Recent data from the 2008 Spanish Growth Study show that the rate of overweight children, adolescents and young adults from the ages of 4–24 has increased by approximately 10% in the last twenty years. At present, it is estimated that 20% and 15% of male and female children and young adolescents respectively are overweight and that 5% of this population and in this age range are obese.1–5
In this context, our Paediatric Endocrinology Department has pioneered the design and development of programmes aimed at the prevention and integral treatment of childhood and youth obesity (“Niñ@s y adolescent@s en movimiento”).6
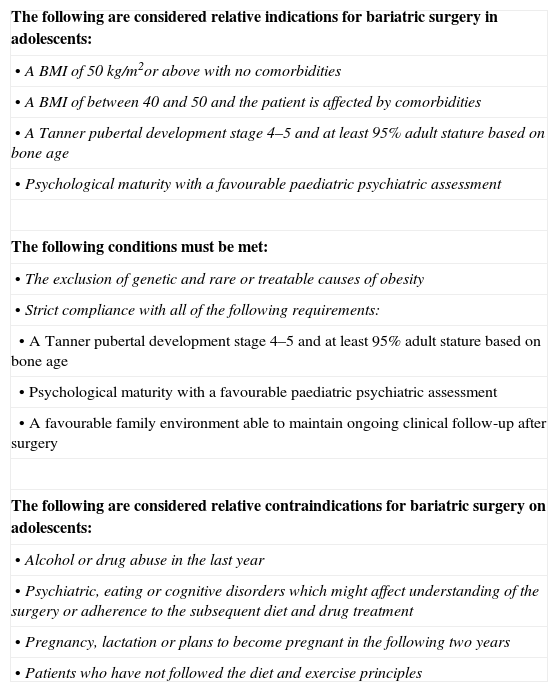
Initially, we decided to start our activity by assessing the efficacy and safety of endoscopic intra-gastric balloon placement in morbidly obese adolescents as this is a minimally invasive method which is reversible and does not alter the absorption or digestion of nutrients and which could reinforce the behavioural therapy and lifestyle changes which these patients had already started.7 Our preliminary experience with this technique is limited to eight patients between 13.9 and 17.9 years of age (five females and three males) with an average BMI of 46.2±6.4, all of them presenting one or more severe comorbidities. The results obtained 18–24 months post IGB explant show that a group of four patients had maintained the weight loss achieved (BMI-SD loss of −11.0±3.7) whereas the remainder had regained or slightly increased in weight prior to the IGB implant (BMI-SD of +2.3±2.4). The partial effectiveness obtained with this technique was a determining factor in forming and developing a programme of “bariatric surgery for adolescents”. Table 1 shows the inclusion criteria and relative contraindications adopted.
Inclusion Criteria and Contraindications for the Obesity Surgery Programme for Adolescents.
| The following are considered relative indications for bariatric surgery in adolescents: |
| •A BMI of 50kg/m2or above with no comorbidities |
| •A BMI of between 40 and 50 and the patient is affected by comorbidities |
| •A Tanner pubertal development stage 4–5 and at least 95% adult stature based on bone age |
| •Psychological maturity with a favourable paediatric psychiatric assessment |
| The following conditions must be met: |
| •The exclusion of genetic and rare or treatable causes of obesity |
| •Strict compliance with all of the following requirements: |
| •A Tanner pubertal development stage 4–5 and at least 95% adult stature based on bone age |
| •Psychological maturity with a favourable paediatric psychiatric assessment |
| •A favourable family environment able to maintain ongoing clinical follow-up after surgery |
| The following are considered relative contraindications for bariatric surgery on adolescents: |
| •Alcohol or drug abuse in the last year |
| •Psychiatric, eating or cognitive disorders which might affect understanding of the surgery or adherence to the subsequent diet and drug treatment |
| •Pregnancy, lactation or plans to become pregnant in the following two years |
| •Patients who have not followed the diet and exercise principles |
This programme is based on the Bariatric Surgery Unit's experience and good results after more than 600 operations and incorporating the DaVinci robot (Intuitive Surgical, Sun Valley, CA, USA), which has already been used in seventy operations. The technique of robotic tubular gastroplasty (RTG) was selected, which has been shown to be effective for weight loss and in treating associated comorbidities, and leaving open the possibility of rescue surgery.8,9
The usual thorough preoperative study, which was normal, was performed in all cases. After positive assessment by the Department of Child and Adolescent Psychiatry, three morbidly obese adolescents of fifteen, sixteen and seventeen years of age with a BMI of 48kg/m2, 47kg/m2, and 42kg/m2 respectively, underwent surgery.
The surgical technique follows the same principles as the conventional technique. The patient is placed supine, legs apart and in a reverse Trendelenburg position. A pneumo-peritoneum of 15mmHg is created using a Veress needle. Five trocars are used (three 12mm trocars, an auxiliary 11mm trocar and an 8mm DaVinci trocar). The assistant attaches the robot's arms to the trocars (docking). The surgeon frees the major gastric curvature using an ultrasonic scalpel to perform a vertical gastrectomy with endostaples at 5cm from the pylorus and guided by a 36 Fr probe. The surgical specimen is extracted and the staple line is reinforced with a continuous 2/0 polypropylene suture. A low pressure suction drain is placed after leak testing with methylene blue. The procedure concludes with a check of the trocars and infiltration with local anaesthetic.
Clinical Case 1This first clinical case was a 17-year-old adolescent male, weighing 130kg with a BMI of 42kg/m2, who presented no obesity-related comorbidities. Once he was included in the programme, the RGT was performed after his eighteenth birthday. He was discharged on the fourth day, after a post-operative period without incident. Three months after the operation, he weighs 104kg and his BMI is 33kg/m2.
Clinical Case 2The second case was a 15-year-old adolescent male, with a history of meningitis in infancy, weighing 160kg with a BMI of 48kg/m2. Comorbidities: (a) glucose intolerance requiring medical treatment with metformin, (b) medically treated arterial hypertension. He had been taking part in the “Adolescent@s en movimiento” programme. An intra-gastric balloon had been placed at the age of fourteen when he weighed 145kg; this achieved a weight loss of 12% in six months. When this was removed he regained the initial weight and continued to gain weight. RGT was performed without incident and he was discharged on the fourth postoperative day. Two months after the operation he weighs 120kg and his BMI is 38kg/m2. His blood pressure and glycaemia have become normal without the need for treatment. Routine checks show that his adjustment to school has greatly improved.
Clinical Case 3This third case was a 16-year-old adolescent male who was included in the “Adolescent@s en movimiento” programme during prepuberty. Associated with his morbid obesity were: (a) glucose intolerance treated with metformin, (b) obstructive sleep apnoea syndrome treated with CPAP. RTG was performed when he weighed 135kg with a BMI of 47kg/m2. He was also discharged four days after an incident-free postoperative period. Two months after surgery, he weighs 105kg and his BMI is 38kg/m2. He no longer needs night-time CPAP or metformin.
All the patients met the inclusion criteria and there were no post-operative complications. Average follow-up was at five months with expected results and no complications to date.
The programme which has been consolidated and accredited in adults has enabled the safe and effective implementation of the bariatric surgery programme for adolescents, with new technologies under evaluation. The availability of surgeons who are experts in obesity and a multidisciplinary team is required in order to ensure the strict selection of candidates and appropriate long-term follow-up.10
The authors wish to thank, amongst others, the following colleagues who made the development of the Obesity Surgery Programme for Adolescents possible: Dr. Carrascosa, Dr. Martínez-Ibañez, Dr. Lloret, Dr. Bueno, Dr. González and Dr. Caubet, Dr. Roca, Dr. Montferrer, Dr. Vázquez, Dr. Marhuenda, Dr. Guillén, Dr. Mesa, Sra. Gromaz, Dr. Gastaminza, Dr. Redecillas.
Please cite this article as: Vilallonga R, Yeste D, Lecube A, Armengol M, Fort JM. Programa de cirugía bariátrica en adolescentes. Resultados preliminares. Cir Esp. 2013;91:685–687.