Pancreaticoduodenectomy (PD) is a very complex operation. Its development took place very slowly at the most prestigious centers in the world. The aim of this investigation is to know who were the first surgeons to perform a PD in Spain as well as its historical circumstances. Despite all kinds of difficulties and very few resources, the first PD in Spain were carried out in Barcelona at the Hospital de la Santa Creu i Sant Pau where from the mid-50s a school of gastrointestinal surgery emerged with surgeons soon to become the spearhead of the Spanish surgery and a reference for the whole country: Pi-Figueras, Vicente Artigas, Antonio Soler-Roig and Antonio Llauradó. Almost simultaneously, in Oviedo, Luis Estrada also introduced the PD and total pancreaticoduodenectomy after a period of training with the pioneers of pancreatic surgery in the United States.
La duodenopancreatectomía cefálica (DPC) es una intervención quirúrgica muy compleja cuyo desarrollo tuvo lugar de forma muy lenta y en los centros de mayor prestigio del mundo. El objetivo de esta investigación es conocer quiénes fueron los cirujanos que realizaron las primeras DPC en España y las circunstancias en que se realizaron. En un contexto histórico caracterizado por la gran escasez de medios técnicos y económicos, como era España en los años 50 del siglo xx, las primeras DPC se llevan a cabo en Barcelona, en el Hospital de la Santa Creu i Sant Pau, donde se desarrolló una escuela de cirugía gastrointestinal liderada por cirujanos que se convirtieron en la punta de lanza de la cirugía española y referencias nacionales como fueron Pi-Figueras, Vicente Artigas, Soler-Roig y Antonio Llauradó. Casi de forma simultánea, en Oviedo, Luis Estrada introdujo también la DPC y la duodenopancreatectomía total tras un periodo de formación con los pioneros de la cirugía pancreática en Estados Unidos.
Pancreaticoduodenectomy (PD) is the treatment of choice for tumors of the head of the pancreas and periampullary tumors. Although today this surgery is habitually performed in specialized units at many Spanish hospitals,1 its development was extraordinarily slow and it was initially only conducted at the most highly prestigious and best equipped hospitals in the world.2,3
Historical circumstances in our country have meant that the initial development of PD has been marked by an enormous lack of resources and all sorts of difficulties. Even so, several surgeons were able to successfully conduct the first PD in Spain, which became the foundation for the later development of oncological pancreatic surgery. To date, there have been no studies that identify and recognize who these PD pioneers were and how they were able to overcome the numerous obstacles encountered.
The objective of this study was to determine which surgeons were those who carried out the first PD in Spain and the circumstances involved.
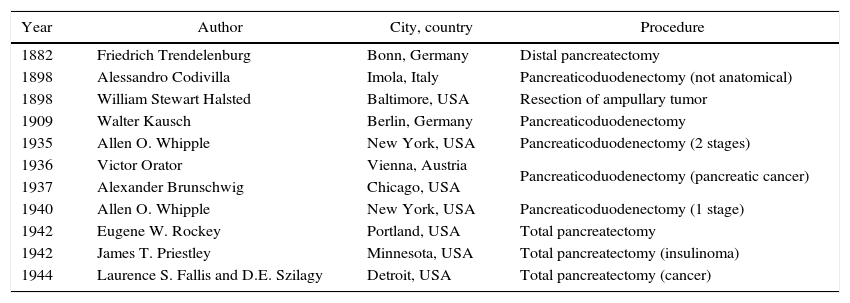
International HistoryBetween the first distal resection by Friedrich Trendelenburg in 1882 and the publication by A. Whipple in 1935, much progress was made in the surgical approach to pancreatic diseases.4,5 Historical events were the first pancreaticoduodenectomy by Alessandro Codivilla in Imola and the first resection of an ampulloma by William Stewart Halsted in Baltimore, both in 1898, or the first pancreatoduodenectomy with survival, by Walther Kausch in Berlin in 1909.6 Although most of these experiences were single cases, and many patients died before being discharged from the hospital, they provided a series of useful technical resources for the much more frequent bile duct interventions.4 In fact, the most common surgical technique in patients with obstructive tumors of the bile duct was bypass: cholecystojejunostomy or cholecystogastrostomy, and later choledochoduodenostomy or a defunctionalized loop in Y.5
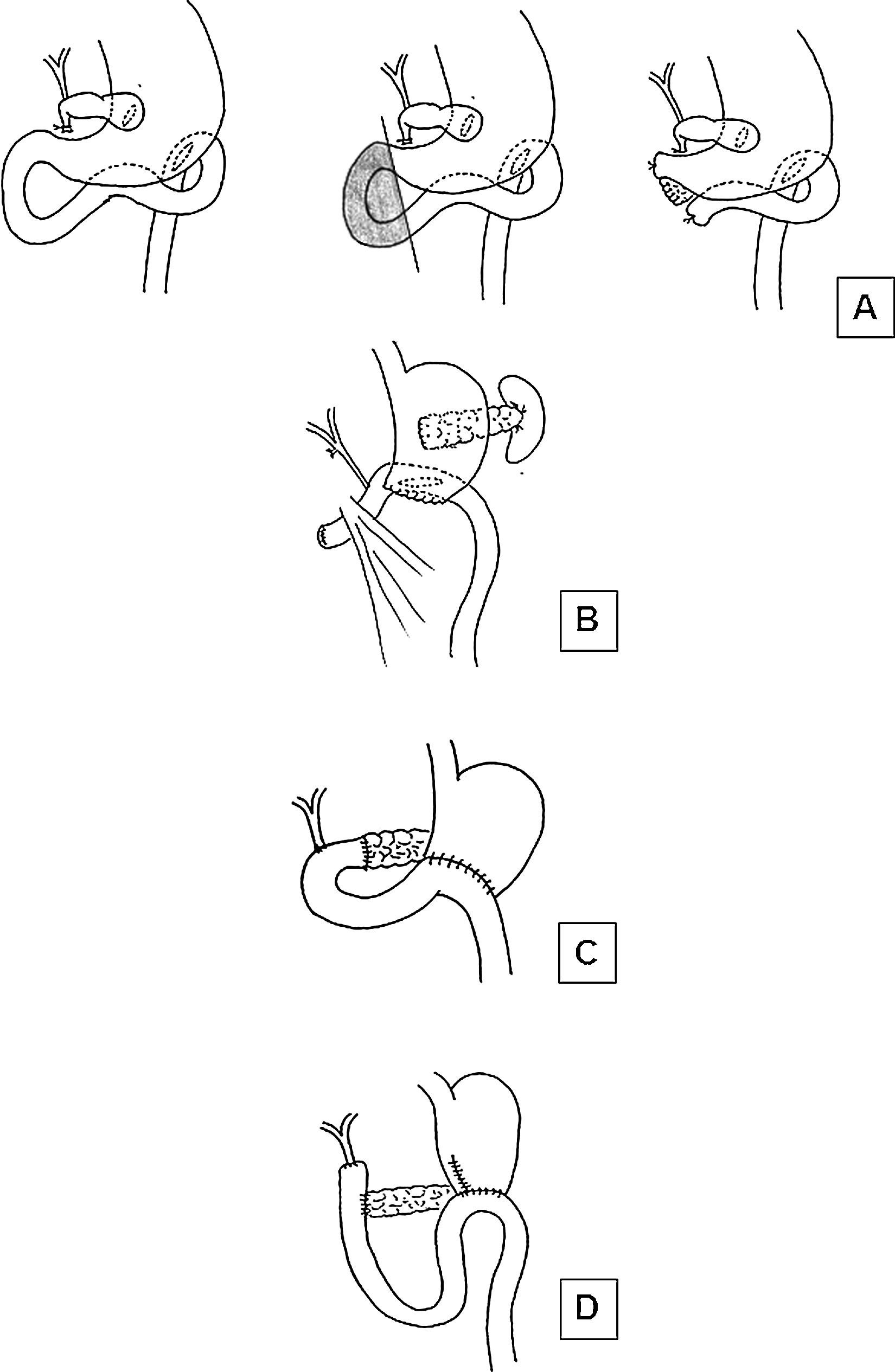
In order to advance from simple bypass to resection, numerous obstacles had to be overcome. The first was that pancreatic juices were considered essential or life. The second was the precarious general state of the patients due to obstructive biliary syndrome, as patients were intensely jaundiced, malnourished and had severe hemorrhagic diathesis. The proposals by Whipple were able to overcome some of these problems. That of pancreatic secretion was resolved by ligating the Wirsung duct and suturing the stump of the pancreatic remnant, as he intuited that the pancreatic juices were not necessary for life. Obstructive biliary syndrome was resolved by performing the surgery in 2 phases: first, cholecystogastric diversion and gastroenterostomy and, once the patient recovered and presented no jaundice and a better nutritional state, PD was completed2 (Fig. 1A). Therefore, the importance of Whipple is not based on the fact that he was the first to conduct a PD (which he was not); instead, he was able to unite the knowledge accumulated in previous decades, apply it and present his findings to the scientific community so that they were feasible for other surgeons. Since then, new cases have been were slowly added, in spite of the high morbidity entailed, and multiple modifications were made to the technique.5 In March 1940, Whipple performed his first case of radical removal of the head of the pancreas and duodenum in one operation. In the corresponding publication,7 Whipple definitively proposed conducting the entire procedure in one single operation, after previously preparing the patient with vitamin K (discovered by Henrik Dam in 1929, but not available in clinical practice until 19398–10), with the anastomosis of the pancreatic duct to the jejunal loop. Shortly before, Viktor Orator in 1936 and Alexander Brunschwig in 1937 performed the first PD in 2 parts due to pancreatic cancer.11–13 Afterwards, in 1942 Eugene Rockey14 completed the first total pancreaticoduodenectomy, who was followed by Priestley15 in an insulinoma with postoperative survival and by Fallis and Szilagyi16 in 1944 in an adenocarcinoma5 (Table 1).
Surgical diagram showing different reconstruction techniques after PD: (A) Original Whipple technique in 2 stages; (B) Reconstruction by Leopoldo Domínguez from the first description of a PD in Spain; (C) Technique used by Pi-Figueras and Vicens Artigas; (D) Technique most frequently used by Luis Estrada.
Historic Events in Pancreatic Surgery.
| Year | Author | City, country | Procedure |
|---|---|---|---|
| 1882 | Friedrich Trendelenburg | Bonn, Germany | Distal pancreatectomy |
| 1898 | Alessandro Codivilla | Imola, Italy | Pancreaticoduodenectomy (not anatomical) |
| 1898 | William Stewart Halsted | Baltimore, USA | Resection of ampullary tumor |
| 1909 | Walter Kausch | Berlin, Germany | Pancreaticoduodenectomy |
| 1935 | Allen O. Whipple | New York, USA | Pancreaticoduodenectomy (2 stages) |
| 1936 | Victor Orator | Vienna, Austria | Pancreaticoduodenectomy (pancreatic cancer) |
| 1937 | Alexander Brunschwig | Chicago, USA | |
| 1940 | Allen O. Whipple | New York, USA | Pancreaticoduodenectomy (1 stage) |
| 1942 | Eugene W. Rockey | Portland, USA | Total pancreatectomy |
| 1942 | James T. Priestley | Minnesota, USA | Total pancreatectomy (insulinoma) |
| 1944 | Laurence S. Fallis and D.E. Szilagy | Detroit, USA | Total pancreatectomy (cancer) |
In Spain, the first reference to the removal of a pancreatic tumor, a fibroma in the tail of the pancreas, was by Salvador Cardenal in 1907.17 There is also evidence of cysts and pseudocysts treated surgically, whose treatment “[…] of choice […] is marsupialization” as indicated in the book by Luis Urrutia Enfermedades del hígado y del pancreas from 1923.18 As for the treatment of tumors of the pancreas and the papilla of Vater, the same author reviewed the cases of the international literature (none in Spain), which provided discouraging outcomes, and concluded that “the most radical yet safe procedure seems to be resection of the mid portion of the duodenum together with the outlet of the common bile duct and the Wirsung duct; […] the intervention is, unfortunately, too large and complicated […]. Therefore, surgeons with greater experience in the biliary tract use cystogastrostomy or cholecystoenterostomy in these cases.”18
It was not until the mid-1940s when there began to be indirect reports of pancreatectomies conducted to treat malignant tumors, although these led to fatal outcomes. For example, the following paragraph from the Medical Pathology lessons of Dr. Jiménez Díaz19 in 1948: “[…] I had a patient […] and the radiology study detected a cancerous mass in the head of the pancreas; […] surgery was indicated […]. The operation, conducted by an expert surgeon, involved the excision of the tumor, which the patient initially tolerated very well the first few days, although later succumbed […]”.
It is at the beginning of the 1950s when we identify the first publication of a PD in our country, which also ended in death of the patient. It was performed in January 1951 by Leopoldo Domínguez Navarro at the Hospital Militar Gómez Ulla in Madrid in a 22-year-old patient with a pancreatic tumor that was identified as a lymphosarcoma. The published report20 provides a description of the surgeon's decision and determination: “[…] faced with formations that were undoubtedly cancerous in appearance […], we decided to carry out the only intervention that could be radical […], pancreatectomy of the head and half of the body, and […] pyloro-duodenectomy, re-establishing the continuities with a gastroenterostomy on the one hand and choledocho-jejunostomy […]”. In the description of the surgery, no reference is made to the management of the remaining pancreas, although the accompanying illustration shows a ligature en masse, with no anastomosis of the bowel (Fig. 1B). It does include, however, a surprising “duration of the operation of 2hours and 20 minutes”. It is precisely this decade, which began with the publication of this first report, that would witness the initial development of PD and pancreatic surgery with a modern feeling in our country, based on 2 foci within Spain and under very different circumstances: in Barcelona, in the heart of the prestigious Surgery Departments at the Hospital de la Santa Creu i Sant Pau and the School of Digestive Pathologies, and in Oviedo under a magnificently talented and versatile surgeon, Dr. Luis Estrada.
The Surgery Departments at the Hospital de la Santa Creu i Sant Pau and the School of Digestive PathologiesIn Spain, the tradition of surgery in Catalonia is well known, and one of its cornerstones was Salvador Cardenal (1852–1927), whose work was continued by a series of disciples, including Antonio Raventós Aviñó, Enrique Ribas Ribas or Manuel Corachán, to name a few. In 1930, when the Hospital de la Santa Creu was transferred from its previous site to its modernist facilities, 3 well-organized surgery departments were created,21 which, after the Spanish Civil War, were directed by Dr. Soler-Roig, Dr. Joan Puig-Sureda and Dr. Joan Prim Rosell. Working with them were a series of disciples who would quickly become the next generation of masters of Catalonian and Spanish surgery during the following decades: Jaume Pi-Figueras, Antoni Llauradó, Vicens Artigas Riera, Antoni Sitges Creus, Lino Torre, etc. In 1950, Puig-Sureda became head of the Digestive Surgery Division of the School of Digestive Pathologies under Dr. Gallart Monés, also located at the Hospital de la Santa Creu i San Pau, and Pi-Figueras took over his position at the General Surgery Department.21,22 They all performed the same operations, although with subtle differences, and were especially interested and had much experience in biliary tract surgery. Soler-Roig was one of the pioneers of preoperative cholangiography and transduodenal papillotomy, Antoni Llauradó was one of the first to conduct hepaticojejunostomies and performed more than 1000 papillotomies, and Pi-Figueras was the forefather of choledochoduodenostomy in Spain.23 His important activity as an educator is observed in the yearly surgery course initiated by Soler-Roig in 1950, which would later be continued by Puig la Calle, with the unification of the departments in 1972. It was precisely in this more advanced surgical setting where the first PD were conducted: the “Sant Pau school” in Barcelona was a historical crusader of capital importance for the development of biliopancreatic surgery in our country.
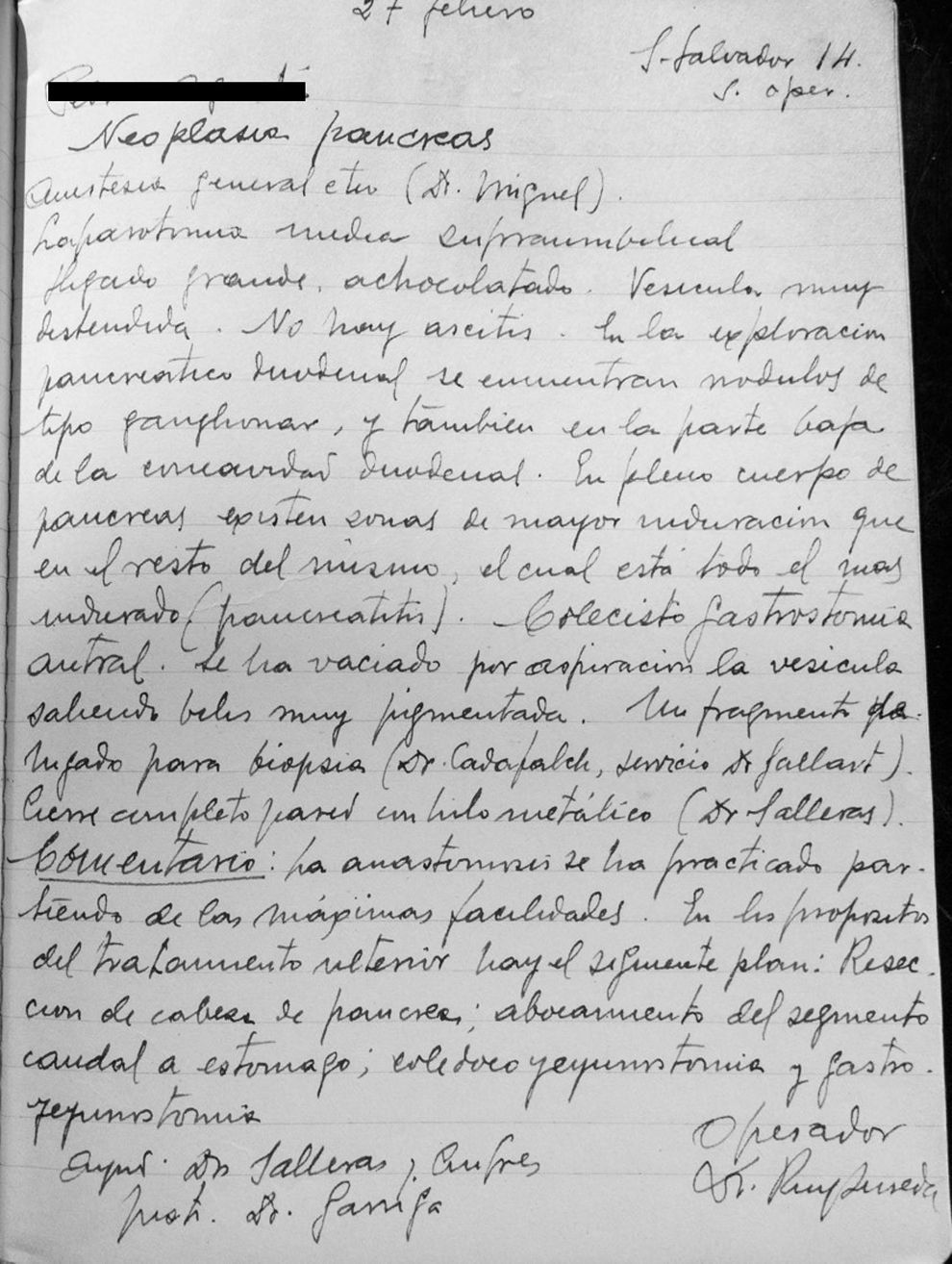
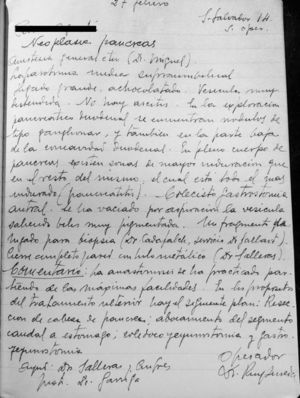
The analysis of the operative reports from the era preserved in the historical archives at the Hospital de la Santa Creu i Sant Pau shows how, stating in February 1946, Puig-Sureda and Llauradó attempted to conduct PD on at least 10 occasions (Fig. 2). However, they were only able to complete the procedure in 2 cases, both resulting in the immediate death of the patient. Furthermore, in the “Clinical lessons in Digestive Pathologies” by Gallart-Esquerdo,24 we have identified the following case of neoplastic obstruction of the bile duct: “First intervention (Soler-Roig; 12 January 1952): [Given the extremely grave nature…] we decided against excessive exploratory maneuvers, but there seems to be a tumor in the papilla of Vater […], causing obstruction […], cholecystostomy alone was performed […]”. The patient survived the intervention and afterwards “[the patient] was properly prepared to attempt excision of the supposed papillary tumor”, proceeding with the “second surgical intervention” (Soler-Roig; 9 February 1952): we decided to perform the radical operation (pancreaticoduodenectomy), followed by the following anastomoses: end-to-side hepaticojejunal, end-to-side pancreaticojejunal, end-to-side gastrojejunal and end-to-end jejunojejunal. After 4 days, in which the general state was relatively satisfactory […] the patient started to decline […] ascites […] [and died 50 days later after progressive decline in his condition]”.
Surgical report from 27 February 1946; surgeon Dr. Puig-Sureda: “General anesthesia with ether (Dr. Miguel). Supraumbilical midline laparotomy. Large, chocolate-colored liver. Very distended gallbladder. No ascites. Upon exploration of the pancreas and duodenum, lymph node-type nodules are found, and also at the lower part of the duodenal concavity. In the body of the pancreas, there are areas with greater induration than the surrounding tissue, and there are signs of pancreatitis throughout. Cholecystogastrostomy. The gallbladder has been emptied with suction, producing very dark bile. One liver fragment is taken for biopsy (Dr. Cadafalch, Dr. Gallart's department). Complete closure of the wall with metallic thread (Dr. Salleras).
Comments. The anastomosis was carried out as simply as possible. Proposed further treatment includes the following plan: resection of the head of the pancreas; anastomosis of the caudal segment to the stomach; choledocho-jejunostomy and gastrojejunostomy.”.
In 1953, at the first presentation of the 3rd National Surgery Conference III in Granada, titled “Surgical aspects of biliary stasis”, Pi-Figueras, Artigas and Llauradó provided their statistics from 28 cases of head of the pancreas neoplasms treated with different techniques, including 2 PD, which had both resulted in immediate death.25 As a counterpoint, Dr. Abilio García Barón from the Hospital Marqués de Valdecilla in Santander contributed 2 cases, both of which had also resulted in immediate death: “[…] radical excision (which we had used 2 times, with immediate failure) […]”.
The first publication of a PD with postoperative survival was in 1954, by Pi-Figueras, Artigas and Esterlich at the 7th Spanish Conference on Digestive and Nutritional Pathologies in Santiago de Compostela.26 Performed in 2 operations, the first being cholecystostomy and the second a resection 15 days later, it was necessary, due to “adherence of the portal vein to the neoplasm”, to ligate and divide this vessel; reconstruction involved “end-to-end pancreatojejunostomy, end-to-side choledocho-jejunostomy and Polya-Hoffmeister-Finsterer gastrojejunostomy […]”. At the 3-month follow-up visit, the patient “[…] has initiated portal hypertension syndrome, with the appearance of ascites”, which was most likely secondary to the portal ligation and which led to the death of the patient shortly thereafter.27 That same year, Vicente Artigas published an excellent review about the “Current state of pancreatic cancer surgery” in the Annals of the Hospital de la Santa Cruz y San Pablo.28 It is a study that already proposed the procedure in one single operation and, exceptionally, preoperative external biliary bypass, as well as pancreaticojejunal and choledochojejunal anastomoses (Fig. 1C). Nonetheless, in spite of the conceptual and theoretical advances, the clinical results continued to be disheartening, which motivated opinions, such as that of Gallart Esquerdo (at that time director of the School of Digestive Pathology): “It is not enough that PD is technically feasible. An operation that causes such elevated mortality should only be recommended when we believe that it must provide the patient with a worthwhile survival, and to date the results obtained by the most skilled surgeons are very disheartening.”29 Or, the opinion of another important surgeon and expert in bile tract surgery, Dr. José Clavero Margati, from a review article in 1956 about the surgical treatment of primitive tumors of the biliary tract30: Tumors of the papilla are susceptible to an intervention […]: papillectomy and papilloduodenectomy, which sometimes provide survivals of 3 or more years […]. Although pancreaticoduodenal procedures have already been practiced […] this surgery is still within the study and experimentation period […]”. This gave rise to the intense debate that continued until well passed the 1970s of recommending only palliative diversion with low mortality versus the resections with curative intent, but associated with greater mortality.31,32 Opinions that contrast with the illustrious and balanced vision of Dr. Artigas in 1956–1957: “The therapeutic problem of pancreatic cancer is a diagnostic problem today and not a problem of surgical technique. […]. In cases where there is no formal contraindication […] to excision, it should be performed, even knowing […] that it is necessary […] for it to be done in an earlier, more localized phase of the neoplasm (in the pancreas) to obtain better results […] but it is expected that, within a few years, the results […] will be more promising and will better reflect its possibilities27 […]. Limiting treatment with palliative surgery means definitively condemning the patient to the inexorable course of the condition, even when we have the means to avoid this outcome.”33 In our opinion, it is precisely this author who took a giant step in Spanish pancreatology, with the publication in 1956 of his Surgical pathology of the pancreas,27 an extraordinary text compiling all the updated information at that time; it incorporated all the advances in pancreatic surgery, revealed a complete change in mentality and was an absolute contrast compared to previous publications about pancreatic surgery in our country. It also provided the personal experiences of the authors and was a uniquely comparable to another book published only 3 years before in the U.S. by Richard Cattel and Kenneth Warren, Surgery of the pancreas.34
We feel that two factors were key in the advances made during these years in pancreatic surgery at the Hospital Santa Creu i Sant Pau. The first was determined by advances in anesthesia. Dr. José Miguel Martínez played a fundamental role in these new developments when, at the request of the surgeon and Chief-of-Staff Dr. Joan Soler i Juliá, he created the first Anesthesiology Department in the country in 1941.35 His determination, drive and motivation of other anesthetists like Dionisio Montón not only made his Anesthesia Department a prestigious unit throughout the country and main training unit for specialists in Anesthesiology, but it also had an enormous effect on the safety of surgical interventions. In contrast, we should also mentioned that 9 years transpired before the second Anesthesia Department was created in Spain, at the Hospital Marqués de Valdecilla in Santander.
The second factor that contributed tremendously to the first successfully completed PD at the Hospital de la Santa Creu i Sant Pau involves pre- and postoperative care. In this facet, Dr. Artigas was also especially important when he indicated that “…the importance of the operation needed and the state of the patient to be treated require thorough preparation to improve the patient's condition for resisting, normalization of nutrition, and correction of frequent coagulation alterations in cases in which the location of the cancer causes jaundice due to retention.”27 He then proposed a series of measurements aimed at the preoperative correction of these factors, such as hydration “by means of a glucosaline isotonic solution, preferably with an i.v. drip […], mineral ions, nutrition, administration of vitamin K, blood transfusions […], treatment of pancreatic function alterations with the administration of insulin adjusted to the treatment guidelines for pancreatic diabetes and active pancreatic extracts (pancreatin, pancreon, etc.) […] to achieve better nutritional assimilation and anti-infectious treatment […].”27 He likewise proposes “the resuscitation treatment of the patient throughout the operation and in the immediate postoperative period” since the “type of intervention that requires pancreatic excision is prolonged and associated with surgical shock”.27 And all of this 8 years before the creation of the first Intensive Care Unit in Spain, at the Clínica de la Concepción in Madrid (current Hospital Universitario Fundación Jiménez Díaz) in 1963.36
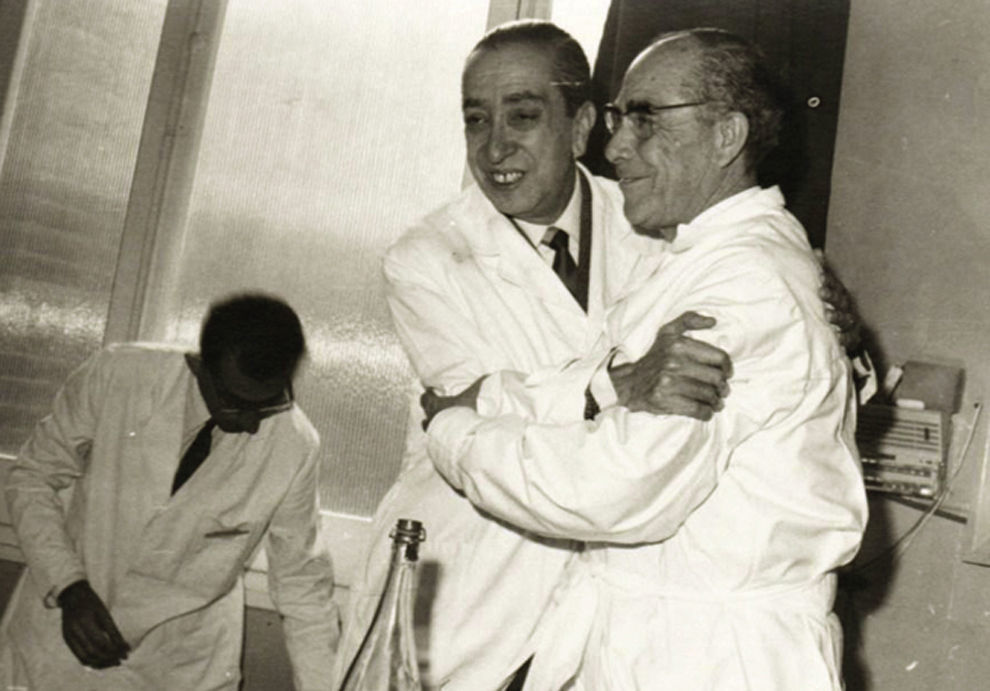
Thus, we have found that, since the 1950s, the first PD have been performed in Spain at the Hospital de la Santa Creu i Sant Pau at the hands of surgeons who made their units the most prestigious in Spanish surgery: Pi-Figueras, Vicente Artigas (Fig. 3), Soler-Roig and Antonio Llauradó. Nonetheless, in terms of the results obtained, we have been able to identify very few references that clearly present their statistics. The following is a summary.
Doctors Jaume Pi-Figueras and Vicenç Artigas Riera in an image from the annual surgery courses at the Hospital de la Santa Creu i Sant Pau (15th Abdominal Surgery Course, Hospital de la Santa Creu i Sant Pau, 1966)
Use authorized by: Galeria de Metges Catalans (http://www.galeriametges.cat/index.php).
In 1959, Soler-Roig, in the monographic text titled “Pathology and symptoms of the terminal portion of the common bile duct”, corresponding with his talk at the 5th Conference of the Surgery Society of the Latin Mediterranean in which he spoke about his vast experience in biliary surgery, he made the following statements referring to his experience with choledochal-duodenal tumors: “[…] and the recent advances in surgical technique have meant that pancreaticoduodenectomy has become included in the radical treatment of malignant neoplasms of the duodenum, papilla and pancreas […]. We have had the opportunity to perform this type of surgery on 2 occasions, with poor immediate results in both cases. […] We hope that, by improving the techniques and applying the indications based on an early diagnosis, better results can be obtained.”37
As for, Pi-Figueras, in his speech at the 21st Conference of the International Surgery Society (Philadelphia, 1966) titled “Pancreatic cancer: techniques for excision surgery” and published in Surgery, Gynecology and Urology, which is the predecessor of the current Cirugía Española, presented an extensive review of theoretical content, but included no postoperative results.38 Nonetheless, 3 years later, Gao Reyero published a review of cases from the department of Pi-Figueras between 1958 and 1968, identifying 4 PD with a mortality of 25%.39 Canals Cadafalch and Olivé Badosa likewise reviewed the patients operated on for biliary duct neoplasm between 1956 and 1965 by Surgery Unit C, directed by Prim Rosell, with 2 PD, although no postoperative results were contributed.40
In 1971, Antonio Llauradó provided the following case study for a postgraduate course in Argentina: “Our experience […] is very limited, but sufficient […][about what] PD means […][we have] practiced PD in 11 cases of cancer of the head of the pancreas. In the immediate postoperative period, 2 patients died […], one of whom was the first in our series, possibly due to lack of experience, and another patient due to injury of the mesenteric artery during surgery. In contrast, we have a patient who is still alive 8 years and 2 months later […]. In the remaining case, survival ranged between 6 months and 2 and a half years. Likewise, we have performed 16 PD due to ampullary cancer […]. In the immediate postoperative period, 4 patients died […]. One patient survived 8 years and 8 months; another 4 patients survived between 1 and 3 years. The 7 remaining patients are currently alive […] and the longest survival […] is almost 10 years […].”41 With these data, we observed that in a total of 27 PD conducted by Antonio Llauradó for cancer until 1971, the mortality rate was 14.81%, and in certain cases prolonged survival was also obtained, which for the first time was attributed in Spain to Dr. Llauradó.23
Finally, in 1976, Dr. Puig la Calle published what seems to be the joint experience of all the departments “reviewing 142 cases of cancer of the head of the pancreas treated surgically at the Hospital de la Santa Creu i Sant Pau, from 1958 to 1972. 65 PD were carried out […] (the Whipple procedure) in 59 patents with a mortality of 30% […]. In the other 6 patients, pancreaticojejunal anastomosis was not done […] [leaving the remaining pancreas] […] ligated en masse […].”42
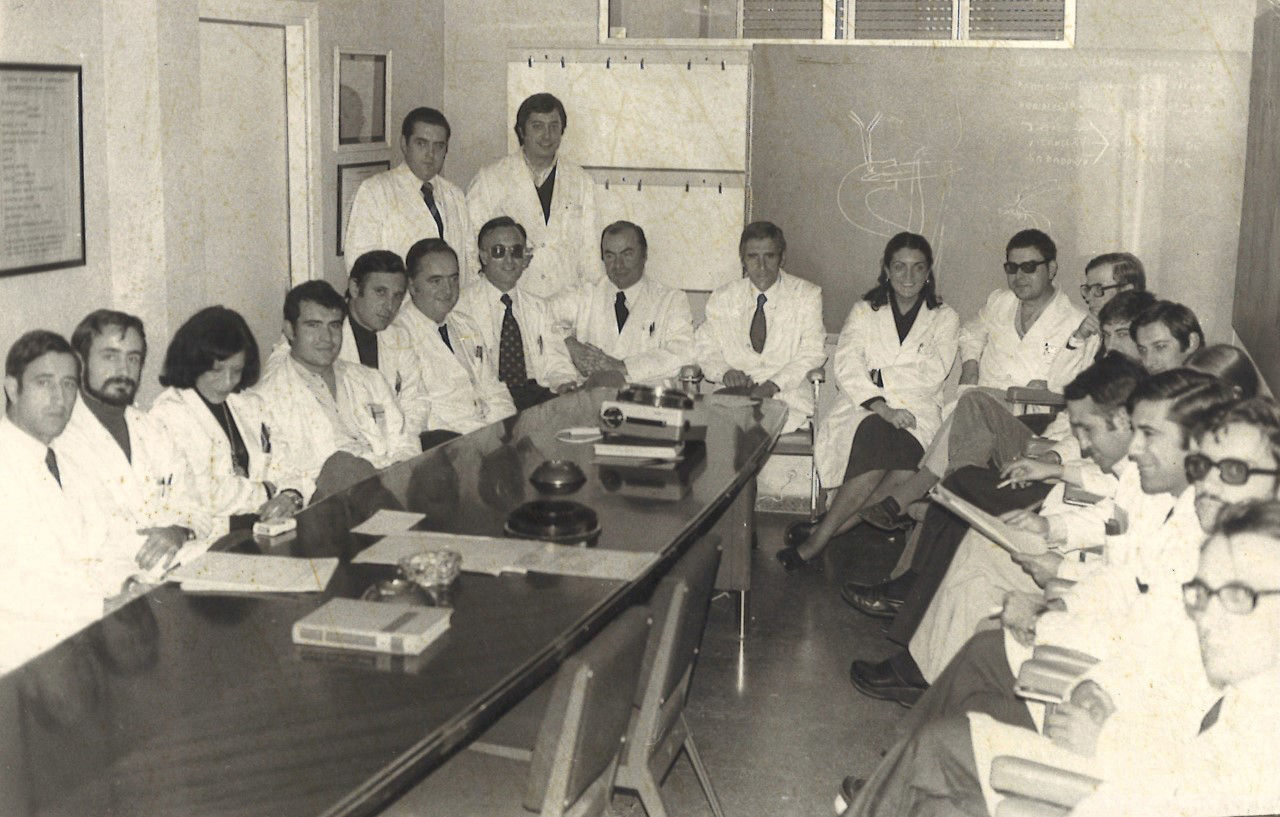
Luis Estrada GonzálezBorn in Avilés in 1922, Dr. Luis Estrada is the second cornerstone of the development of pancreatic surgery in Spain. From very humble beginnings, he studied medicine as a free student while he worked, taking annual exams at medical school in Valladolid and graduating in 1945. In 1941, he passed the entrance exams to begin as an intern at the Surgery Department of the Hospital Provincial in Oviedo. The department was directed by Dr. García Morán, an extraordinary surgeon with German training, who performed the most advanced surgical techniques of the era and who had also been a disciple of Luis Urrutia in Madrid. With an admirable work ethic, natural leader, sportsman and passionate about mountaineering, Luis Estrada was a surgeon for the Seguro Obligatorio de Enfermedad (forefather to the Spanish public health system) and the Red Cross in Oviedo from 1950 to 1972, to later become the head of the Department of Surgery at the Ciudad Sanitaria de Nuestra Señora de Covadonga in Oviedo (Fig. 4). His career as professor began by creating surgery seminars in the 1960s, which were weekly meetings for physicians throughout the province to debate clinical cases and attend conferences or roundtables about current surgery events of the time. With extensive experience in postgraduate teaching with surgeons-in-training, he was responsible for the Surgical Pathology Department at the Medical College, inaugurated in the 1969–1970 academic year, and was named dean. We do not know if he was inspired by his teacher García Morán or by his own fighting entrepreneur spirit, conscious of the fact that the pancreas continues to be the last surgical frontier, Estrada took on pancreatic surgery as the main objective of his professional career. After a stay at the Digestive Pathology School at the Hospital de la Santa Creu i Sant Pau in Barcelona in 1947, with whose members he always maintained a close friendship, and especially with Vicente Artigas, he decided to go to the Lahey Clinic in Boston. There, he was a surgical fellow from 1954 to 1955 with Dr. Richard Cattell and Dr. Kenneth Warren, preeminent figures of the time in pancreatic surgery.43,44 Although afterwards Dr. Estrada shared training, surgeries and knowledge with other illustrious surgeons who had developed personal techniques for the treatment of pancreatic diseases, such as Professor Leger from Paris or Professor Mallet-Guy from Lyon, it was his time at the Lahey Clinic that would truly define his future as a pioneer in pancreatic surgery in Spain.
After returning to Spain, in 1956 Estrada published his first 2 cases of PD due to pancreatic cancer in 2 phases (the first phase cholecystojejunostomy), and both had postoperative survival.45 At the end of that same year at the 8th Conference of the Spanish Society for Digestive Pathologies and Nutrition, he reported 8 cases with pancreatic or periampullary cancer, 3 of which had been able to undergo PD: the one patient who died was the only one who had undergone single-phase surgery.46 Two years later, Estrada conducted the first total pancreaticoduodenectomy in Spain, although the patient died 6 days later due to subsequent metabolic alterations.47
The figure of Estrada is essential to understand the evolution of pancreatic surgery and PD in Spain, not only because of his dedication with a special interest in this surgery, but also due to the presentation of his statistics and the critical analysis of his results. In this sense, of utmost importance is his speech in 1959 at the 5th National Surgery Conference held in Valencia, which was published by the AEC in a book titled Cirugía del pancreas (Pancreatic Surgery), with texts by Estrada (Surgery of Pancreatic Neoplasms) and Vicente Artigas (Surgical Problems Posed by Pancreatopathies and their Complications).47 Later, but still in the same year of 1959, Luis Estrada published the book Cirugía de las neoplasias del pancreas (Surgery of Pancreatic Neoplasms), which was a more extensive and complete version of the aforementioned text and also included chapters on pancreatic anatomy and physiology, diagnosis, anatomic pathology and especially surgical techniques.48 In both texts, the most important element is the first series of 29 patients treated between 1955 and 1959 with pancreatic and periampullary cancer, including 6 PD, one total pancreatectomy one left pancreatectomy and the rest were palliative operations or exploratory laparotomies. Each of the 29 cases of the series is explained in detail and accompanied by a diagram of each procedure (Fig. 1D). And, more importantly, it presents the results for PD, with a postoperative mortality of 33% (50% for single-procedure surgeries and 25% for those done in two phases) and a survival time after resection of 7 months. This is the first extensive series of oncologic pancreatic or periampullary surgery in Spain, and it is a historic event that other surgeons in Spain, including those from the Hospital de la Santa Creu i Sant Pau, frequently cite. In 1970, he conducted a new review including 48 patients with cancer of the pancreas and the ampullary area, including 11 PD, with a drop in mortality to 27.2% and an increase in mean survival to 9 months.49 These numbers clearly contrast with those from the same series but in cases with diversions or palliative interventions: operative mortality of 11.5% and mean survival of 3 months. It is truly a lesson to see how, maintaining a critical spirit, Estrada remained convinced about the radical procedure, and always had the same argument: “Although we are far from satisfied with our results, our opinion is the same as when we presented a series of 29 cases at the Spanish Conference on Surgery. We have attempted to cure our patients when the case was appropriate, and we have always achieved palliation. We believe that in some cases we have extended survival, while in many others we have provided some sort of relief. It is possible that, if we continue with this approach, we will one day be able to make one of our patients survive.”49
Finally, there were another 2 series that would later complete the overall experience of Luis Estrada with pancreatic and ampullary cancer: one from 1979, which included 100 patients treated in previous years, and another from 1981 with 170. The former included 21 PD and 4 total pancreatectomies, and the latter 30 PD and 7 total, with mortality rates for these two interventions of 33 and 28%, respectively,50,51 which are percentages similar to those reported by Dr. Puig la Calle in his review from 1976.42
In short, the first oncologic pancreaticoduodenectomies in Spain were performed in Barcelona, at the Hospital de la Santa Creu i Sant Pau. After the 1950s, a gastrointestinal surgery school arose, founded on the tradition of Salvador Cardenal, Enrique Ribas Ribas and Manuel Corachán, and led by surgeons who became the next generation in Spanish surgery and a reference for the entire country, including Pi-Figueras, Vicente Artigas, Soler-Roig and Antonio Llauradó. As a result of their advances and experience in biliary surgery, they were able to carry out the first PD and lay the technical and practical foundation for pancreatic surgery in Spain. Almost simultaneously, but in Oviedo, Luis Estrada also introduced PD and total pancreatoduodenectomy after a training period with the pioneers in pancreatic surgery in the United States. Working in more of a solitary manner, although with the support of his teacher Dr. García Morán, he followed the tradition of another pillar of digestive surgery in Spain at the beginning of the 20th century, Luis Urrutia.
Authorship/CollaboratorsThe 3 coauthors have participated in locating and analyzing historical material. LSO has composed the original version of the manuscript, and EMP and VAR have contributed to the composition, critical review and final approval.
Conflict of InterestsThe authors have no conflicts of interests to declare.
The authors would like to acknowledge the following:
- Joaquín Díaz Dominguez, Associate Professor at the Universidad Autónoma de Madrid.
- Rafael Estevan Estevan, Chief of Surgery, Instituto Valenciano de Oncología.
- Laureano Fernández-Cruz, Surgery Professor and Chair, Universitat de Barcelona.
- Enrique Martínez Rodríguez, Surgery Professor and Chair, Profesor Eméritus at the Universidad de Oviedo.
- Cristóbal Pera Blanco-Morales, Surgery Professor and Chair, Profesor Eméritus at the Universidad de Barcelona.
- Pilar Salmerón Sánchez, from the Hospital Historical Archives, Hospital de la Santa Creu i San Pau.
- Manuel Trías i Folch, Surgery Professor and Chair at the Universitat Autónoma de Barcelona.
Please cite this article as: Sabater Ortí L, Martín-Pérez E, Artigas Raventós V. Inicios de la cirugía pancreática oncológica en España. Un tributo a los pioneros. Cir Esp. 2017;95:190–198.