Dynamic endoanal ultrasound has emerged in recent years as a test that could replace the now existing tests in the diagnosis of pelvic floor disorders. The aim of this paper is to determine the usefulness of echodefecography in the diagnosis and evaluation of patients with symptoms of anorrectal obstruction, and show the results obtained after its implementation in a pelvic floor unit, as a complementary tool that could replace conventional defecography.
MethodsIn this retrospective study we analysed 66 patients with a mean age of 55 years (19–83), 61 women (92%). All dynamic ultrasound was performed in 3 dimensions and was correlated with symptoms and physical findings in the consultation. A descriptive and inferential study was performed to find a kappa correlation between physical examination and echodefecography.
ResultsThe reasons for consultation were: Anorrectal obstruction syndrome 36 patients (54.5%), pelvic organ prolapse 27 patients (40.9%), and anorrectal obstruction syndrome along with pelvic organ prolapse 3 patients (4.5%). The correlation of the 2 groups indicated that echodefecography diagnosed more patients with grade III rectocele, enteroceles, and anismus than the combination of scan-ultrasound-manometry-proctoscopy (Kappa 0.26, 0.38 and 0.21, 95% CI: from 0.07 to 1.00, 0.15 to 1.00 and from 0.12 to 1.00, respectively) (P<.001). Conversely, echodefecography diagnosed less perineal descense (Kappa 0.28, 95% CI: 0.12–1.00).
ConclusionsDynamic anal ultrasonography may have a role as a complementary test in patients with pelvic floor disorders, achieving diagnoses that would go undetected by inspection, physical examination and manometry.
La ecografía endoanal dinámica (EEAD) en 3 dimensiones ha surgido en los últimos años como una alternativa a las pruebas existentes en el diagnóstico de las alteraciones del suelo pélvico. El objetivo de este trabajo es determinar la utilidad de la ecodefecografía en el diagnóstico y evaluación de los pacientes que presentan síntomas de obstrucción defecatoria, así como mostrar los resultados obtenidos tras su implementación en una unidad de suelo pélvico.
MétodosEstudio retrospectivo que analiza a 66 pacientes (61 mujeres), con una edad media de 55 años (19–83). Se realizó una EEAD y se correlacionó con los síntomas y los hallazgos exploratorios en consulta. Se realizó tanto un estudio descriptivo como inferencial, así como un índice Kappa para buscar correlación entre la exploración física y la EEAD.
ResultadosLos motivos de consulta fueron: síndrome de obstrucción defecatoria (SOD) 36 pacientes (54,5%), prolapso de órganos pélvicos (POP) 27 pacientes (40,9%) y SOD junto con POP 3 pacientes (4,5%). La correlación de ambos grupos indica que la EEAD diagnostica más pacientes con rectocele grado III, enteroceles y anismos que la combinación de exploración-manometría-proctoscopia-ecografía bidimensional (Kappa 0,26; 0,38 y 0,21; IC 95%: 0,07-1,00; 0,15-1,00 y 0,12-1,00, respectivamente) (p<0,001). Por el contrario, la EEAD diagnostica menos descensos del periné (Kappa 0,28; IC 95% 0,12-1,00).
ConclusiónLa ecografía dinámica puede tener un papel relevante como prueba complementaria en el paciente con enfermedad del suelo pélvico, ya que permite diagnosticar procesos que mediante la inspección, la exploración física y la manometría pasarían desapercibidos.
Pelvic floor disorders are frequent, especially in women, in whom the incidence is between 12 and 20%.1 Before prescribing further tests, a thorough clinical history and physical examination are necessary. So far, conventional defecography (CD) has been considered the “gold standard” for the study of disorders of the posterior compartment.2 Nevertheless, it has its limitations; it must be performed in a specific radiological area, the patient is exposed to radiation and it does not allow sphincter evaluation.3
As an alternative to conventional tests, an interest in endoanal and endorectal ultrasonography (EEUS) has emerged in recent years. Murad-Regadas et al. described the technique for the assessment of disorders of the posterior compartment with a 360 transducer and 3D imaging rebuilding. In a study comparing it against defecography, Murad-Regadas et al. showed that it seemed to be just as effective in the diagnosis of abnormalities in the posterior (rectocele, intestinal intussusception and anismus) and mid (enterocoele, degree III)4 compartments.
Although several years have passed and various papers demonstrate its excellence, its application in daily practice has not yet spread.5–8
In this manuscript, we show both the efficacy of EEUS in the diagnosis and assessment of patients with obstructed defecation syndrome symptoms and the results of its application in a pelvic floor unit, as a complementary tool in the study of such patients.
MethodsIn this retrospective observational study, 66 patients with pelvic floor outlet obstruction problems (SOD), a prolapse of the pelvic organ of the posterior compartment (POP) and anismus were assessed between January 2012 and January 2014.
Patients over 18 who met at least 2 Rome III criteria for obstructed defecation,1 clinical evidence of POP or clinical-manometric anismus were included. Those with organic colon disease, anal stenosis, inflammatory bowel disease and pregnant women were excluded. All the patients signed an informed consent form.
All the patients underwent a diagnostic protocol which consisted of a complete clinical history, physical examination, proctoscopy, anorectal manometry and dynamic ultrasound scan.
The same practitioners who recorded the patients’ prior medical history and carried out the physical examination (inspection, cutaneous-anal contractile reflex, perineal descent and rectal examination), manometry and proctoscopy, also performed the EEUS.
Manometry was performed with a 4-channel manometer (Laborie Medica, Bristol, United Kingdom). The length of the anal canal, rest pressure, contraction and recto-anal inhibitory reflex were measured.
An inspection of the perineum during defecation strain allowed us to diagnose perineal descent as a bulging perineum under the ischial tuberosity of more than 2cm during defecation.
Rectal examination allowed us to assess the presence of rectocele (together with a vaginal inspection). Definitions are the following: grade I if it prolapses into the vagina, grade II if the prolapse is up to the vaginal opening, grade III if it prolapses beyond the vaginal opening and, finally, grade IV prolapse out of the vulva. Manometry helped us to diagnose anismus, because due to the lack of relaxation of the sphincter complex during defecation, rest and contraction pressure during defecatory strain were augmented in relation to rest pressure.
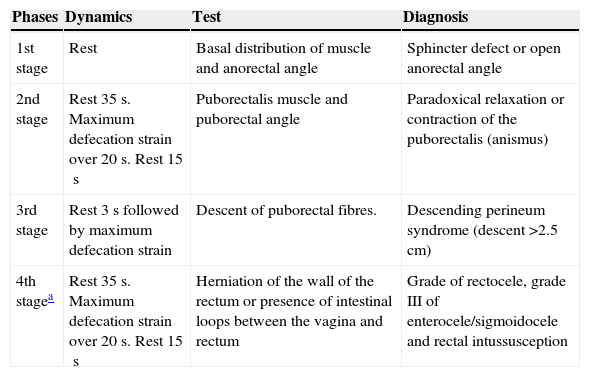
An EEUS was performed with the technique described by Murah-Regadas et al.,3 with a Brüel & Kjaer Flex Focus 2202s ultrasound scanner, 2050 catheter (B-K Medical, Herlev, Denmark). The mean time for exploration was 25min (18–42). In Table 1, the whole procedure is described. Each process was defined as follows:
- -
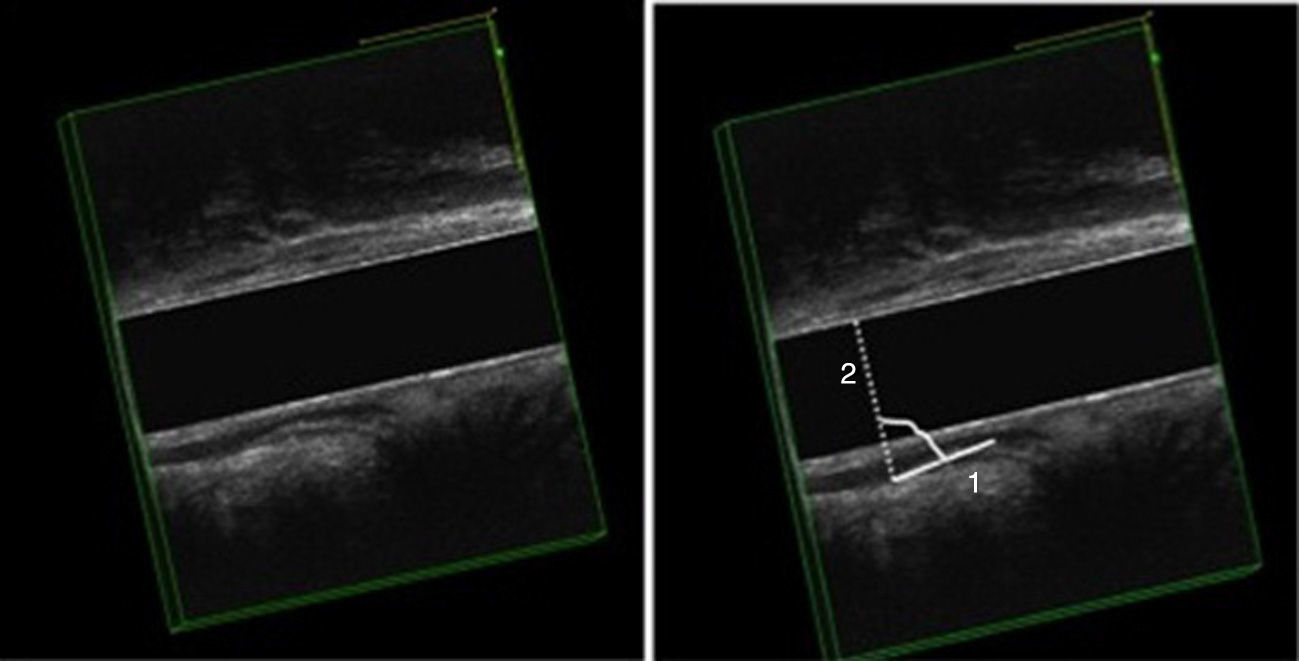
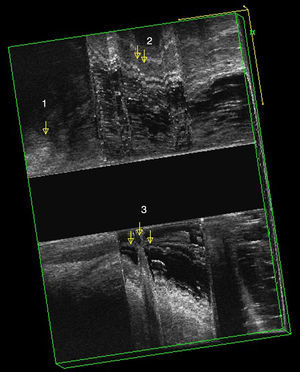
EEUS Anismus: more than one degree of closure of the anorectal angle during defecation, as compared to rest (Fig. 1).
- -
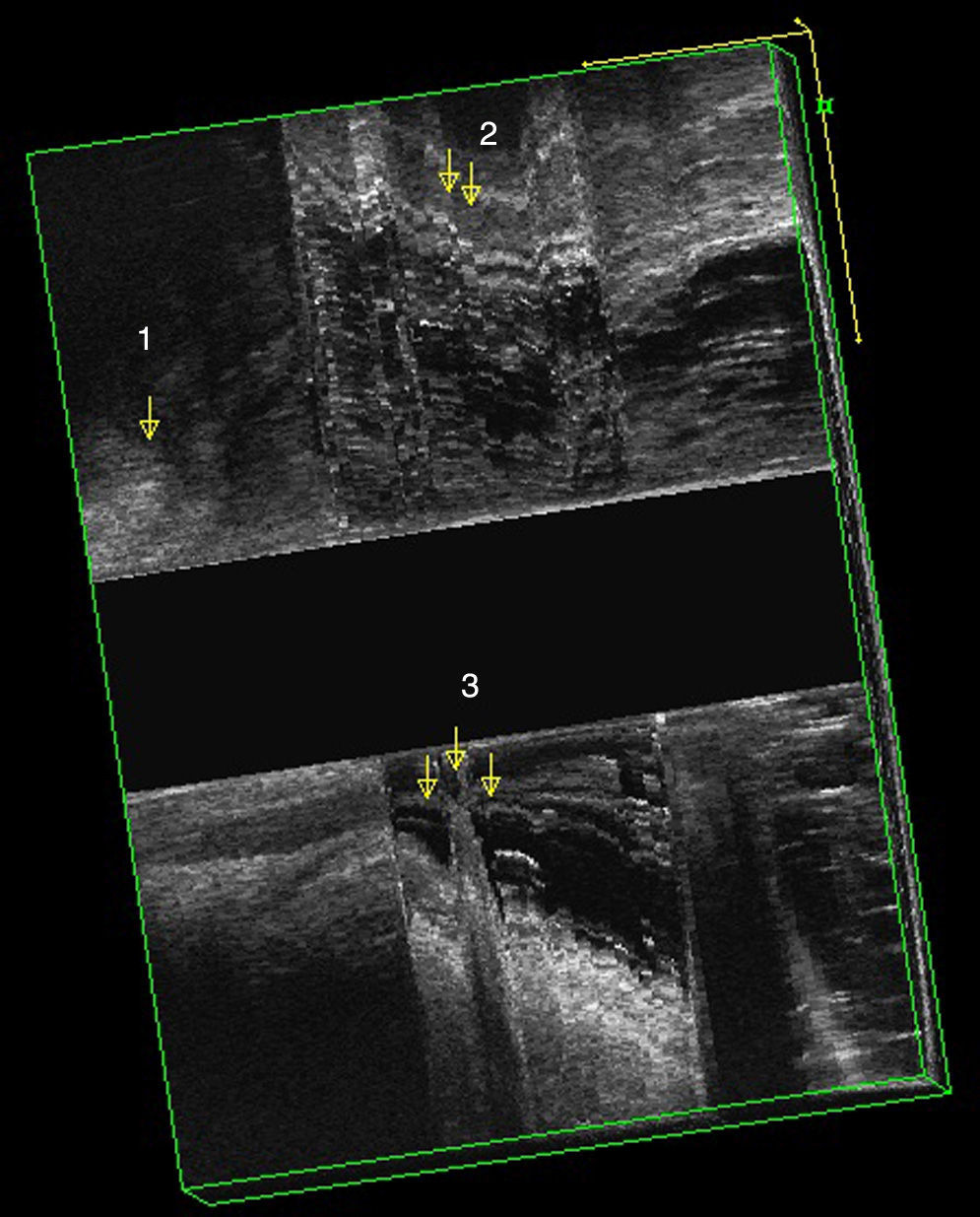
EEUS rectocele: after injecting 150cc of ultrasound gel into the rectum and during defecation straining, an anomalous hypo-echoic image is observed which was not visible at rest. This image corresponds to a hernia of the anterior wall of the rectum filled with ultrasound gel (Fig. 2). Grade I equals to less than 0.6cm, grade II between 0.7 and 1.3cm and grade III more than 1.3cm.
- -
Internal invagination: this cannot be diagnosed clinically. In the ultrasound we can appreciate a “finger like shape” at the anterior or posterior level, which is composed by all the layers of the rectum. The deeper the invagination, the clearer the image (Fig. 2).
- -
Clinical enterocele: vaginal bulging where we can see an intestinal loop, sometimes with eventual peristaltic movements.
- -
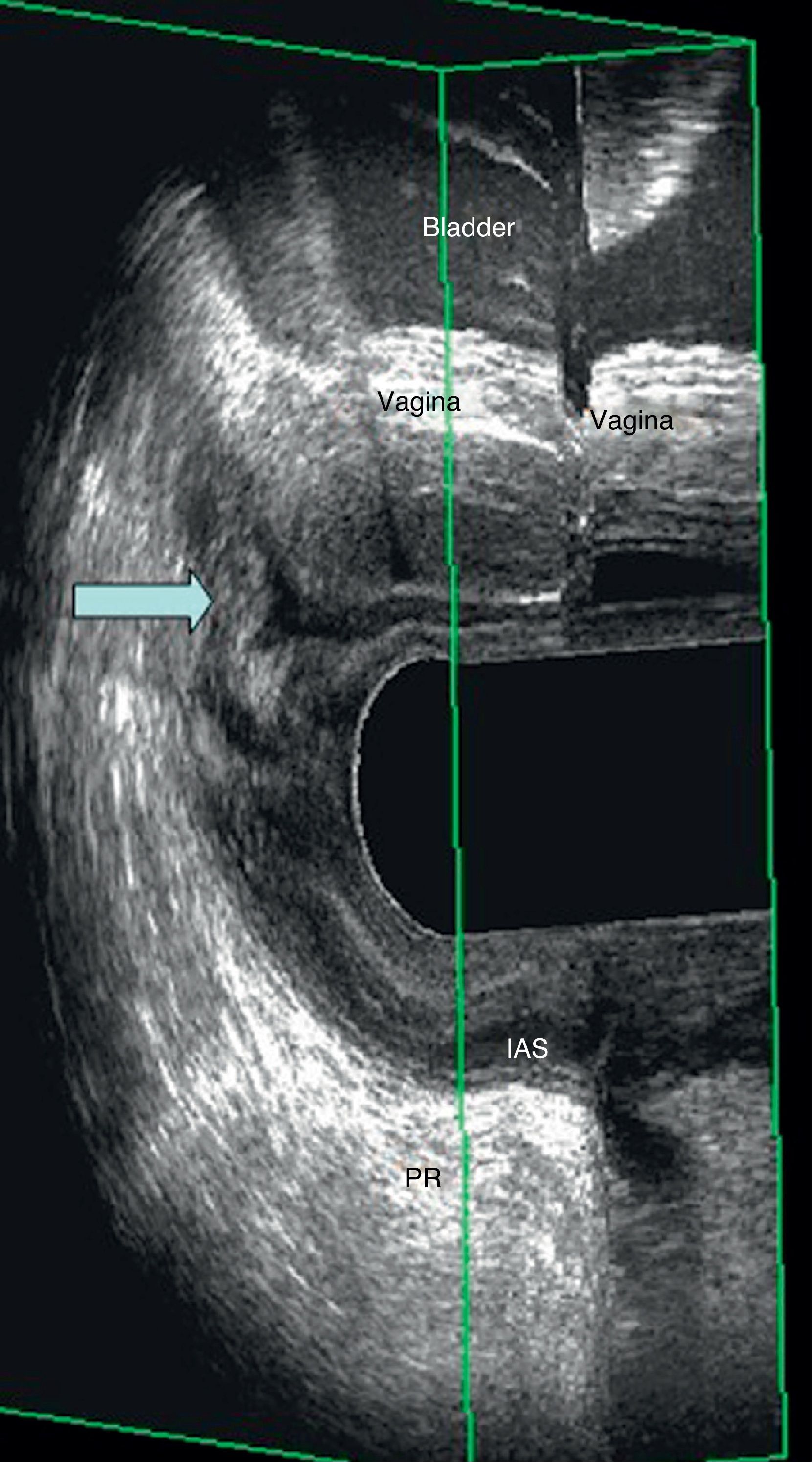
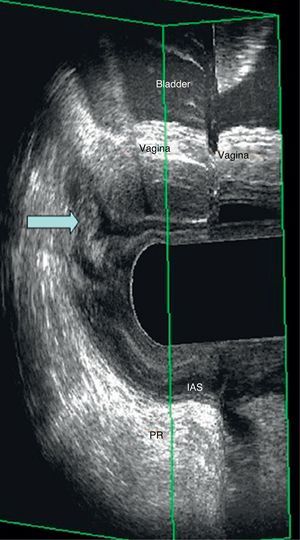
EEUS enterocele: observation of the intestinal loop between the vagina and the rectum during defecation straining; the image observed is similar to that of a “mitochondria”. It can be seen in both the vaginal and rectal ultrasound (Fig. 3).
- -
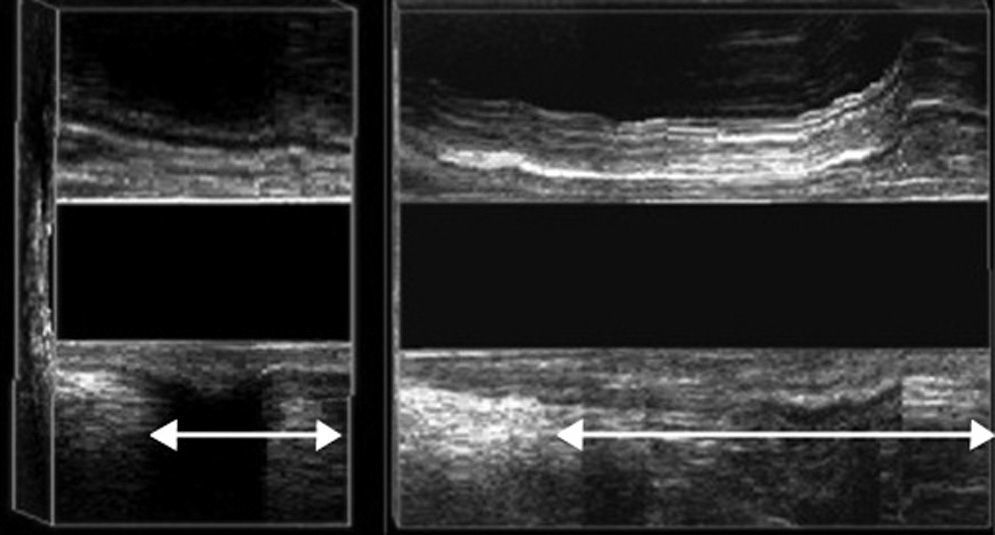
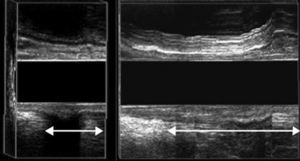
EEUS perineal descent: puborectal descent during maximum strain higher than 2.5cm (Fig. 4).
Description of the Technique According to Murah-Regadas.
| Phases | Dynamics | Test | Diagnosis |
|---|---|---|---|
| 1st stage | Rest | Basal distribution of muscle and anorectal angle | Sphincter defect or open anorectal angle |
| 2nd stage | Rest 35s. Maximum defecation strain over 20s. Rest 15s | Puborectalis muscle and puborectal angle | Paradoxical relaxation or contraction of the puborectalis (anismus) |
| 3rd stage | Rest 3s followed by maximum defecation strain | Descent of puborectal fibres. | Descending perineum syndrome (descent >2.5cm) |
| 4th stagea | Rest 35s. Maximum defecation strain over 20s. Rest 15s | Herniation of the wall of the rectum or presence of intestinal loops between the vagina and rectum | Grade of rectocele, grade III of enterocele/sigmoidocele and rectal intussusception |
Source: Murah-Regadas.2,3
In a descriptive study, qualitative variables are expressed by the number of cases, as well as the percentage with respect to the totality of the variable under study. The Lee coefficient (κ) was used to assess concordance between physical exploration and echodefecography. Values were classified as follows: 0 without concordance between both tests; 0.00–0.39 low concordance; 0.40–0.59 moderate concordance; 0.60–0.79 high concordance; and between 0.80 and 1.00, concordance is almost perfect. Differences were considered significant when the P value was lower than .05. For the execution of the statistical study the SPSS 15.0 for Windows software (Chicago, IL, USA) was used.
ResultsA total of 66 patients (61 women) with a mean age of 55 years (19–83) were included. Twelve patients had undergone a hysterectomy.
Complaints were: SOD in 36 patients (54.5%), POP in 27 patients (40.9%), and both SOD and POP in 3 patients (4.5%).
A clinical examination in combination with an anal and vaginal examination, proctoscopy and manometry allowed us to reach the following diagnoses: anismus in 5 patients (7.6%), rectal prolapse in 23 patients (34.8%), enterocele in 5 patients (7.6%), perineal descent in 22 patients (33.3%) and rectocele in 32 patients (48.4%) (grade I: 9; II: 16; III: 7; grade IV: none). The contraction values of all of the patients were normal.
Ultrasound findings showed: anismus in 21 patients (31.8%), rectal prolapse in 8 patients (12.1%), enterocele in 13 patients (19.7%), perineal descent in 13 patients (19.7%) and rectocele in 46 patients (69.6%) (grade I: 3; II: 12; III: 31). In 3 patients an anterior sphincter defect was found in the external anal sphincter, without repercussions in the manometry.
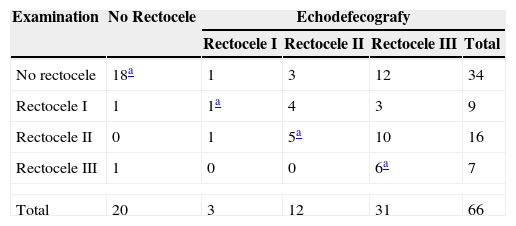
The conditions most frequently diagnosed by ultrasound, which justified the patient symptoms were: rectocele (69.7% of the studied patients), followed by rectoanal intussusception and anismus (33.3 and 31.8% respectively) (Table 2).
Concordance Between Echodefecography and Physical Examination for Diagnosing Rectocele.
The rectoanal intussusception cases found during a dynamic ultrasound coincide with those patients with clinical rectal prolapse. During the ultrasound exploration, a rectal prolapse appears in the form of internal invagination, because the catheter is in the rectum and prevents the prolapse from protruding outwards.
When we compare a physical examination to EEUS, a rectocele was detected in 32 patients after a physical examination and in 46 patients using dynamic ultrasound (P<.002) (Kappa 0.26; IC 95%: 0.07–1.00). Furthermore, an echodefecography exploration was able to diagnose a higher number of patients with grade III rectocele, compared to the physical examination.
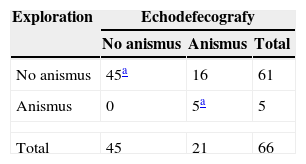
Using manometry, we were only able to diagnose 5 patients with anismus; notwithstanding, a dynamic ultrasound showed an image compatible with anismus in 21 patients (P<.002) (Kappa 0.21; IC 95% 0.12–1.00) (Table 3).
An image compatible with rectoanal intussusception was shown in 22 cases (33.3%).
Perineal descent was detected in 19.7% of patients (13 cases) with dynamic ultrasound. Contrastingly, this figure was higher when a physical examination was performed (22 cases).
The correlation between both groups indicates that EEUS diagnoses more patients with grade III rectocele, enterocele and anismus than a combination of exploration-manometry-proctoscopy-3D ultrasound (Kappa 0.26; 0.38 and 0.21; IC 95%: 0.07–1.00; 0.15–1.00 and 0.12–1.00, respectively) (P<.001). On the contrary, EEUS diagnoses less perineal descents (Kappa 0.28; IC 95% 0.12–1.00).
DiscussionAs we have noted, CD presents significant limitations despite being a technique of high prestige. To overcome these limitations, a dynamic echodefecography is a valid alternative for studying posterior and even medial and anterior compartment behaviour.4–8
Several studies have shown echodefecography to be as valid as CD and MRI defechography, particularly when assessing rectocele, intussusception and anismus. Furthermore, it allows us to see the whole sphincter complex and its dynamic behaviour at closure.5–7
It has clear advantages such as an absence of radiation, better availability, less resource consumption; and, therefore, it is less expensive and easier to perform. The learning curve is relatively short since it only requires 10–20 supervised echodefecographies for it to be performed with accuracy.5,7
Both an echodefecography and a pelvic floor NMR (NMRPF) show similar results in the assessment of pelvic floor disorders compared to CD.9 Despite the NMRPF being performed in a more physiological position than an echodefecography (left lateral decubitus position), an NMRPF can be more emotionally upsetting. Patients say that they feel embarrassed when having to evacuate in front of others, which leads people to avoid these tests. Perniolay et al.10 showed that the discomfort felt by the patient was 7 times less with an echodefecography than that caused by CD, and was also less uncomfortable. Vitton et al. noted that their patients preferred an echodefecography as a follow-up for this reason.9
EEUS proved to have a good correlation to a CD; obtaining accurate results seems to be more influenced by the expertise of the technician than by the position of the patient. Echodefecography is a well-tolerated examination that only requires 10–15 minutes of the patient's time to complete the whole procedure. A small amount of ultrasound gel (150–180ml) is a sufficient stimulus to defecate without the need to use barium paste as in a CD. As well as avoiding radiation, an echodefecography is less expensive than a CD or an NMRPF and similarly sensitive and accurate.11
The excellent view that it gives of the anatomical structure of the pelvic floor seems to make an echodefecography more effective than a CD in some aspects.10 It seems to show anismus, intussusception and grade III enterocele better; reflecting this, Regadas et al. observed 26 cases of anismus with echodefecography and 19 cases with CD; concordance was practically identical with both methods for grade III enterocele. However, an echodefecography seems to have limitations for assessing the anterior pelvic floor behaviour and identifying grade I and II enterocele, due to the limited dynamic rank of the catheter in the rectum. In a transvaginal ultrasound, however, these limitations can be overcome.7,12
As we have seen in our study, we can efficiently diagnose perineal descent, though not as efficiently as through a physical examination or with a CD, probably due to the patient's position during the ultrasound.5
In effect, the findings of a defecography are not always in agreement with symptoms, despite the fact that its pre-surgical use has been demonstrated to be essential because it is more accurate than a physical examination. It can be used as a guide to accurately select the most suitable treatment for the patient.13
Our research data shows that there is low agreement between the results of physical examinations and other basic tests, and dynamic ultrasound. This data coincides with other literature and reveals the need for using a dynamic imaging test to facilitate a diagnosis of pelvic floor disorder. We can guess that physical examination and conventional methods alone might under-diagnose patients with some disorders, such as a grade III rectocele, enterocele or anismus, and over-diagnose others (perineal descent). Taking into account that CD is still the “gold standard”, the latest studies where EEUS and CD are compared show a similar concordance between both studies with an almost identical Kappa index in the diagnosis of pelvic floor disorders. This is why many authors are considering EEUS as a valid option that could substitute defecography.4–8
The main advantage of defecography is the ability to study the anatomic integrity of the structure of pelvic floor at the same time as assessing how it functions during evacuation. Furthermore, the high definition 3D images without anatomic distortions that it obtains allows an examination to be recorded in real time for further detailed analysis. An echodefecography is a simple, reproducible and well-tolerated method that can be performed in a short period of time during a patient consultation.
As a conclusion, we believe that dynamic ultrasound has a relevant role as a complementary test in the study of patients with pelvic floor disorders, since it lets us diagnose disorders that would go unnoticed if assessed through inspection, physical examination and manometry. An accurate knowledge of the technique, standardisation, values and the basic parameters of echodefecography, as shown in this research, are basic elements of this new diagnostic tool to be standardised in our hospitals.
Conflict of InterestThe authors declare that there are no conflicts of interest.
Please cite this article as: de la Portilla F, Rubio Manzanares Dorado M, Pino Díaz V, Vazquez Monchul JM, Palacios C, Díaz Pavón JM, et al. Utilidad de la ecografía dinámica tridimensional en el estudio del suelo pélvico. Cir Esp. 2015;93:530–535.