Conservative breast cancer surgery requires an exact knowledge on the impact that local resection may have on the cosmetic result, and for this reason, the characteristics of each breast region must be taken into account. The segmentation theory helps to predict the consequences of local resection in each breast segment and, at the same time, optimise the choice of the best procedure for their prevention. Therefore, surgical planning based on segmentation of the breast would help us achieve a current objective of breast oncological surgery: a surgery adapted to the breast and the tumour. This article describes the different breast segments, their resources and limits for remodelling, and the best technical options to prevent deformities in each one of them.
La cirugía conservadora del cáncer de mama precisa de un conocimiento sobre la repercusión que la resección local producirá en el resultado cosmético y para ello es necesario tener en cuenta las características de cada región mamaria. La teoría de la segmentación permite predecir las consecuencias de la reseccio¿n local en cada segmento mamario y, al mismo tiempo, optimiza la selección del mejor procedimiento para su prevención. De esta forma, una planificación quirúrgica basada en la segmentación de la mama nos permitirá alcanzar el objetivo actual de la cirugía oncológica de la mama: una cirugía adaptada a la mama y al tumor. Este artículo describe los diferentes segmentos de la mama, sus recursos y límites para la remodelación y las mejores opciones técnicas para la prevención de deformidades en cada uno de ellos.
The use of oncoplastic procedures in the treatment of breast cancer has led to an increasing sensitivity towards deformities and asymmetry to the point where the cosmetic result is now considered an integral part of the oncologic procedure, to preserve physical harmony and the psychological wellbeing of women.1 This experience has led to identifying critical areas for the occurrence of deformities. Furthermore, it has also shown that the breast is not the homogeneous organ that was once believed; but is instead a heterogeneous organ with each area playing a different role in women's body image and reacting differently to local resection. This realisation has resulted in a different anatomical division of the breast being done to identify critical areas for breast resection and to improve the cosmetic results of conservative surgery.
Tumour size and location and breast volume are the basic considerations for the indication for conservative surgery in women with breast cancer. Although tumour size can be altered by neoadjuvant therapy, this is not the case with anatomical variables of the breast, which remains unchanged during chemotherapy. Of these two anatomical variables, breast size has a generic influence on the indication for conservative surgery, as it must ensure an appropriate ratio between the sizes of the tumour and breast. On the other hand, the choice of procedure is significantly influenced by tumour location, as this affects the cosmetic impact of resection on the contour of the breast. This relationship between tumour location and cosmetic outcome after resection is based on the following:
- -
Glandular tissue is not distributed evenly across the breast, which means that some areas are more difficult to be re-modelled and are more vulnerable to deformity.
- -
The breast contour is heterogeneous in its response to local resection, which means that some areas, such as the lower pole, are at high risk of deformity and will suffer regardless of the volume of resection.
- -
The nipple-areola complex (NAC) is an anatomical area sensitive to deformity or mobilisation after resection nearby.
- -
There are areas of the breast related to the social life of women, which are areas more prone to public exposure where a scar or deformity must be prevented.
Classification of breast regions based on division into quadrants is insufficient to meet these new needs of breast cancer surgery. The cosmetic outcome, while not the main objective of breast conservation is, increasingly, a basic requirement in the quality of the procedure. Therefore, a new classification, based on the cosmetic impact of resection on the different areas of the breast, is needed in order to achieve 2 objectives: to prevent deformities which are typical for a particular breast area, and to select the best surgical procedure for this.2–5
The purpose of this article is to propose a new breast division, based on segmentation into regions and their specific behaviour towards surgical resection.
Breast SegmentationA detailed observation of deformities in conservative surgery shows that the breast has a variable response to resection according to the anatomical area acted upon. The variability in morphology and glandular distribution is responsible for the cosmetic differences seen after local resection without remodelling. The aim of breast segmentation is to make full use of the different resources available for remodelling that each area has and to minimise the visual impact of the scar. This model can predict adverse outcomes (oncological and cosmetic) after local excision in a given segment, the local resources for remodelling and, in particular, the conservative management limits in a case. Thus, once the limitations for local excision in a segment are identified, the procedure best suited for tumour resection, prevention of local deformities, and minimal scar impact can be selected.
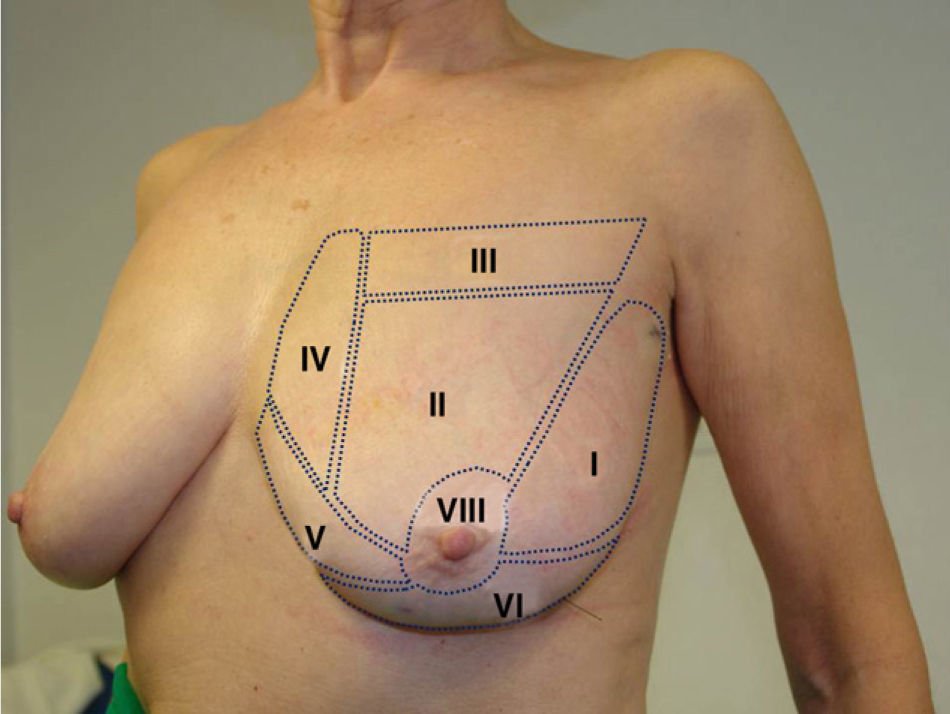
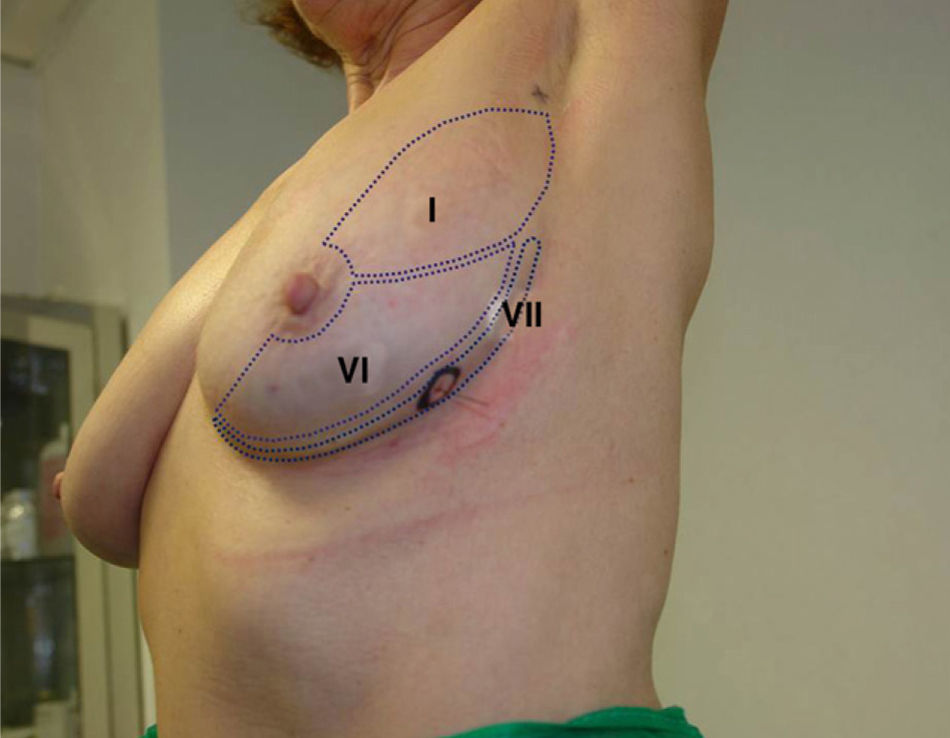
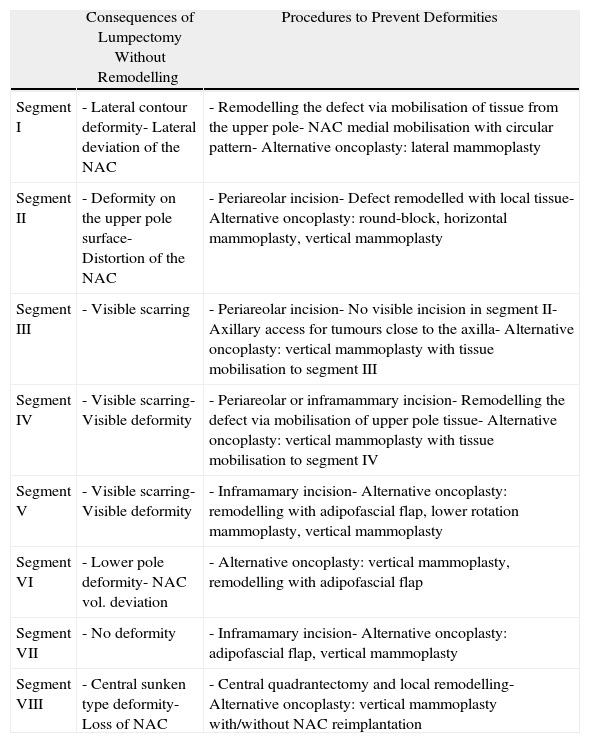
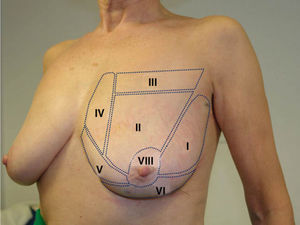
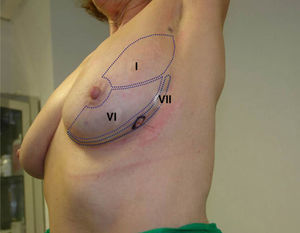
The female breast can be divided into 8 segments as follows: the lateral segment (segment I), upper pole (segments II, III and IV), lower pole (segments V, VI and VII) and the central region (segment VIII), see Figs. 1 and 2. Their identification and size depend on two anatomic variables: the size and ptosis. A larger breast size improves identification and visualisation of these segments, while, as breast size reduces, overlapping segments hinder the choice of the surgical procedure and the adverse effects of each segment must be added. This explains why a small breast is more difficult for conservation and is more likely to display cosmetic deterioration. Meanwhile, breast ptosis expands the segments, especially upper pole segments where there is an increase in segments III–IV and a decrease in segment II. Breast reduction techniques contribute to a reconfiguration of the upper pole, improving the ratio of segments II–III. Table 1 shows the characteristic deformities for each segment and procedures to prevent them.
Alternative Techniques for the Prevention of Breast Deformities in Each Segment.
| Consequences of Lumpectomy Without Remodelling | Procedures to Prevent Deformities | |
| Segment I | - Lateral contour deformity- Lateral deviation of the NAC | - Remodelling the defect via mobilisation of tissue from the upper pole- NAC medial mobilisation with circular pattern- Alternative oncoplasty: lateral mammoplasty |
| Segment II | - Deformity on the upper pole surface- Distortion of the NAC | - Periareolar incision- Defect remodelled with local tissue- Alternative oncoplasty: round-block, horizontal mammoplasty, vertical mammoplasty |
| Segment III | - Visible scarring | - Periareolar incision- No visible incision in segment II- Axillary access for tumours close to the axilla- Alternative oncoplasty: vertical mammoplasty with tissue mobilisation to segment III |
| Segment IV | - Visible scarring- Visible deformity | - Periareolar or inframammary incision- Remodelling the defect via mobilisation of upper pole tissue- Alternative oncoplasty: vertical mammoplasty with tissue mobilisation to segment IV |
| Segment V | - Visible scarring- Visible deformity | - Inframamary incision- Alternative oncoplasty: remodelling with adipofascial flap, lower rotation mammoplasty, vertical mammoplasty |
| Segment VI | - Lower pole deformity- NAC vol. deviation | - Alternative oncoplasty: vertical mammoplasty, remodelling with adipofascial flap |
| Segment VII | - No deformity | - Inframamary incision- Alternative oncoplasty: adipofascial flap, vertical mammoplasty |
| Segment VIII | - Central sunken type deformity- Loss of NAC | - Central quadrantectomy and local remodelling- Alternative oncoplasty: vertical mammoplasty with/without NAC reimplantation |
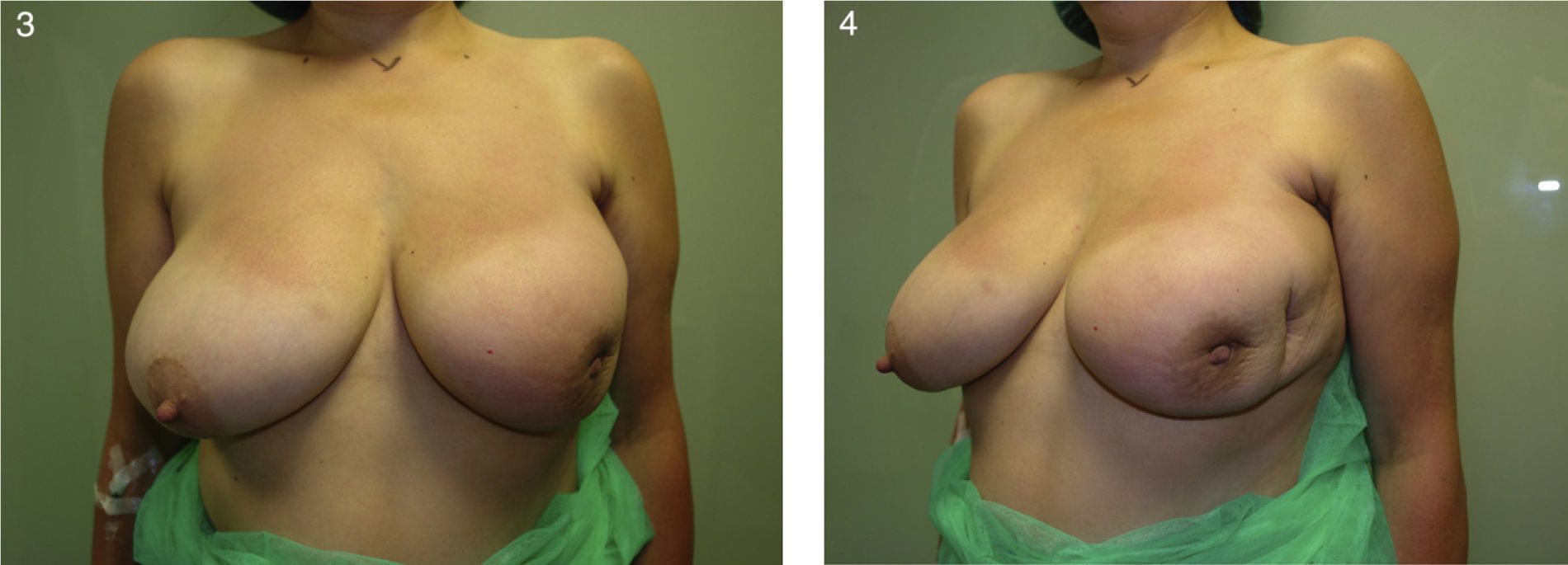
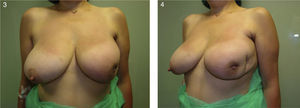
The lateral segment is the most frequent area for tumour resection in clinical practice, as it contains a high proportion of the breast parenchyma. This is a suitable segment for local excision, especially in women with a high glandular component, in whom deformity is less common. Local excision without remodelling causes two undesirable effects in the lateral segment: deformity on the lateral contour of the breast and lateral (axillary) deviation of the nipple–areola complex (Figs. 3 and 4). The extent of these adverse effects after a lateral resection depends on the glandular composition of the breast (which is higher in fatty, postmenopausal breasts) and, more importantly, the resection location in this segment. There are three different areas in this segment:
- -
Periareolar area: located around the areola, it is the medial third of segment I. Deformities in this area almost exclusively affect the NAC, whose outline will be distorted.
- -
Medial area: located in the middle third of segment I, it is the most frequent area for resection. It combines contour deformity and medial deviation of the NAC.
- -
Lateral or axillary area: this is the area closest to the armpit or anterior axillary line (lateral third of segment I). Most local resection in this region will not result in a deviation of the NAC or in breast contour deformities, due its remoteness. However, this depends on the extent and volume of the lumpectomy.
Severe effects from a lateral resection (middle third) Local excision and extension of the margins constitute a high-risk scenario for deformities in segment I, where both deviation of the NAC and the breast contour deformity are seen. This 47-year-old woman had an infiltrating lobular carcinoma and underwent a quadrantectomy with expanded margins and a second procedure was necessary due to inadequate margins. The result was an apparent deformity in the lateral segment of the breast that required a mastectomy and immediate breast reconstruction with expander, given the presence of the disease in the new surgical margins.
Two simple procedures are recommended to prevent these defects: medial mobilisation of the NAC with a circular pattern and defect remodelling by mobilisation of upper pole tissue. The basic technical options depend on the location of the tumour, as explained below:
- -
Periareolar: the best choice is local excision from an areolar access and remodelling of the defect by mobilising a dermoglandular flap from the upper pole. If the defect is significant and it is believed that healing and radiation of the surgical bed may pull on the NAC, this can be mobilised medially to compensate for the lateral force.
- -
Medial: The classic choice was the lateral mammoplasty pattern, although in these cases the possibility of a change in its design must be considered to disconnect the quadrantectomy area from the NAC medial mobilisation area. This modification is to try to prevent the pull exerted by the lateral pattern scar on the NAC which sometimes leads to misconfiguration of its contour. In other cases, the external inter-quadrant area can be accessed through a round-block pattern, mobilising the pattern towards the sternum to prevent lateral movement of the NAC after resection.
- -
In these tumours the best option is to approach from the armpit or inframammary fold at its lateral end. In most cases, remodelling of the defect may be done by mobilising the upper pole of the breast.
This segment extends throughout the upper pole of the breast, with its limits being the visible areas of cleavage and periareolar region. As with segment I, it is an area with a high number of breast tumours due to the abundance of glandular tissue. However, unlike the previous segment, different oncoplastic procedures for resection and breast remodelling can be used. Its anatomical positioning (flat surface) and abundance of tissue for remodelling of any defect by local mobilisation make it a segment which is good for both surgeon and patient. Only in cases with a large resection without remodelling or local complication (e.g., seroma or abscess) will leave a pronounced deformity in this area of breast anatomy. This deformity depends on the region in which it occurs. Thus, resections close to the NAC typically lead to its retraction and deviation; while, in the more remote areas, there are changes in the breast surface, deformation of the upper pole or the presence of fibrous bands (Figs. 4 and 5).
There are three methods to prevent deformities in this segment:
- -
Periareolar incision: This is a basic part of performing a lumpectomy in this segment, as the majority of neoplasms are accessible by this approach, and the visual impact of the scar and its local complications (e.g., fibrous bands, dehiscence) are reduced.
- -
Local mobilisation of glandular tissue: The abundance of this tissue type in segment II allows dermoglandular flaps to be constructed in remodelling after the tumour resection. When this procedure, together with periareolar access, is applied during the lumpectomy, the best cosmetic results are obtained in this segment.
- -
Oncoplastic pattern according to the breast and tumour: Sometimes a lumpectomy is not the best option for resection due to the breast features or presentation of the tumour. In these cases, an oncoplastic pattern must be fashioned according to the upper pole, using a batwing horizontal or round-block mammoplasty or a vertical one with an inferior pedicle.
This segment is located at the upper edge of the breast and its main feature is not anatomic but social, i.e., it is a part of the breast that women often display in public. Therefore, from a surgical point of view, this area requires a different evaluation to prevent scarring and deformities. This could be considered as the most cranial part of segment II, however, due to the specific implications on the female body image (regarding public exposure of the scar) and the lack of local tissue for remodelling it plays an important role in surgical planning. The dimensions of this segment vary according to the size and shape of the breast, and are very noticeable in those with excessive ptosis.
Typical deformities in this segment are the presence of visible scars in the infraclavicular region, with a significant impact on the body image of women, affecting their social life (Figs. 5 and 6). There are three methods to prevent this:
- -
Tumour resections in segment III must be performed from an areolar approach, especially in small breasts, or from an intermediate access located in segment II. Either access must enable the mobilisation of local flaps for closing any defect. If an oncoplastic procedure is used, usually a vertical mammoplasty with inferior or internal pedicle, the resection must be performed from the edges of the pattern and tissue mobilisation must be planned in remodelling.
- -
In addition, a sentinel node biopsy of the internal mammary chain must be performed through an invisible incision, either from an areolar access in small breasts or intermediate access in segment II, to prevent visible scarring in the cleavage area.
- -
Segment III tumours near the armpit can be considered via an access from the armpit by tunnelling and, simultaneously, the sentinel node biopsy through the same incision.
As with segment III, the upper medial segment is a visible area of the female breast whose main difficulty is the remoteness of invisible access points and the scarcity of tissue for remodelling. These two features make this segment a particular challenge for breast conservative surgery, as there is no ideal procedure to address these problems. Located in the most medial part of the upper inner quadrant, resections in this location have been marked by a visible deformity in the cleavage area (Figs. 6 and 7), given the inability to restore the volume with local tissue, leaving a scar that influences the patient's clothing. When resection is accompanied by extension of the margins, major deformities can be produced by an ablation of the medial half of the breast which also leads to a retraction of the NAC in many cases. This limitation also affects extension of the margins without remodelling taking place in oncoplastic techniques.
As mentioned above, remodelling this segment depends on the features of each breast and there is no standard procedure for its resolution. However, there are two basic guidelines to be followed during surgery on this segment to improve the aesthetic impact of resection:
- -
Use the nearest invisible access to the tumour bed for resection, i.e. areolar and inframammary access. The objective is to at least prevent a visible scar in the breast area.
- -
Remodel the defect caused by the lumpectomy by mobilising tissue from the upper pole (segments II and III) as this is the only source of autologous tissue available. It is not recommended to mobilise the lower medial area (segment V) as this would completely deform the medial edges of the breast.
The lower medial segment is a ‘no-man's land’ between the upper and lower poles and has traditionally been identified with the lower inner quadrant. Its area is small, as well as its frequency of tumours, and a resection in this area has all the disadvantages mentioned for other segments (visibility of the deformity/scarring), as well as an absence of local resources for remodelling. Therefore, it is a segment that benefits from oncoplastic procedures providing autologous tissue from other locations to mask the defect.
Deformities in this segment are especially visible in lumpectomies with extended margins or on small breasts. Also, deformities in this segment are typical after oncoplastic resection such as that after a haematoma in the medial branch of a horizontal mammoplasty. One feature of segment V deformities is that they are never accompanied by alterations in the NAC.
Alternatives for preventing deformities in this segment require oncoplastic management and can be summarised in two groups:
- -
Remodelling a lumpectomy in segment V benefits from access via the submammary fold and from filling the volume with an adipofascial flap.
- -
In cases where an oncoplastic pattern is required, the procedure that best fits the breast morphology will be indicated, although only two procedures are suitable for this segment. Firstly, a lower rotation mammoplasty allows partial removal of this segment and its remodelling by medial mobilisation of the lower pole via the submammary fold. Secondly, vertical mammoplasty including this segment in the resected section may be used in women with ptotic breast.
This segment includes the entire lower pole except for segment V. Its main anatomical feature is the presence of a convex surface, very evident in a ptotic breast, which has a low tolerance to local tissue remodelling. In general, any attempt at a lumpectomy with local remodelling poses a high risk of deterioration in the contour of the lower pole, due to the straightening of the natural curvature, and this will lead to a deformity after radiation (Figs. 7 and 8). In a significant number of patients this deformity is accompanied by a distortion of the NAC, which in extreme cases causes the typical parrot beak deformity. The risk scenarios for the appearance of these cosmetic defects are extensive lumpectomies or large extensions of the margins that can lead to sunken breast deformities (“axel blows”). In the field of oncoplastic surgery, the most common deformities in this segment occur in a vertical branch scar after excessive extension of the surgical margins.
Prevention of these defects is easily achieved via two procedures:
- -
Using an inframammary access in small breasts and remodelling the defect with an adipofascial flap.
- -
Using a vertical pattern adapted to the anatomy of a ptotic breast of average size.
This segment is an unusual location for breast cancer as it covers a limited region of 2–3cm above the inframammary fold. Its main feature is the low impact that deformities in this area have on the body image of women, as most are hidden by the breast ptosis. Therefore, most patients can benefit from a lumpectomy from the inframammary fold without local remodelling or by masking the defect via dissection of an adipofascial flap when the extent of resection requires so.
Segment VIII (Central)This is the breast segment with the greatest impact on the body image of women as it includes the NAC. Therefore, this region requires special consideration during the preoperative period to determine the affectation of the NAC by the neoplasia. In general, a central resection via a lumpectomy is an accepted procedure as it allows local remodelling with surrounding tissue, which is very abundant in this area. Only large central resections without remodelling lead to sunken breast deformities which are now considered as a thing of the past. In the practice of oncoplastic procedures, central deformities are the result of extensions towards the NAC from segment I or II with poor local remodelling, especially in lateral and horizontal patterns. It may also be caused by necrosis of the NAC during the postoperative period of a vertical mammoplasty.
To solve any of these problems, centrally located tumours have different technical alternatives adapted to the type of tumour and breast that ensure adequate process control and optimal cosmetic outcomes.6
In conclusion, conservative surgery for breast cancer requires an understanding of the impact of local resection on the cosmetic outcome. Therefore, the features of each breast region need to be taken into consideration. Breast segmentation can predict the consequences of local excision in each segment, while selecting the optimum approach for its prevention. Thus, planning the surgery based on breast segmentation achieves the current goal of breast cancer surgery: surgery adapted to the breast and the tumour.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please, cite this article as: Acea Nebril B., Los segmentos mamarios. Un modelo para la prevención de deformidades en la cirugía conservadora del cáncer de mama. Cir Esp. 2011;89:574–80.