Congenital arteriovenous malformations (AVM) are frequently found in the lower extremities, and their localization in the thoracic wall is extremely rare. When they are very large, there is a risk of bleeding. This is an added difficulty when planning surgical treatment, and preoperative embolization is occasionally required.1,2
We present the case of a 20-year-old patient with no prior medical history who came to our consultation due to thoracic pain associated with a large chest wall mass that had been growing slowly for 9 years. Examination revealed a poorly defined left lateral thoracic tumor formation measuring 10cm that fluctuated in size, apparently adhered to the muscle plane.
An initial ultrasound of the left periscapular area revealed a heterogeneous nodular focal lesion with poorly defined edges. Color Doppler showed considerably large vessels in its interior, findings that could correspond with a vascular lesion, probably soft tissue hemangioma.
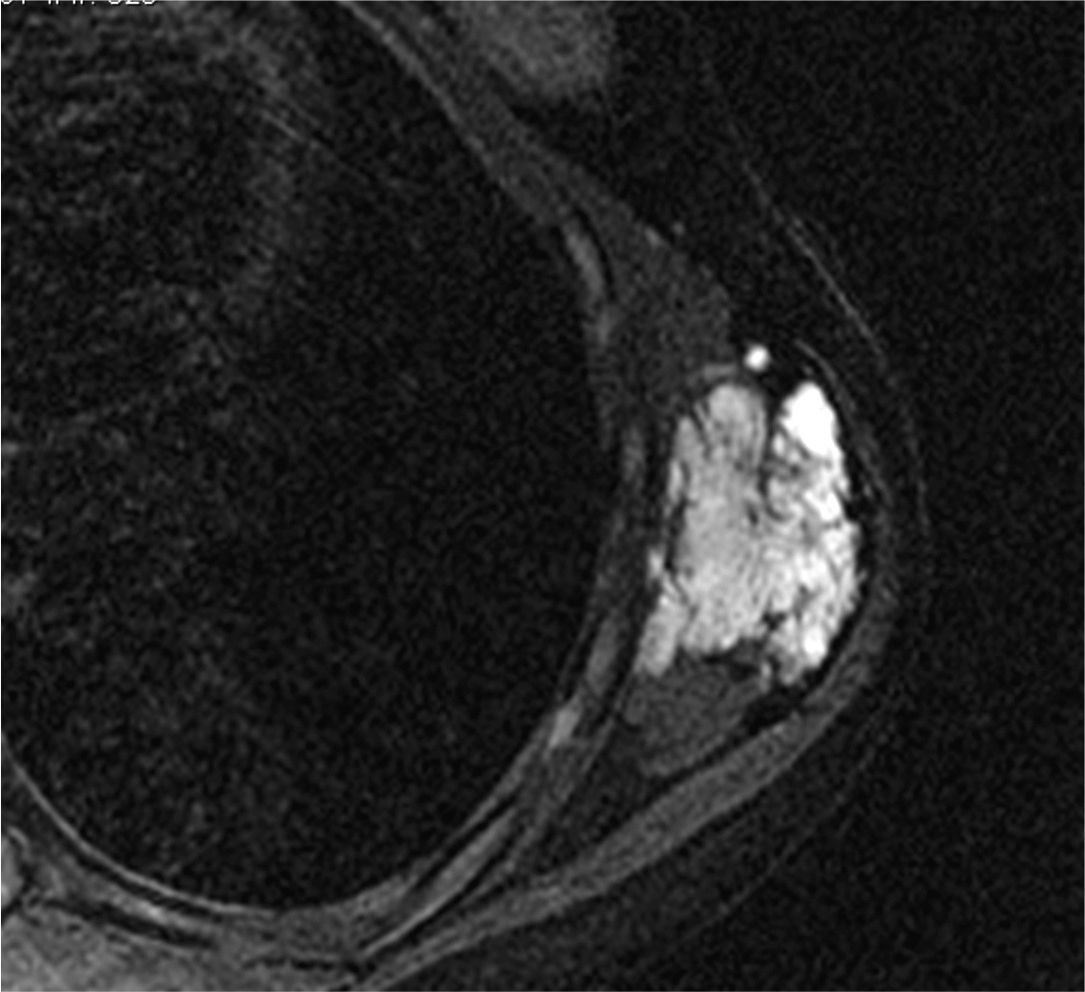
In order to more precisely outline the lesion, a magnetic resonance imaging study was ordered (Fig. 1), which showed evidence of a solid mass in the left serratus anterior muscle measuring 11cm×5.5cm×3.3cm (craniocaudal, anteroposterior and lateral, respectively), that was notably hyperintense in T2, with a winding path and exhibiting signal void phenomenon in its center related with high-flow vessels, denoting the vascular nature of the mass.
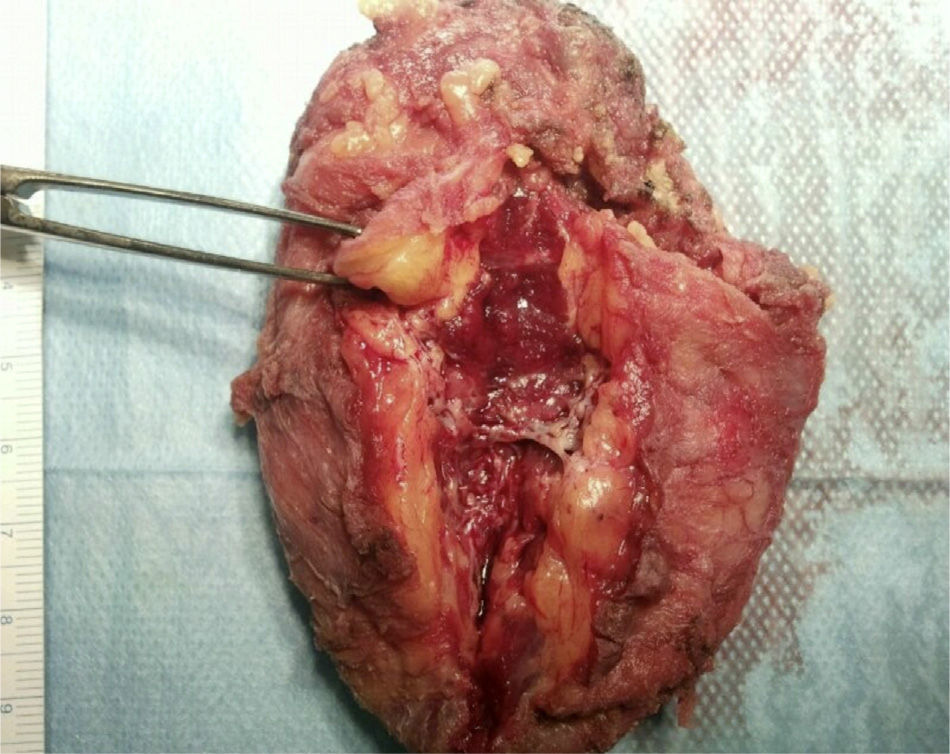
We decided to make an incision over the area of the lesion and then removed an oval tumor measuring 8cm×7cm×2cm in the serratus muscle (Fig. 2), whose upper end passed the tip of the scapula, without infiltrating the costal plan. In its interior, there was a conglomeration of vascular-looking elements, some of them with a congestive appearance.
The pathology study reported the lesion to be an arteriovenous malformation.
Arteriovenous malformations are a network of multiple direct communications between arterial and venous branches without capillary network amongst them.3 They often involve the peripheral vascular system although they can occur in any organ.4 They are defects in the circulatory system that generally occur during embryonic or fetal development.
AVM may be classified as either acquired or congenital, which are very rare. Although present at birth, symptoms are usually not seen until adulthood, normally in the second or third decades of life. Acquired forms often result from trauma, cirrhosis, neoplasms or infections.1
Depending on their location, arteriovenous malformations may be asymptomatic or, on the contrary, they may cause serious symptoms. There is one published case of chest wall compression due to rupture of an AV fistula.5 Likewise, there are reports of mediastinal and intrapulmonary intercostal localizations.6 Within the thoracic cavity, pulmonary AVM are the most frequent (2–3 cases per 100000 inhabitants), occasionally associated with Rendu–Osler–Weber syndrome.3
AVM can cause symptoms when they are infectious, causing compression of adjacent structures due to their size or bleeding. Symptomatic cases that have been published involved brachycephalic, intercostal and internal mammary arteries,7 most frequently in the right upper extremity, which may be related to the complex embryonic development of the right subclavian artery.1
Early diagnosis and appropriate treatment of these lesions are necessary as there may potentially be severe symptoms such as congestive heart failure due to the shunt effect or important bleeding.
On other occasions, the discovery of AVM may be an incidental finding during imaging testing for another cause.
Effective diagnostic tests include Doppler ultrasound, magnetic resonance imaging and angiography, which show the exact vascular architecture of the lesion in cases of high-flow lesions. Ultrasound and MRI were the tests indicated in our patient, since the latter correctly defines the origin of the lesion and its relationship with adjacent structures.
As for treatment, surgical removal is accepted as the definitive treatment, although we must take into account that the results are variable in terms of recurrences and the risk of intraoperative bleeding. Preoperative embolization in order to obliterate the abnormal arteriovenous connections can be useful to reduce bleeding and improve long-term recurrence rates.
We have not found in the literature any cases of intramuscular AVM such as the one presented in our patient. In conclusion, we can say that AVM of the chest wall are uncommon lesions, and that correct differential diagnosis is necessary for proper management. The only symptom of our patient was the sensation of a mass that had been growing since childhood.
Please cite this article as: Arroyo Pareja L, García Gómez F, Barrera Talavera MD, de la Cruz Lozano FJ, Moreno Mata N. Malformación arteriovenosa en músculo serrato mayor. Cir Esp. 2014;92:58–60.