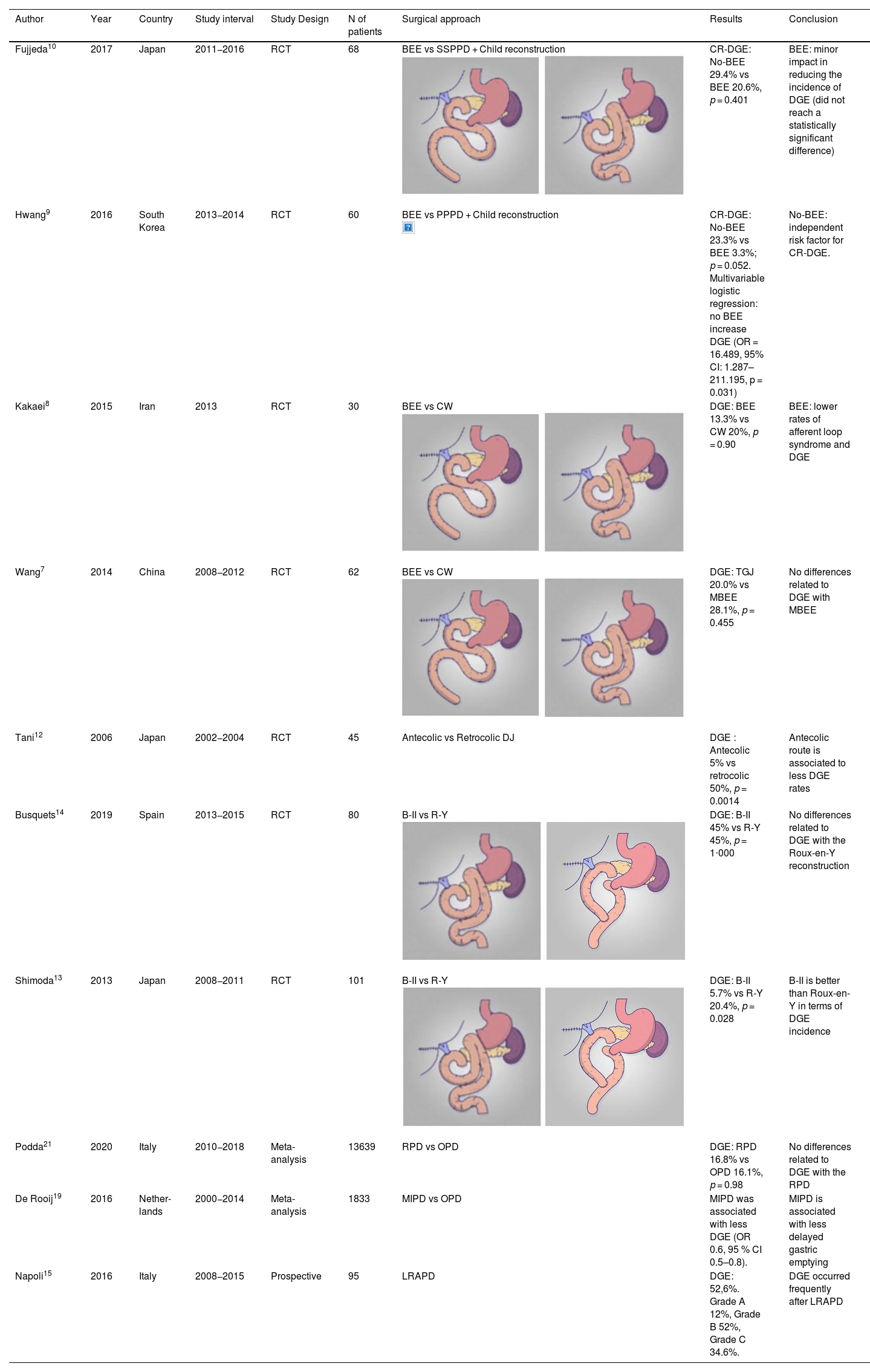
Partial pancreatoduodenectomy (PD) is the treatment of choice in pancreatic head tumours. Description of this technique includes antrectomy, although other variations have been proposed to save the pylorus, without clear advantages. The most widely used reconstruction in PD is Child reconstruction, in which the pancreatic-jejunal, hepatic-jejunal, and gastroenteric anastomoses are performed in a single loop with a Billroth II reconstruction. However, numerous modifications in the reconstruction of the tract to improve postoperative outcomes have been described. So, surgeons may be confused as to which is the best option for our patients. We reviewed published studies of different technical options for gastric anastomosis, and their impact on delayed gastric emptying (DGE) (Table 1).
Gastroenteric anastomoses.
| Author | Year | Country | Study interval | Study Design | N of patients | Surgical approach | Results | Conclusion |
|---|---|---|---|---|---|---|---|---|
| Fujjeda10 | 2017 | Japan | 2011−2016 | RCT | 68 | BEE vs SSPPD + Child reconstruction | CR-DGE: No-BEE 29.4% vs BEE 20.6%, p = 0.401 | BEE: minor impact in reducing the incidence of DGE (did not reach a statistically significant difference) |
| Hwang9 | 2016 | South Korea | 2013−2014 | RCT | 60 | BEE vs PPPD + Child reconstruction | CR-DGE: No-BEE 23.3% vs BEE 3.3%; p = 0.052. Multivariable logistic regression: no BEE increase DGE (OR = 16.489, 95% CI: 1.287–211.195, p = 0.031) | No-BEE: independent risk factor for CR-DGE. |
| Kakaei8 | 2015 | Iran | 2013 | RCT | 30 | BEE vs CW | DGE: BEE 13.3% vs CW 20%, p = 0.90 | BEE: lower rates of afferent loop syndrome and DGE |
| Wang7 | 2014 | China | 2008−2012 | RCT | 62 | BEE vs CW | DGE: TGJ 20.0% vs MBEE 28.1%, p = 0.455 | No differences related to DGE with MBEE |
| Tani12 | 2006 | Japan | 2002−2004 | RCT | 45 | Antecolic vs Retrocolic DJ | DGE : Antecolic 5% vs retrocolic 50%, p = 0.0014 | Antecolic route is associated to less DGE rates |
| Busquets14 | 2019 | Spain | 2013−2015 | RCT | 80 | B-II vs R-Y | DGE: B-II 45% vs R-Y 45%, p = 1⋅000 | No differences related to DGE with the Roux-en-Y reconstruction |
| Shimoda13 | 2013 | Japan | 2008−2011 | RCT | 101 | B-II vs R-Y | DGE: B-II 5.7% vs R-Y 20.4%, p = 0.028 | B-II is better than Roux-en-Y in terms of DGE incidence |
| Podda21 | 2020 | Italy | 2010−2018 | Meta-analysis | 13639 | RPD vs OPD | DGE: RPD 16.8% vs OPD 16.1%, p = 0.98 | No differences related to DGE with the RPD |
| De Rooij19 | 2016 | Nether-lands | 2000−2014 | Meta-analysis | 1833 | MIPD vs OPD | MIPD was associated with less DGE (OR 0.6, 95 % CI 0.5–0.8). | MIPD is associated with less delayed gastric emptying |
| Napoli15 | 2016 | Italy | 2008−2015 | Prospective | 95 | LRAPD | DGE: 52,6%. Grade A 12%, Grade B 52%, Grade C 34.6%. | DGE occurred frequently after LRAPD |
RCT: randomized clinical trial, BEE: Braun entero-enterostomy, SSPPD: subtotal stomach preserving pancreatoduodenectomy, PPPD: pylorus-preservation pacreatoduodenectomy, DJ: duodeno-jejunostomy, B-II: Billroth II, RPD: robotic pancreatoduodenectomy, OPD: open pancreatodudenectomy, MIPD: Minimally invasive pancreatoduodenectomy, PD: pancreatoduodenectomy, DGE: delayed gastric emptying, CW: Classic Whipple, PR: pylorus-resection, PP: pylorus-preservation, CR-DGE: clinically relevant DGE, OR: Odds ratio, CI: confidence interval, TGJ: traditional gastro-yeyunostomy, MBEE: Modified braun entero-enterostomy, R-Y : Roux-en-Y, LRAPD: Laparoscopic robotic assisted pancratoduodenectomy.
Whipple1 described the technique of resecting the pancreatic head by removing the gastric cavity. Later, Traverso2 published his variation to spare removal of the den and the pylorus. Some randomized controlled trials (RCTs) have shown that pylorus-preserving pancreatoduodenectomy (PPPD) provides benefits compared to Whipple pancreatoduodenectomy, with better nutritional and endocrine recovery, and better postoperative quality of life. However, other studies showed increased DGE in patients undergoing pylorus preserving pancreatoduodenectomy. In recent decades, several RCTs and metanalyses have found similar results for the two techniques. As may be seen, it remains unclear which of the two is better with respect to DGE. Furthermore, several RCTs have been published comparing pyloric ring preservation versus its resection, with contradictory conclusions. The latest meta-analyses, including 24 RCTs and 2526 patients, suggest that pyloric resection followed by Braun’s omega was the best reconstruction in terms of DGE3.
Termino-terminal gastroenteric anastomoses (Billroth I)In 1995, Ueno4 proposed reconstruction of the tract in a single loop starting with the termino-terminal gastric suture, in Billroth I, followed by pancreatic suture and, finally, biliary suture. In their article, they evaluated patients after PPPD and reconstruction with Billroth I with end-to-side duodenojejunostomy, and did not observe any cases of DGE. Subsequently, a study published by Goei5 in 2001 compared the incidence of DGE with Billroth I or Billroth II reconstruction after PPPD in 174 patients. In this retrospective study, a higher incidence of DGE after Billroth I reconstruction was found (76 % after Billroth I vs 32% after Billroth II (p < 0.05). To date, there is scarce evidence that Billroth I is a good option for entero-enteric anastomosis.
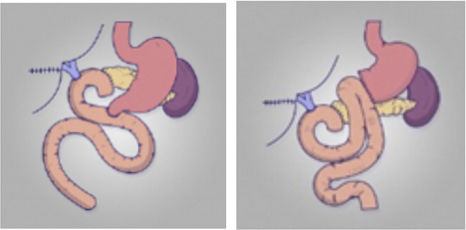
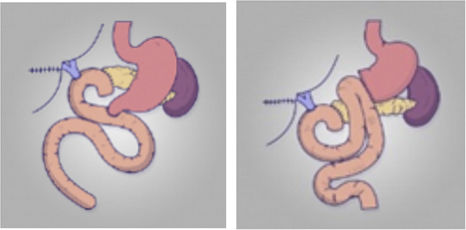
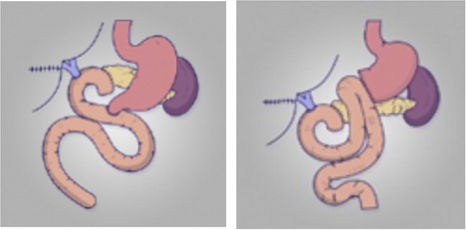
Braun omega enteroenterostomyIn 2015, Watanabe6 compared the incidence of DGE after adding a Braun enteroenterostomy (BEE) to the gastroenteric suture after PPPD. In his retrospective study including 185 patients, the group undergoing BEE had a lower incidence of DGE (4% of patients with BEE and 21% of those without BEE, p < 0.01). In fact, BEE was the only independent factor associated with DGE in the multivariate analysis (OR 5.04, p < 0.01). To date, four RCT studies have been published in this regard. The two older ones argue for the use of Braun omega, with less alkaline reflux or less DGE7,8.However, the two most recent studies show that Braun's omega showed a similar DGE9,10 (Table 1).
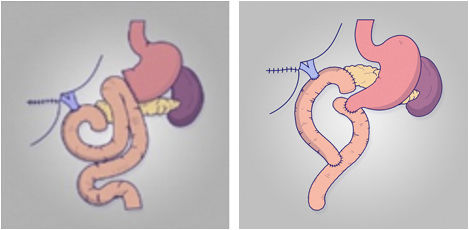
Ascension of the jejunal loop and relation of the gastric suture to the colonAs a technical detail, Park's group in Korea demonstrated in 2003 that the passage of the jejunal loop via the retro-mesenteric route was slower than the mesenteric passage of the jejunal loop11. The authors suggested that the oedema of the jejunal loop at its retro-mesenteric passage could lead to worse gastric swelling. Recently, several groups have shown that antecolic gastroenteroanastomosis is useful in reducing DGE compared to retrocolic reconstruction, and it has become the technique used worldwide, either with gastric sparing or with antrectomy. The fact that antecolic reconstruction favours vertical positioning of the stomach may explain the improvement in stomach wall displacement. In the RCT published by Tani12, 40 patients were randomized to either retrocolic or antecolic reconstruction of the duodenojejunostomy after PPPD. DGE occurred in 5% of patients with the antecolic route for duodenojejunostomy versus 50% with the retrocolic route (P = 0.0014), showing that antecolic reconstruction decreases postoperative morbidity and length of hospital stay by decreasing DGE.
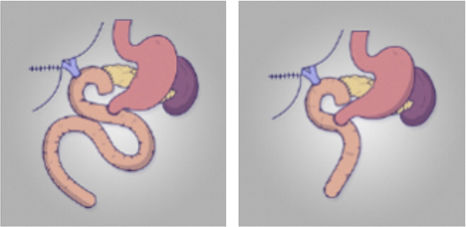
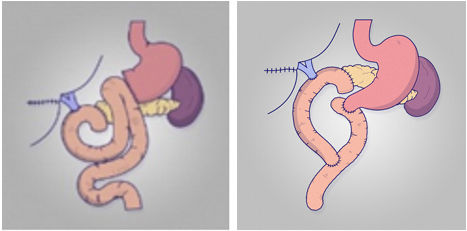
Roux-en-Y gastroenteroanastomosis in partial pancreatoduodenectomySeveral authors have proposed performing a Roux-en-Y gastroenteroanastomosis with partial pancreatoduodenectomy to improve postoperative outcomes. In 2013 Shimoda13 published a randomised study comparing Roux-en-Y reconstruction with Billroth II reconstruction in 101 patients. The group demonstrated a higher rate of DGE and longer hospital stay in the Roux-en-Y group (5.7 vs 20.4%, p = 0.028 and 31.6 ± 15 days vs 41.4 ± 20.5 days, p = 0.037). Recently, our group also published a randomized study with 80 patients that failed to demonstrate differences between Billroth II and Roux-en-Y gastroenteroanastomosis14.
Minimally invasive pancreatoduodenectomy (MIPD)Several studies indicate a lower DGE in MIPD compared to open pancreatoduodenectomy (OPD) with, however, some controversy. The Pisa group published a review of 96 robotic PDs in 2016, showing a DGE rate of 52.6%15. Later, Wang16 published a propensity-score study with 87 cases of robotic pancreaticoduodenectomy (RPD) and 87 cases of OPD, and less DGE was noted in the RPD (3.4 vs 13.8, p = 0.015). In a recent study17 including 304 RPD and 172 OPD, DGE was 3.5% in the RPD group and 13.6% in the OPD (p < 0.001). Finally, Oosten18 found RPD to be associated with a lower incidence of DGE (9.4%) compared to OPD (23.5%; P = 0.006).
The meta-analyses are also contradictory. So, De Rooij19 compared MIPD and OPD, showing that DGE occurred less frequently in MIPD (OR 0.6, 95%CI 0.5–0.8). Contradictorily, Peng20 in 2017 analysed 5 studies without finding differences in terms of DGE (RR = 0.52; 95%CI 0.26–1.04; P = 0.06). Similarly, Podda21 compared RPD with laparotomic PD based on 18 studies involving 13,639 patients and found similar rates of DGE (16.8% vs 16.1%; OR 1.00, 95% CI 0.74–1.34; P = 0.74) (Table 1).
In conclusion, there remain many technical options for gastric reconstruction in pancreatoduodenectomy. Child's reconstruction is the most widespread technique, although patients continue to suffer from delayed gastric emptying. MIPD could provide better results with respect to the DGE.
The authors would like to thank the IDIBELL Foundation and the CERCAProgramme/Generalitat de Catalunya for the institutional support provided.