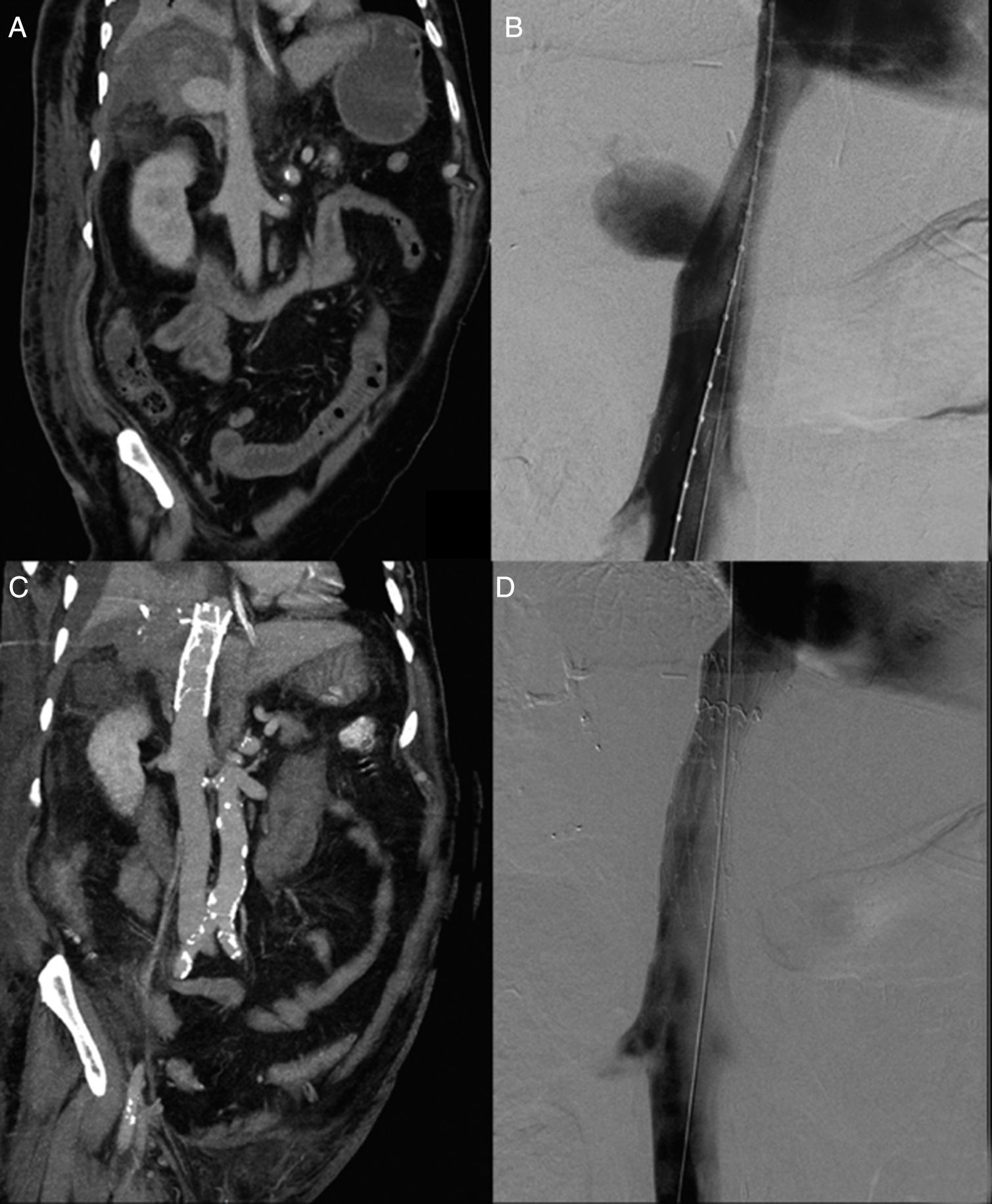
A 65-year-old man was admitted to the emergency department for being in septic shock. Ten days ago he had undergone right extended hepatectomy due to cholangiocarcinoma. Initial laboratory results revealed reduced hematocrit blood level, reduced prothrombin time, platelets, and fibrinogen, with increased aPTT, and metabolic acidosis. CT angiography showed a subhepatic IVC pseudoaneurysm with subphrenic spontaneuos high attenuated free fluid (Fig. 1A). Since the patient condition was inappropriate for surgery, an endovascular solution was chosen.
(A) CT angiography, portal phase, coronal plane. Subhepatic IVC pseudoaneurysm is seen and free liquid with high attenuation, suggestive of rupture. (B) Cavogram. Subhepatic IVC pseudoaneurysm is confirmed. (C) CT angiography, portal phase, coronal plane. Stent patency is seen. (D) Cavogram. Stent patency is confirmed.
Under general anesthesia, the common femoral vein was punctured, an 8 fr introducer was placed, and a pigtail catheter was advanced until right atrium. Cavogram confirmed CT angiograpgy findings (Fig. 1B). We placed a cuff vela (ENDOLOGIX INC, 11 Studebaker, Irvine, CA 92618, United States) that excluded the pseudoaneurysm from the circulation without compromising renal and suprahepatics veins. Ten days later CT angiography (Fig. 1C) and cavogram (Fig. 1D) showed stent patency.
Inferior vena cava (IVC) pseudoaneurysm is a hematoma, with disruption of one or more vessel layers, that has high rate of rupture. It can be caused by different injuries (traumatic, iatrogenic injury, etc.) associated or not with inflammatory processess, such as infection. Patients can be completely asymptomatic or present with life-threatening conditions.1
Surgical therapies (patch repair, vein grafts, atriocaval shunting, etc.) are definitive treatments for stable patients. Like in our patient, to achieve hemostasis in retrohepatic or subhepatic IVC injuries require extensive organs dissection, worsening the patient condition. That is the reason why it has been estimated mortality up to 70% in such conditions. Endovascular approach should be consider in either stable or unstable hemodinamically patients, since it can be done with relative ease and speed, causing minimal additional sorrounding tissue injury.1,2
De Naeyer reported the use of a talent endoluminal stent-graft to treat infrarenal IVC perforation due to a lumbar vertebral fusion,3 Erzurum et al. reported the use of an aneurix aortic extension cuff in a retrohepatic IVC injury during a retroperitoneal leiomyosarcoma resection,4 and Watarida et al. reported the use of a fenestrated stent-graft for a traumatic juxtahepatic IVC injury.5
Since potentiable risks are associated with the use of these devices in IVC (erosion or even rupture of it, thrombosis and probable pulmonary embolization, etc.) close follow-up of these patients is strongly advised.2
Particularly in hemodinamically unstable patients with injury of retrohepatic or subhepatic IVC injury, endovascular approach should be consider, since it can be performed with relatively speed and ease, offering an alternative solution for such life-threating condition.
Please cite this article as: Causa Andrieu PI, Gomez N, Rabellino MJ, Pejokl J, Garcia-Monaco R. Tratamiento no quirúrgico de seudoaneurisma de la vena cava inferior poshepatectomía. Cir Esp. 2017;95:298–299.