another study in Mexican patients who underwent surgical fat removal by abdominoplasty without liposuction reported no improvement in insulin sensitivity measured 40–50 days after the procedure, although leptin concentrations decreased.22
In the present case, although no significant difference was observed between the HOMA-IR of the 2 patient groups, a significant limitation to this observation is that, unlike the patients in the LIPO + ABDO group, the LIPO group had a mean preoperative HOMA-IR above 2.9, indicating significant insulin resistance.23 It is possible that this fact could have reduced their ability to improve with surgery, regardless of the group. However, the fact that a strong correlation was found between the preoperative HOMA-IR value and the postoperative improvement in the LIPO + ABDO group (Fig. 1C) contradicts this possibility. Another important limitation, which is inherent to the design, is that the study includes patients from a single hospital and was not randomized (use of the Matarasso scale for group assignment). Indeed, the ability to perform abdominoplasty was determined by the presence of excess skin and/or skin laxity, which is not present in Matarasso grades I and II. The presence of excess skin, in addition to the accumulation of abdominal fat, is a frequent consequence of pregnancy or significant weight loss. Abdominoplasty is a low-risk surgical procedure that could entail possible metabolic benefits in these patients along with the aesthetic and psychosocial results, especially when accompanied by an exercise program and lifestyle changes.24,25 To confirm this possibility, further multicenter studies are required with a greater number and diversity of patients.
In conclusion, the data presented herein suggest that combining abdominoplasty with liposuction, which is considered a low-risk surgery when performed correctly,26 could have an additional benefit in improving the metabolic health of patients, especially if they are relatively young. More powerful multicenter studies with larger patient populations are required to evaluate this possibility.
Conflicts of interestThe authors declare that this article was prepared in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
ThanksThis study received partial funding from the Support Program for Research and Technological Innovation Projects (PAPIIT) of the General Directorate of Academic Personnel Affairs, UNAM (no. IN227123) awarded to JPM.