Advances in oncology and surgical technique, along with studies that demonstrate its importance in survival,1,2 have led to metastatic cancer surgery becoming more frequent. The liver and lungs represent the most common sites of metastasis, particularly in colorectal neoplasms.3 The treatment strategy to be followed in these patients continues to be full of controversy. There are therapeutic regimens that advocate initial resection of the metastases and later resection of the primary tumor, while others recommend the opposite. It is true, however, that there are no data to fully support either vision.4,5 Nonetheless, it seems logical to try to perform the treatment during the same surgery, whenever possible.
Some months ago, our unit treated a 63-year-old woman, with no previous history of interest, who was diagnosed with adenocarcinoma at the descending colon-sigmoid junction with numerous unresectable synchronous hepatic and pulmonary metastases, for which she had received neoadjuvant chemotherapy with 5-fluorouracil (5-FU) and oxaliplatin. Post-chemotherapy follow-up studies showed its effectiveness, as the disease was reduced to the sigmoid lesion, a single hepatic metastasis measuring 2.5cm in segment VII and another single lesion measuring 2cm in the right lung base.
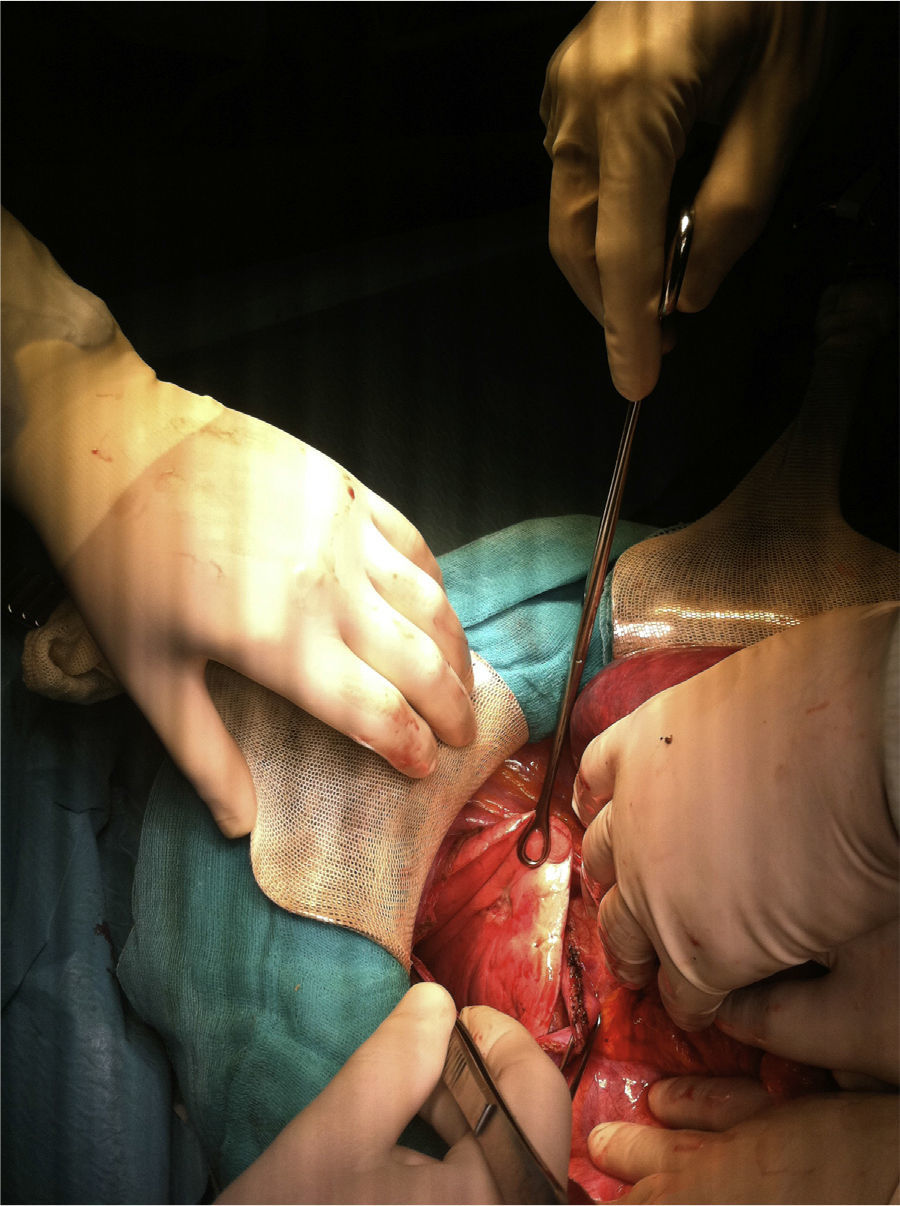
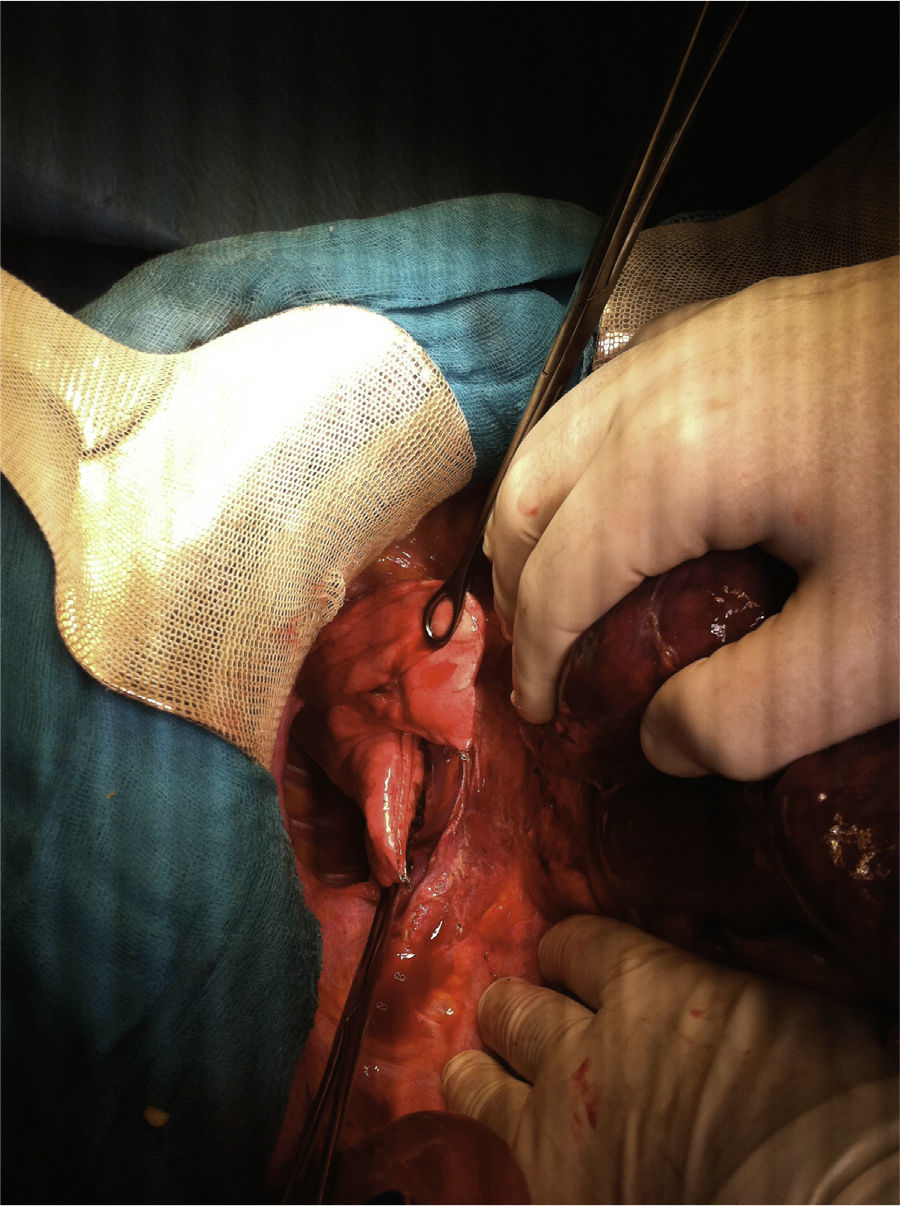
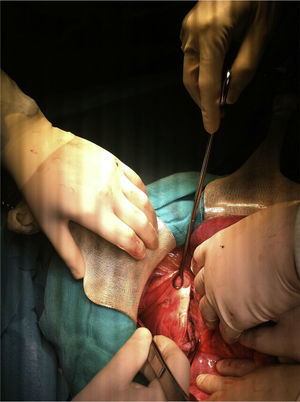
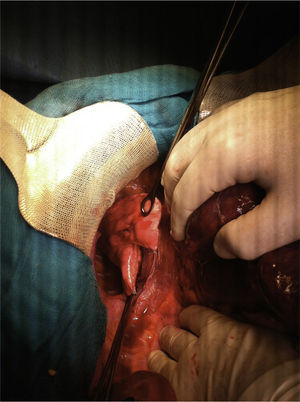
Through a Río-Branco incision and after confirming the single liver lesion by intraoperative ultrasound, the following procedures were carried out in this order: hepatic and lung metastasectomies, and left hemicolectomy with primary end-to-end anastomosis. The approach of the pulmonary tumor was done transdiaphragmatically, with opening of the right diaphragm and traction of the lung base toward the abdominal cavity (Fig. 1). Once the lesion was located, it was resected with a stapler (Fig. 2). Afterwards, the diaphragm was closed with a continuous suture of absorbable material, leaving a drain tube in the pleural space. Prior to closing, two other drains were inserted in the abdominal cavity.
The patient had a favorable recovery and 48h after surgery the pleural drain and one of the abdominal drains were withdrawn. The other drain was removed on the sixth day post-op upon being discharged with no surgical complications. At the writing of this paper six months after surgery, there were no complications and the patient remained disease free.
Patients who present liver metastases at the time of diagnosis often have synchronous lung lesions. In experienced hospitals, when these tumors are resectable, these patients may benefit from a combined approach during the same surgical intervention. The standard procedure, even when performed in the same operation, usually involves both abdominal and thoracic approaches.6 Nevertheless, some selected cases, such as ours, with lesions located in the liver and right lung, can be completely resected with a single approach. This surgical strategy reduces operating time as well as complications associated with prolonged anesthesia. In addition, an incision less would also logically imply a lower rate of surgical site complications. In our case, the patient had three tumor foci resected from three different organs through a single incision, with no morbidity associated with the procedure. This is the first published case of a resected primary colorectal tumor with liver and lung metastases in the same surgery using the transdiaphragmatic approach.
Only a few similar cases have been reported in the literature to date. In 2006, Dionigi et al.7, published a series of three patients who underwent abdominal and thoracic procedures using the transdiaphragmatic approach and minimally invasive instruments. Like us, Dionigi concluded that in expert hands this procedure is feasible and safe. From another point of view, the opposite approach has also been reported with satisfactory results. In 2008, Delis et al.8 presented a series of 7 patients who simultaneously underwent resection of liver (located in segments VII and/or VIII) and lung metastases using the transdiaphragmatic approach and thoracotomy exclusively, without finding additional complications with this surgical technique.
In conclusion, according to the limited literature on the subject and based on our experience, the transdiaphragmatic approach seems to be safe and feasible for the removal of metastatic lesions of the liver and lung. Thus, patients with resectable hepatopulmonary metastatic disease may benefit from treatment in a single surgery and, in selected cases, the transdiaphragmatic approach. In the future, a further step along these lines will be the resection of a primary tumor, liver and lung metastases in one surgical intervention and using a single, minimally invasive approach, be it either thoracoscopic or laparoscopic.
Please cite this article as: Medina Fernández FJ, Espinosa Jiménez D, Luque Molina A, López Cillero P, Rufián Peña S. Abordaje transdiafragmático de metástasis hepatopulmonares: casos que apoyan su viabilidad y seguridad. Cir Esp. 2014;92:60–62.