Although the conventional treatment of patients with stage IV colorectal cancer involves resection of the primary tumour followed by chemotherapy, several studies suggest that in patients with few symptoms the first and only treatment should be chemotherapy. The objective of this study is to analyse the complications related to the primary tumour in a series of patients with unresectable metastatic colorectal cancer treated with chemotherapy without surgery.
Materials and methodsRetrospective descriptive study. The study included all patients with unresectable metastatic colorectal cancer treated with chemotherapy without resection of the primary tumour (January 2007–February 2011).
ResultsThe mean age of the 61 patients analysed was 67±13 years and the performance status was 0-1 in 53 (87%). Twenty (33%) patients developed complications during follow-up. The most common complication was intestinal obstruction in 15 (25%) patients followed by perforation. Complications required surgery in 6 (10%) cases. We did not find differences in patient characteristics between those who had a complication and those without, although the complication rate in patients with a colonic stent (53%) was twice that of other patients (26%).
ConclusionsChemotherapy without surgery is a good option in most patients with unresectable metastatic colorectal cancer. However, although the percentage of patients requiring surgery is low, the total number of complications related to the primary tumour is not negligible. Studies are needed to identify those patients in whom a prophylactic colectomy could be indicated.
Aunque el tratamiento convencional de los pacientes con cáncer colorrectal en estadio iv ha consistido en la resección del tumor primario seguida de quimioterapia, varios estudios defienden que en pacientes poco sintomáticos el primer y único tratamiento debe ser quimioterapia. El objetivo es analizar las complicaciones relacionadas con el tumor primario en una serie consecutiva de pacientes con cáncer colorrectal y metástasis irresecables tratados con quimioterapia sin cirugía.
Material y métodosEstudio descriptivo retrospectivo. Se ha incluido a todos los pacientes con cáncer colorrectal y metástasis irresecables en los que se decidió realizar quimioterapia sin resección del tumor primario durante el periodo enero 2007-febrero 2011.
ResultadosLa edad media de los 61 pacientes analizados era de 67±13 años. Veinte (33%) pacientes presentaron alguna complicación durante el seguimiento. La complicación más frecuente fue la obstrucción intestinal en 15 (25%) seguida de la perforación. Las complicaciones precisaron cirugía en 6 (10%). No hemos encontrado diferencias estadísticamente significativas en las características de los pacientes entre aquellos que presentaron una complicación y los que no, aunque el porcentaje de complicaciones entre los portadores de prótesis colónica (53%) dobló el del resto de pacientes (26%).
ConclusionesLa quimioterapia sin cirugía es una buena opción en la mayoría de los pacientes con cáncer colorrectal y metástasis irresecables. Sin embargo, aunque el porcentaje de pacientes que precisan cirugía es bajo, el número de complicaciones relacionadas con el tumor primario no es despreciable. Se necesitan estudios que permitan identificar a aquellos pacientes en los que estaría indicada una colectomía profiláctica.
Considering both sexes, cancer of the colon and rectum has the highest incidence of any malignant tumour, with more than 25500 new cases annually in Spain, and the second highest mortality with some 14000 persons dying each year as a result.1 Approximately 20% are diagnosed at stage IV; hepatic metastases are the most frequent, followed by pulmonary metastases. The metastases are unresectable in over 80% of these patients, thus ruling out surgery with curative intent.2,3 While some patients present symptoms related to the primary tumour (lower GI bleeding, anaemia, intestinal obstruction or abdominal pain), others barely have any symptoms or are completely asymptomatic.
The surgical treatment of patients with colorectal cancer (CRC) in stage IV is controversial. For many years, the treatment strategy consisted of resection of the primary tumour, independently of the presence or absence of symptoms, followed by chemotherapy.4,5 The goal of the surgery was to avoid possible complications of the colonic neoplasm such as perforation, obstruction or haemorrhage and, according to some authors, increase survival.6,7 However, it has been suggested that in patients with few symptoms or those who are asymptomatic, the first and only treatment ought to be systemic chemotherapy.8,9 In patients with stenosing neoplasms, chemotherapy could be combined with placement of an endoscopic stent. This new treatment proposal is based on several motives: the impossibility of offering surgery with curative intent, the need to offer early systemic treatment, the morbidity associated with resection of the colon, and the delay in initiating chemotherapy treatment, especially if complications appear.8–12 In addition, the immunosuppressed state induced following any surgical intervention is said to activate growth factors that could stimulate neoplastic growth.9,13
In addition, the use in recent years of new chemotherapeutic drugs such as irinotecan and oxaliplatin in combination with monoclonal antibodies such as cetuximab or bevacizumab has made it possible to obtain response rates of 50% and increase mean survival in these patients up to 20 months in prospective clinical trials.14,15 This increased survival could be associated with a higher number of complications related to the unresected primary tumour in patients who were initially asymptomatic; this heightens the controversy over which is the best treatment option in these cases.
The Functional CRC Unit of the Hospital del Mar decided in 2007 that stage IV patients with unresectable metastases who were asymptomatic or had few symptoms, would be treated with chemotherapy without resection of the primary tumour. The goal of this study is to analyse the complications related to the intact primary tumour in these patients.
Materials and MethodsA descriptive, retrospective study on a prospectively maintained database that includes all patients diagnosed and treated for CRC at the Functional Unit of the Hospital del Mar. We analysed the period between January 2007 and February 2011 and identified all the patients in stage IV at the time of diagnosis. When a patient is diagnosed with CRC in stage IV, the resectability of the hepatic or pulmonary metastases is evaluated first. Since 2007, patients with metastases considered unresectable have been treated with chemotherapy without resection of the primary tumour as long as they are asymptomatic or have few symptoms. Patients in stage IV with signs and symptoms of present or imminent intestinal obstruction who can be palliatively managed with an endoscopic stent are also treated with chemotherapy without surgery. Furthermore, in selected patients in whom endoscopy shows complete stenosis, prophylactic placement of an endoscopic stent is prescribed before initiating chemotherapy, even though they may be asymptomatic. In this way we included in the study group all of those patients with CRC in stage IV who were treated with chemotherapy without resection of the primary tumour, with or without placement of an endoscopic prosthesis. We excluded patients in whom resection of the primary tumour was indicated for symptoms that could not be palliated with medical or endoscopic treatment, and also those patients for whom only palliative care was indicated.
All patients were informed of the potential benefits and risks of not resecting the primary tumour and of administering only systemic chemotherapy, as well as regarding the control of symptoms with measures such as analgesia and laxatives. Possible clinical complications related to the unresected colon cancer were also closely monitored.
In the group of patients analysed, we recorded demographic variables; tumour-related variables such as location, histologic type, local and remote extension; type of chemotherapy administered and duration; and concomitant administration of palliative radiotherapy. We identified those patients in whom an endoscopic prosthesis was implanted before the start of treatment, and we recorded primary tumour-related complications classified according to the Clavien–Dindo criteria,16 the time elapsed from the start of treatment until the onset of the complication, and its treatment.
We performed a descriptive analysis in which the quantitative variables were expressed as a mean and standard deviation if the distribution was normal, or as a median and interquartile range (25th–75th percentile) if the distribution was not normal. Categorical variables were expressed as absolute numbers and percentages. The comparison of quantitative variables was performed using the Student t parametric test, when the application conditions were met. Otherwise, non-parametric tests were used. The chi-square test was used for categorical variables. Statistical significance was considered to exist when P was less than .05. Data analysis was performed with the SPSS version 18.0 program.
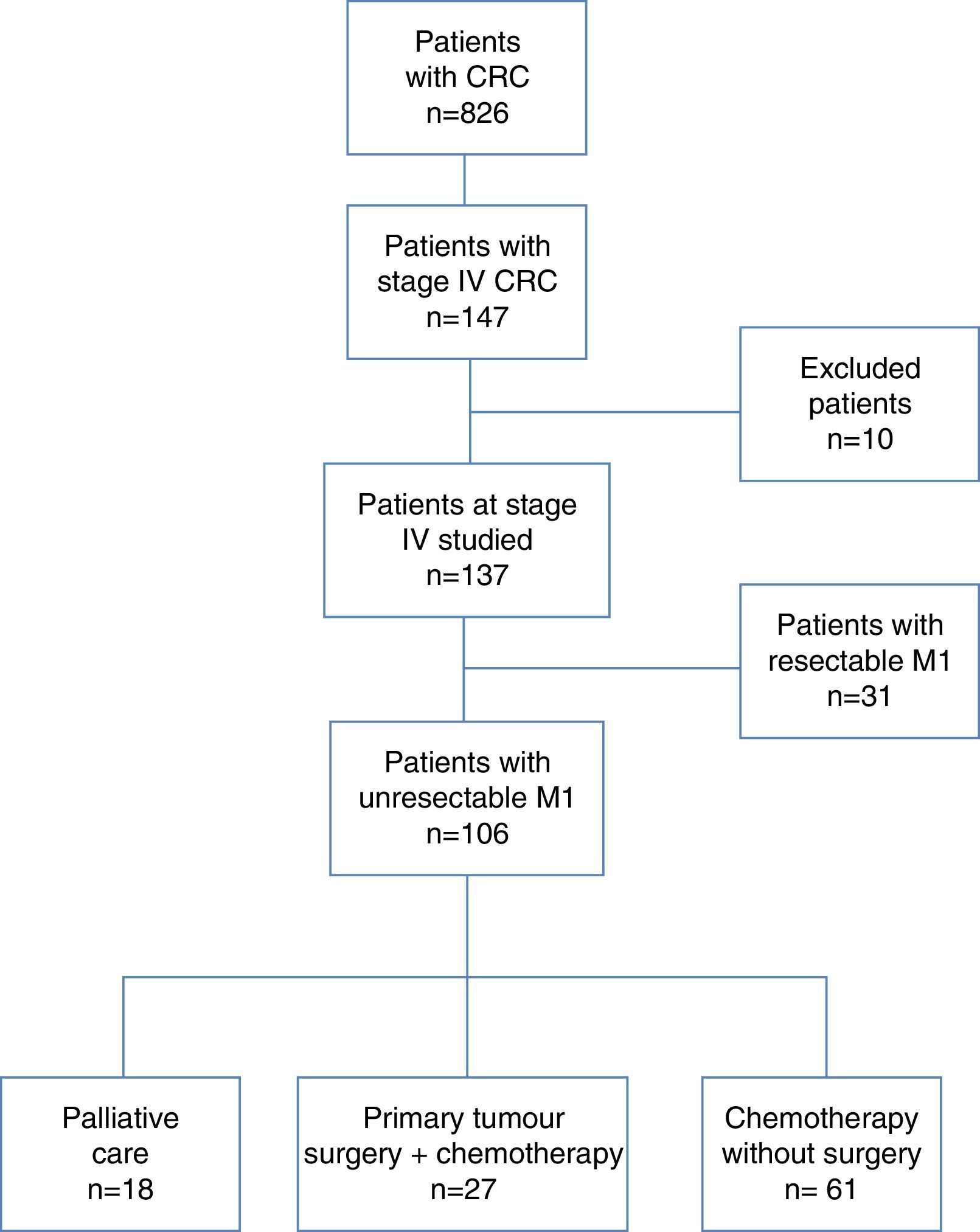
ResultsFig. 1 shows the flow chart that part of the patients with CRC diagnosed during the study period (n=826) of which 147 (18%) presented metastases. Ten patients were excluded for various reasons such as transfer to their city of origin, transfer to another centre or incomplete study. Of the 137 remaining patients in stage IV, 31 (23%) cases had resectable metastases and were operated on for these and for the primary tumour in one or 2 procedures, depending on the case. In the other 106 patients, the metastases were considered unresectable. After presentation of the cases in the CRC Functional Unit, it was decided to provide palliative care only in 18 patients, to resect the primary tumour followed by chemotherapy in 27 patients, and to administer chemotherapy without resection of the primary tumour in 61 patients. This last group of patients is the subject of this study.
The mean age of the 61 patients with unresectable metastases treated with chemotherapy was 67±13 years; 40 (65%) were male. The performance status (PS) was 0-1 in 53 (87%) patients. Two patients presented signs and symptoms of intestinal obstruction which required emergency placement of an endoscopic stent. The other 59 patients were asymptomatic or presented minimal symptoms related to the primary tumour, which could be controlled with outpatient medical treatment.
The most frequent tumour location was in the left colon and rectum in 28 (46%) and 20 (33%) patients respectively, and the histologic type was adenocarcinoma in 58 (95%) cases. Lower gastrointestinal endoscopy was incomplete due to stenosis in 23 (38%) patients. Abdominal computerised axial tomography (CT) showed signs of local infiltration in 46 (75%); there was involvement of the pericolic fat in 39 of these and of adjacent organs in 7. Signs of primary tumour necrosis were seen on CT in only 2 patients.
The extension study showed hepatic metastases in 57 (93%) patients. The metastases involved both hepatic lobes in 47 (77%) of these patients, and the great majority (76%) presented more than 4 lesions identified on CT. The mean number of hepatic segments involved was 6±3. Pulmonary metastases were identified in 22 (36%) patients; these were bilateral in half of the patients. Twenty-four (39%) patients presented, in addition, metastases in other locations such as the retroperitoneum, adrenal glands and bone. Finally, 10 (16%) patients showed initial signs compatible with carcinomatosis, such as peritoneal nodules or thickening of the omentum, in the extension study.
In addition to the emergency placement of an endoscopic stent at the time of diagnosis in 2 patients, it was decided to perform prophylactic placement of a stent in another 13 patients who, although they did not present obvious clinical signs of obstruction, had almost complete stenosis on endoscopy. In all, 15 (25%) of the 61 patients had a colonic stent when chemotherapy was initiated.
The initial chemotherapy treatment used most frequently was the combination of capecitabine and oxaliplatin in 21 patients, followed by 5-fluorouracil (5-FU) and oxaliplatin in 15, capecitabine in 10, and the combination of 5-FU and irinotecan in 8. Carboplatin and VP-16 were used in 3 patients with neuroendocrine tumours. In addition, bevacizumab was administered as first-line or subsequent treatment in 21 (34%) patients. The time period from diagnosis to start of treatment was 20 (11–27) days. The mean duration of chemotherapy treatment was 12±8 months; 7 (12%) patients withdrew from treatment because of toxicity. In a group of 10 (16%) patients with cancer of the rectum, palliative radiotherapy was also administered. Four (7%) patients had a very good response to chemotherapy which allowed subsequent surgical rescue with resection of the hepatic metastases and the primary tumour, although they had been initially considered unresectable. Median patient follow-up was 342 (212–632) days.
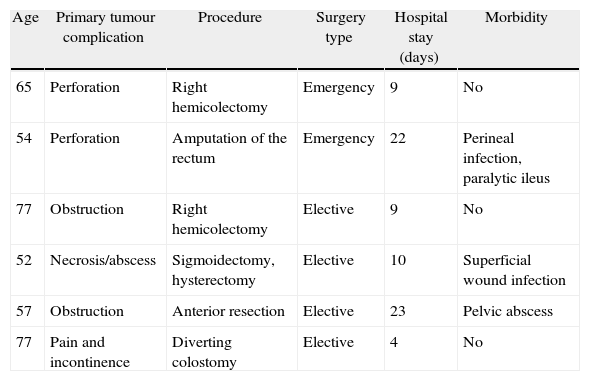
In total, 20 (33%) patients in the study group presented a complication related to the primary tumour during the follow-up period. The time period from diagnosis to onset of the complication of the primary tumour was 6 (3–12) months. The most frequent complication was intestinal obstruction in 15 patients. Perforation or tumour necrosis with abscess formation occurred in 4 cases, while one patient presented pain that was not controlled with medical treatment. The complications were more frequent in those patients in whom an endoscopic stent had been previously placed, in comparison with those in whom chemotherapy was the only initial treatment: 8 out of 15 (53%) and 12 out of 46 (26%) respectively (P=.056), although the difference did not reach statistical significance. In the 8 patients with a stent who developed a complication, this was an obstruction resulting from endoluminal tumour growth. The complications required surgical treatment in 6 (10%) cases; resection of the primary tumour was performed in 5 of these and a diverting colostomy in one. The surgery was performed on an emergency basis in only 2 (3%) patients, while an elective surgical procedure was scheduled in the other 4 (7%). Table 1 shows the surgical procedures performed and their associated morbidity. None of the 6 patients who received surgery died in the immediate postoperative period; their median survival was 480 (240–720) days. In the remaining 14 patients with primary tumour complications who did not require surgical intervention, treatment was as follows: endoscopic stent in 5 (8%) patients with intestinal obstruction, medical treatment in another 2 (3%) patients with obstruction, and palliative care in 7 (11%) patients with very advanced disease and a PS of 3 or higher. In these patients who received palliative care only, the most frequent complication was intestinal obstruction in 5 cases, followed by perforation in 2. Median survival following the complication in these 7 patients was 12 (5–40) days. Following the Clavien–Dindo classification, 2 patients presented grade II complications, 5 patients presented grade IIIa complications and 6 patients had grade IIIb complications. The 7 patients who received only palliative care died days after the complication (grade V), although the rapid progression of the disease contributed as much as or more than the complication to the final result in all of them.
Surgical Procedures and Postoperative Morbidity in the 6 Patients Who Required Surgery to Treat Complications of the Primary Tumour.
| Age | Primary tumour complication | Procedure | Surgery type | Hospital stay (days) | Morbidity |
| 65 | Perforation | Right hemicolectomy | Emergency | 9 | No |
| 54 | Perforation | Amputation of the rectum | Emergency | 22 | Perineal infection, paralytic ileus |
| 77 | Obstruction | Right hemicolectomy | Elective | 9 | No |
| 52 | Necrosis/abscess | Sigmoidectomy, hysterectomy | Elective | 10 | Superficial wound infection |
| 57 | Obstruction | Anterior resection | Elective | 23 | Pelvic abscess |
| 77 | Pain and incontinence | Diverting colostomy | Elective | 4 | No |
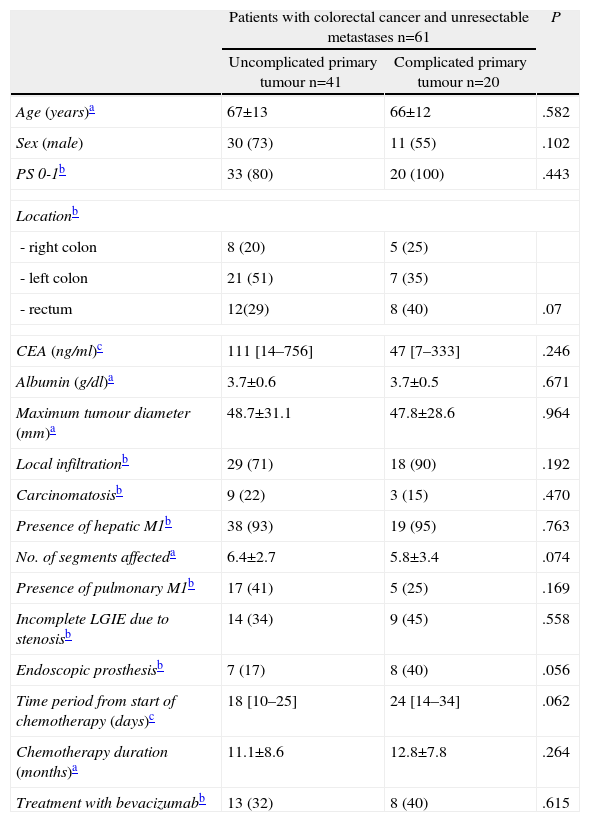
We did not find statistically significant differences in the characteristics of the patients or of the tumours, nor in the treatment administered, between those who presented a primary tumour complication and those who did not present one during the follow-up period (Table 2).
Characteristics of Patients With Unresectable Metastases With and Without Complications of the Primary Tumour.
| Patients with colorectal cancer and unresectable metastases n=61 | P | ||
| Uncomplicated primary tumour n=41 | Complicated primary tumour n=20 | ||
| Age (years)a | 67±13 | 66±12 | .582 |
| Sex (male) | 30 (73) | 11 (55) | .102 |
| PS 0-1b | 33 (80) | 20 (100) | .443 |
| Locationb | |||
| - right colon | 8 (20) | 5 (25) | |
| - left colon | 21 (51) | 7 (35) | |
| - rectum | 12(29) | 8 (40) | .07 |
| CEA (ng/ml)c | 111 [14–756] | 47 [7–333] | .246 |
| Albumin (g/dl)a | 3.7±0.6 | 3.7±0.5 | .671 |
| Maximum tumour diameter (mm)a | 48.7±31.1 | 47.8±28.6 | .964 |
| Local infiltrationb | 29 (71) | 18 (90) | .192 |
| Carcinomatosisb | 9 (22) | 3 (15) | .470 |
| Presence of hepatic M1b | 38 (93) | 19 (95) | .763 |
| No. of segments affecteda | 6.4±2.7 | 5.8±3.4 | .074 |
| Presence of pulmonary M1b | 17 (41) | 5 (25) | .169 |
| Incomplete LGIE due to stenosisb | 14 (34) | 9 (45) | .558 |
| Endoscopic prosthesisb | 7 (17) | 8 (40) | .056 |
| Time period from start of chemotherapy (days)c | 18 [10–25] | 24 [14–34] | .062 |
| Chemotherapy duration (months)a | 11.1±8.6 | 12.8±7.8 | .264 |
| Treatment with bevacizumabb | 13 (32) | 8 (40) | .615 |
CEA, carcinoembryonic antigen; LGIE, lower GI endoscopy; PS, performance status.
Conventional treatment of CRC with unresectable metastases consists of resection of the primary tumour followed by chemotherapy. Although the surgery does not have a curative intent, this treatment option continues to be used in a majority of patients; its principal goal is to avoid complications related to the primary tumour. In a recent study that reviewed more than 9000 cases, it was found that surgical resection of the primary tumour before initiating chemotherapy was performed in over 65% of patients with CRC in stage IV.17 Cook et al. also evaluated the use of primary tumour resection in these patients, utilising a national prospective database that includes information from 11 population registries including approximately 14% of the population of the United States.18 The authors observed that resection of the colon or rectum was performed in 66% of the 26754 patients diagnosed with CRC in stage IV over a period of 12 years.
Although resection of the primary tumour may be justified in patients with persistent bleeding or perforation, several studies published in recent years defend the advantages of treatment with chemotherapy without surgery in asymptomatic patients or those with symptoms that can be palliated with medical or endoscopic treatment.8–11 The main advantage lies in the possibility of initiating early systemic treatment and avoiding delay due to the surgical intervention. Initiation of chemotherapy is often delayed several weeks, especially when there are postoperative complications. For this reason, we progressively introduced this new treatment strategy 5 years ago in the CRC Functional Unit of the Hospital del Mar.
One of the possible drawbacks of this treatment approach is the onset of complications related to the unresected primary tumour, especially when patient survival increases with the use of new forms of chemotherapy. In this respect, several studies have shown that treatment with chemotherapy without surgery in patients with CRC and synchronous unresectable metastases is associated with a low rate of complications before death occurs as a result of disease progression.19–22 In a series of 24 patients in whom the primary neoplasm was left in situ, Sarela et al. observed only one case of complete obstruction that required emergency surgery and 3 progressive obstructions that were treated with an endoprosthesis or elective surgery.21 In a longer series with 82 patients treated with chemotherapy without resection of the primary tumour, Tebutt et al. observed that the most serious complications such as peritonitis or persistent bleeding occurred in less than 4% of patients, while intestinal obstruction affected 13.4%, in the majority of cases as a result of peritoneal progression.22 The conclusions of these first studies in favour of treatment with systemic chemotherapy without resection of the primary tumour have been criticised for including patients who were only administered 5-FU. However, later studies using the new chemotherapy regimens have shown that, despite the increase in survival, the rate of complications related to the primary tumour continues to be low.8,23 This is because the new systemic chemotherapy combinations have permitted better local control of the tumour, not only of the metastases.10 In a retrospective study, Poultsides et al. analysed the incidence of primary tumour complications that required surgery, radiotherapy or implantation of a prosthesis in a series of 233 consecutive patients. They found that 217 (89%) never required any direct procedure on the tumour to control symptoms, 16 (7%) required emergency surgery for haemorrhage or perforation, and 10 (4%) required radiotherapy or implantation of an endoscopic prosthesis. The authors concluded that the majority of patients in stage IV with unresectable synchronous metastases who are treated with the new forms of chemotherapy will never require palliative surgery, and that routine prophylactic colectomy is therefore not indicated.23 In a recent Cochrane Review, 7 uncontrolled studies were included which compared surgical treatment versus chemotherapy as sole treatment in patients in patients in unresectable stage IV CRC. Despite the absence of controlled studies, the authors concluded that resection does not reduce the risk of tumour-related complications.24
Although the number of patients is more limited, the results of our study also suggest that treatment with chemotherapy without surgery is a good option in the majority of patients with CRC and unresectable metastases. Only 6 patients in our series required surgery, and it was possible to perform it on a scheduled basis in 4 of them. In addition, surgical treatment morbidity was low and mortality was zero. However, 33% of patients presented complications of the primary tumour which required some form of treatment; this is a higher rate than in some of the previously mentioned series. Therefore, although routine prophylactic resection of the primary tumour may not be indicated, it would be desirable to identify those patients at higher risk of presenting complications in whom resection of the colon would be indicated before initiating chemotherapy. However, when we compared patients who presented a complication with those who did not, we did not observe differences either in the characteristics of the tumour or in the treatment administered which would allow us to identify these patients, although we should note that the complication rate in patients with a colonic stent was double that of the other patients.
Poultsides et al. were also unable to identify variables that would make it possible to predict the need of an emergency colectomy.23 The risk of [requiring] emergency surgery in the patients was not related to age, tumour location, number of metastases, CEA or serum albumin concentration.
One of the limitations of this study is the heterogeneity of the sample. We included patients with cancer of the colon and rectum, with hepatic, pulmonary or retroperitoneal metastases. Some of them received radiotherapy; in addition, there are 3 patients with neuroendocrine tumours. Still, we believe that the important consideration is that all of the patients have in common the fact that the primary tumour was left intact. The goal of the study was to analyse the possible complications of the unresected primary tumour, independently of the histologic type or of the location of the metastases. We believe that, in this way, the sample in this study is a clear reflection of the patients we will find in everyday practise and not an “experimental group.”
A controversial aspect in the use of chemotherapy without surgery as the initial treatment is the use of bevacizumab, since this has been associated with a 1%–2% incidence of gastrointestinal perforations in prospective clinical trials.25 However, in this study we also did not observe differences in the percentage of patients who were administered the monoclonal antibody when comparing patients with complicated and uncomplicated primary tumours. In the Poultsides et al. study, administration of bevacizumab in half the patients was not associated with a greater number of complications of the intact primary tumour.23 Recently, the first prospective phase II study was published whose principal objective was to determine the incidence of complications related to the primary tumour requiring surgical treatment or hospitalisation. Eighty-six patients with CRC and unresectable synchronous metastases who received 5-FU, oxaliplatin and bevacizumab were included; of these, 12 (14%) presented a major complication related to the primary tumours; 10 required emergency surgery and 2 died. As in previous studies, the authors concluded that the morbidity related to the intact primary tumour is acceptable and that surgery in asymptomatic patients can be avoided.26
Another controversial aspect regarding the best treatment option in these patients is the possible beneficial effect of primary tumour resection on survival. The results of some retrospective studies suggest that non-curative resection of an asymptomatic primary CRC can prolong survival compared to non-resection.18,27–31 Others, however, did not observe this beneficial effect on survival.19,32 In our study we only analysed the patients who received chemotherapy without surgery; we did not conduct a comparison with the few patients in whom the primary tumour was resected, given that there is a clear selection bias since these were patients with symptoms that required palliative surgery. Selection bias is precisely one of the most significant limitations of any of the previously mentioned comparative studies.18 A recent systematic review emphasised that none of the 21 studies included was controlled, and that selection bias and incomplete follow-up made interpretation of the results difficult.33 Randomised prospective studies are therefore needed which would allow confirmation of chemotherapy without surgery as the treatment of choice, and identification of those few patients in whom primary tumour resection would indeed be indicated. In this regard, the protocol of the German multicentre SYNCHRONOUS study, which compares global survival as well as the safety and impact on quality of life of both forms of treatment, has just been published.34
It is interesting to note that the intestinal obstruction rate was higher in those patients in whom an endoscopic stent was initially implanted, up to 53%. These are obviously not comparable groups, since the patients in whom stent placement was indicated probably presented more locally advanced and more stenosing malignancies. Nonetheless, these results – in agreement with the observations of other authors22 – show that endoscopic treatment should be performed only when the patient presents obstructive symptoms, not prophylactically, in order to prolong as much as possible the effective functioning time of the stent. We should also bear in mind that the rate of complications related to endoscopic palliation is not inconsiderable35,36 and that the risk of intestinal obstruction does not appear to be higher in stage IV CRC patients compared to earlier stages.37
In summary, the results of this study support the use of chemotherapy without colonic resection as treatment in the majority of CRC patients with unresectable synchronous metastases. However, although the percentage of patients who require emergency surgery is low, the total number of complications related to the primary tumour is not inconsiderable; studies are therefore needed which would make it possible to identify those patients for whom prophylactic colectomy would be indicated.
Conflict of InterestsThe authors declare that they have no conflict of interests.
We are grateful to Mercè Piracés, case manager at the Colorectal Cancer Functional Unit of the Hospital del Mar, for her valuable cooperation in identifying the patients and data collection.
Please cite this article as: Cáceres M, Pascual M, Alonso S, Montagut C, Gallén M, Courtier R, et al. Tratamiento del cáncer colorrectal con metástasis irresecables con quimioterapia sin resección del primario: análisis de las complicaciones relacionadas con el tumor. Cir Esp. 2014;92:30–37.
Given as an oral presentation at the XV Meeting of the Spanish Coloproctology Association, 4–6 May, 2011, Zaragoza.