Acute appendicitis (AA) is the most frequent cause of urgent abdominal surgery in our setting and represents around 60% of all cases of acute abdomen requiring surgery.1 AA secondary to obstruction of the lumen of the appendix by a foreign body is a rare condition that must be considered in certain situations.2 Episodes of acute appendicitis secondary to ingested shotgun pellets used in hunting small game are rarely reported in the literature but should be considered in certain cases.
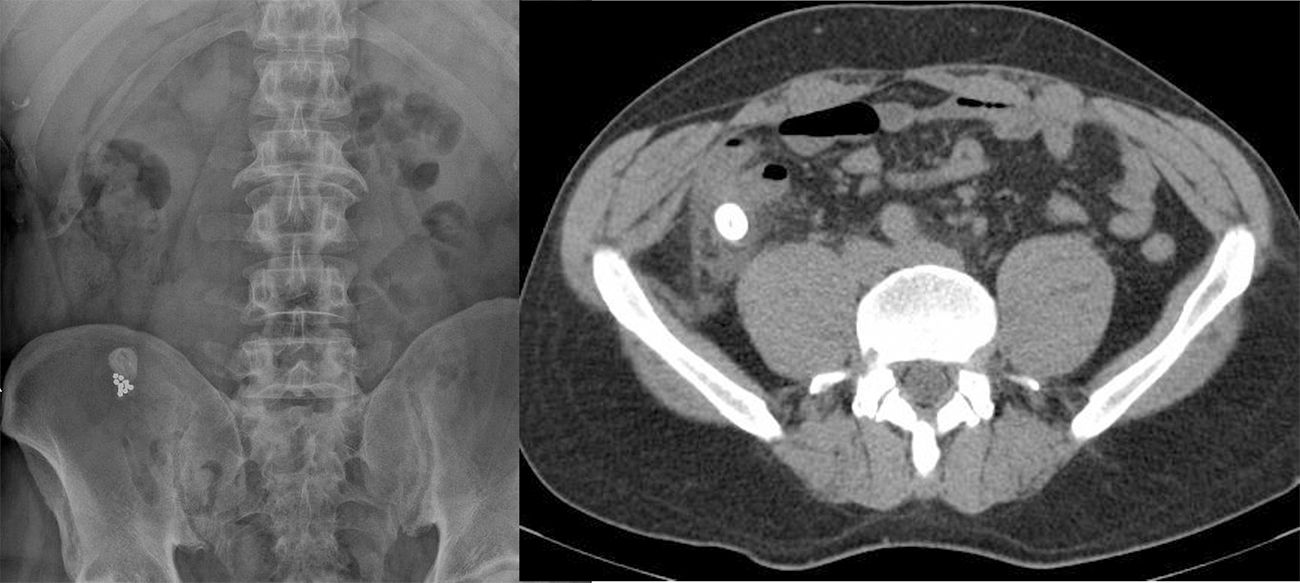
We present the case of a 45-year-old patient who resided in a rural area and whose family hunted for sport, so he had habitually eaten small game (partridge and rabbit) since childhood. He came to the Emergency Room with abdominal pain that had been developing over the previous 72h in the right iliac fossa (RIF), suggestive of acute appendicitis. Upon physical examination, pain was detected on palpation in the RIF, with muscle guarding and signs of peritoneal irritation. Lab work-up showed 17600 leukocytes with left shift. Imaging studies found evidence of acute appendicitis with obstruction of the appendiceal lumen by a foreign body measuring 1.7cm, as well as other smaller-sized bodies located distally (Fig. 1).
The patient was taken to surgery immediately, and laparoscopy discovered gangrenous AA. When the surgical specimen was opened (Fig. 2), the lumen was obstructed by a 1.7cm compaction of pellets, which had triggered the appendiceal process, as well as other loose pellets located distally. The patient evolved favorably and was discharged on the 2nd postoperative day. Later radiography studies showed no persistence of any foreign bodies. The anatomic pathology study confirmed the diagnosis of gangrenous AA secondary to obstruction by a foreign body.
Obstruction of the lumen of the appendix is the most common etiology in the development of AA, usually due to fecal material, adhesions or lymphoid hyperplasia. AA is rarely caused by a foreign body.3 Ingestion of foreign bodies is frequent in certain patient groups (children, patients with mental disorders or self-harm attempts). Most of these elements are eliminated with the feces, and only 1% of these foreign bodies require surgical intervention, usually due to bleeding or intestinal perforation.4 Foreign bodies located in the lumen of the appendix are very uncommon (<0.0005%), and the most frequently described materials include: seeds, surgical staples and needles, prosthetic material, screws or, less frequently, birdshot.5,6 Even if the lumen of the appendix becomes obstructed by shotgun pellets or other foreign bodies, the development of AA is very rare.
The first description of this pathology was in 1736 by Claudius Amyand, who treated an 11-year-old boy with acute appendicitis and perforation of the appendix secondary to the impaction of a “pin”.7 A clinical follow-up study has been conducted of patients with radiological evidence of appendicular foreign bodies, and less than 1% of patients developed acute appendicitis in more than 10 years of follow-up.8
There are several mechanisms that could trigger AA. The first would be obstruction of the intestinal lumen by the foreign body, with subsequent vascular congestion, ischemia, bacterial translocation and infection. Other mechanisms could be direct perforation of the appendix by a sharp object and the resulting infection, or the generation of a fecalith around the foreign body with the consequent obstruction of the appendix.9 In our case, the AA was triggered by the compaction of several pellets over a long period of time, forming a lead foreign body measuring 1.7cm in diameter that was the cause of obstruction of the appendiceal lumen.
Despite the exceptional nature of this condition, several groups advocate close monitoring of these patients and even endoscopic extraction or prophylactic appendectomy in selected patients in order to avoid the morbidity associated with the development of AA.8 Isolated cases have been reported in which the occupation of the appendiceal lumen and other intestinal areas by lead pellets has led to elevated blood levels of this metal and the appearance of symptoms that can range from nonspecific symptoms to severe encephalopathy.10 For all these reasons, it would seem reasonable to indicate scheduled laparoscopic appendectomy in patients who are symptomatic or at high risk of complications or toxicity; meanwhile a conservative approach is indicated in asymptomatic patients with small foreign bodies, although there is no firm consensus in the scientific community.
The clinical diagnosis and surgical management of emergencies in these patients does not differ from other patients with AA. However, this situation was suspected given the patient's background (in Spain, small game hunting with birdshot is still a frequent practice) as well as the characteristic radiopaque image on abdominal radiograph (Fig. 1). Early identification of these patients will allow us to either manage the patient conservatively, attempt endoscopic extraction of the foreign body or perform a scheduled appendectomy with minimal morbidity and mortality.
Please cite this article as: Abellán I, Ibañez N, Vergel R, Rondeau MB, González P. Apendicitis aguda causada por cuerpo extraño. Cir Esp. 2019;97:347–348.