For a long time, splenectomy was the method of choice, even for minor ruptures of the spleen, whether traumatic or iatrogenic. The discovery of “overwhelming post-splenectomy infection” (OPSI syndrome) prompted many surgeons to adopt a gentler approach to splenic parenchyma.1 The development of diagnostic tools such as ultrasound, computed tomography (CT), magnetic resonance imaging, new suture techniques using modern materials and hemostatic agents (fibrin glue), and the rapid development of laparoscopy have placed new technical demands on conservative splenic surgery.2,3
The article presents a case series of nine patients operated at the Institute of Pulmonary Diseases of Vojvodina. The preparation of the case series was approved by the Ethics Committee under the number: 71-XII /27. Since the internally cooled radiofrequency ablative single electrode (Cool-tip RFA Single Electrode Kit Covidien, USA®) proved to be a reliable hemostatic agent in the treatment of liver parenchyma, we used our experience in liver surgery and applied it in the preservation of the spleen. In all splenic surgeries, we used a high-frequency ablative single electrode, which has an internal cooling channel with an exposure tip of 2–3 cm and a length of the RF needle of 10–25 cm, and a RF system (Cool-tip RF Ablation System, Covidien, USA®).
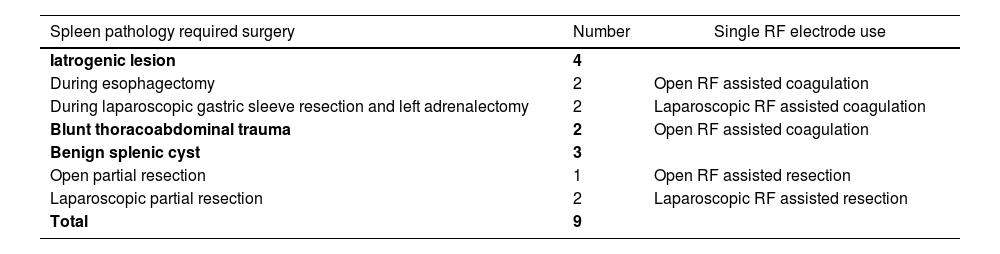
Of the indications, four patients had iatrogenic rupture of the spleen and two suffered traumatic rupture of the spleen in the setting of thoracoabdominal injury (Fig. 1). Three patients required surgery for a splenic cyst. Two of these patients underwent laparoscopic partial resection, while the third underwent open partial resection (Table 1). The spleen was not mobilized and a series of coagulation excisions were performed with the RF needle, piercing the skin and the anterior and anterolateral abdominal wall without using the trocar, but by choosing the shortest and most appropriate puncture position for the needle. The principle and plan behind the resection procedures was to use a series of coagulation-exsiccation necrosis with a RF needle, followed by incision of the splenic parenchyma with a knife or scissors without the use of other hemostatic agents. RF-assisted resection was performed and RF-assisted coagulation was achieved without rebleeding or reintervention.
Surgical pathology and use of radiofrequency single ablation electrode.
| Spleen pathology required surgery | Number | Single RF electrode use |
|---|---|---|
| Iatrogenic lesion | 4 | |
| During esophagectomy | 2 | Open RF assisted coagulation |
| During laparoscopic gastric sleeve resection and left adrenalectomy | 2 | Laparoscopic RF assisted coagulation |
| Blunt thoracoabdominal trauma | 2 | Open RF assisted coagulation |
| Benign splenic cyst | 3 | |
| Open partial resection | 1 | Open RF assisted resection |
| Laparoscopic partial resection | 2 | Laparoscopic RF assisted resection |
| Total | 9 |
Patients received antibiotic prophylaxis and low-molecular-weight heparin to prevent thromboembolism. All patients underwent postoperative examination of the spleen and upper abdomen, scintigraphy, and hematologic tests at CT. In all patients, scintigraphy confirmed the function of the spleen. Histopathological specimens were analyzed in all patients with splenic cysts. During the postoperative period, none of the patients received a vaccine against meningococcus, pneumococcus, or Haemophilus influenzae type B.
Splenectomy exposes the patient to a lifetime risk of post-splenectomy infections. This is particularly common in the pediatric population.4 For this reason, the techniques of conservative surgery of the spleen have been developed for all conditions that previously required splenectomy. The rapid development of laparoscopic surgery has contributed to the development of techniques for partial resection of the spleen whenever possible, especially for benign splenic cysts.5,6
Radiofrequency technology involving desiccation of the parenchyma (liver, spleen, lung) was used not only for ablation but also for resection by achieving a safe desiccation line that does not bleed after the incision. For our material, we used a RF needle with internal cooling, which causes local tissue destruction in the parenchyma with a ball of desiccation of approximately 2–3 cm, and a generator that produces waves of 200 W at 480 kHz. Desiccation is followed by complete hemostasis at the application site. Meanwhile, the tip of the RF needle remains cool and the tissue in which it is placed is warm due to Brownian motion and heat-induced protein denaturation.
Early work, particularly experimental procedures, involved the use of a bipolar resection device (Habib 4×), but its use is limited to open procedures and it is rarely used in laparoscopic procedures.7 A single RF needle is suitable for manipulation and positioning at the desired site on or within the splenic parenchyma even in open procedures. RFAC achieved by desiccation of the parenchyma has been adequate for all types of splenic lesions, including major ruptures. Laparoscopic partial resections of the spleen are now frequently performed for benign splenic disease, especially in children, but are still a difficult procedure mainly because of bleeding.8 Our results show that it is possible to safely cut the splenic parenchyma with a series of desiccations, while this devitalized parenchyma can be cut with ultrasonic scissors or even normal laparoscopic scissors. This type of application of RF technology to the spleen has no effect on the remaining, healthy portion of the spleen, as demonstrated by scintigraphy in all patients.
The use of this RF system is fast, simple and efficient. It is particularly suitable for laparoscopic partial resections of the spleen, as the cool tip of the needle can be inserted through the skin and muscles of the anterior abdominal wall at multiple sites in succession without causing damage. We recommend its use in surgical trauma centers performing complex laparoscopic procedures.
Conflicts of interestNone.
Please cite this article as: Putnik SS, Ilic MD. Usabilidad del electrodo de ablación simple de radiofrecuencia en la cirugía del bazo. Cir Esp. 2023.