Although the majority (95%) of gastrointestinal mesenchymal neoplasms are tumors of the gastrointestinal stroma (GIST) and smooth muscle, there are also descriptions of a large variety of other tumor types with a very low incidence, such as schwannomas, desmoid tumors, solitary fibrous tumors, inflammatory fibroid polyps, inflammatory myofibroblastic tumors, etc.1,2 The main diagnostic problem presented by these uncommon lesions is that they are easily confused with certain morphological types of GIST, especially with CD117-negative GIST and with no mutations in the KIT or PDGFRA genes (wtKIT/PDGFRA).
Recently, a rare form of gastrointestinal mesenchymal neoplasms have been described, that are clinically benign, with fibro/myofibroblastic differentiation and presence of calcified foci. These have been referred to with the descriptive terms of “childhood fibrous tumor with psammoma bodies”3 and “calcifying fibrous tumors”.4
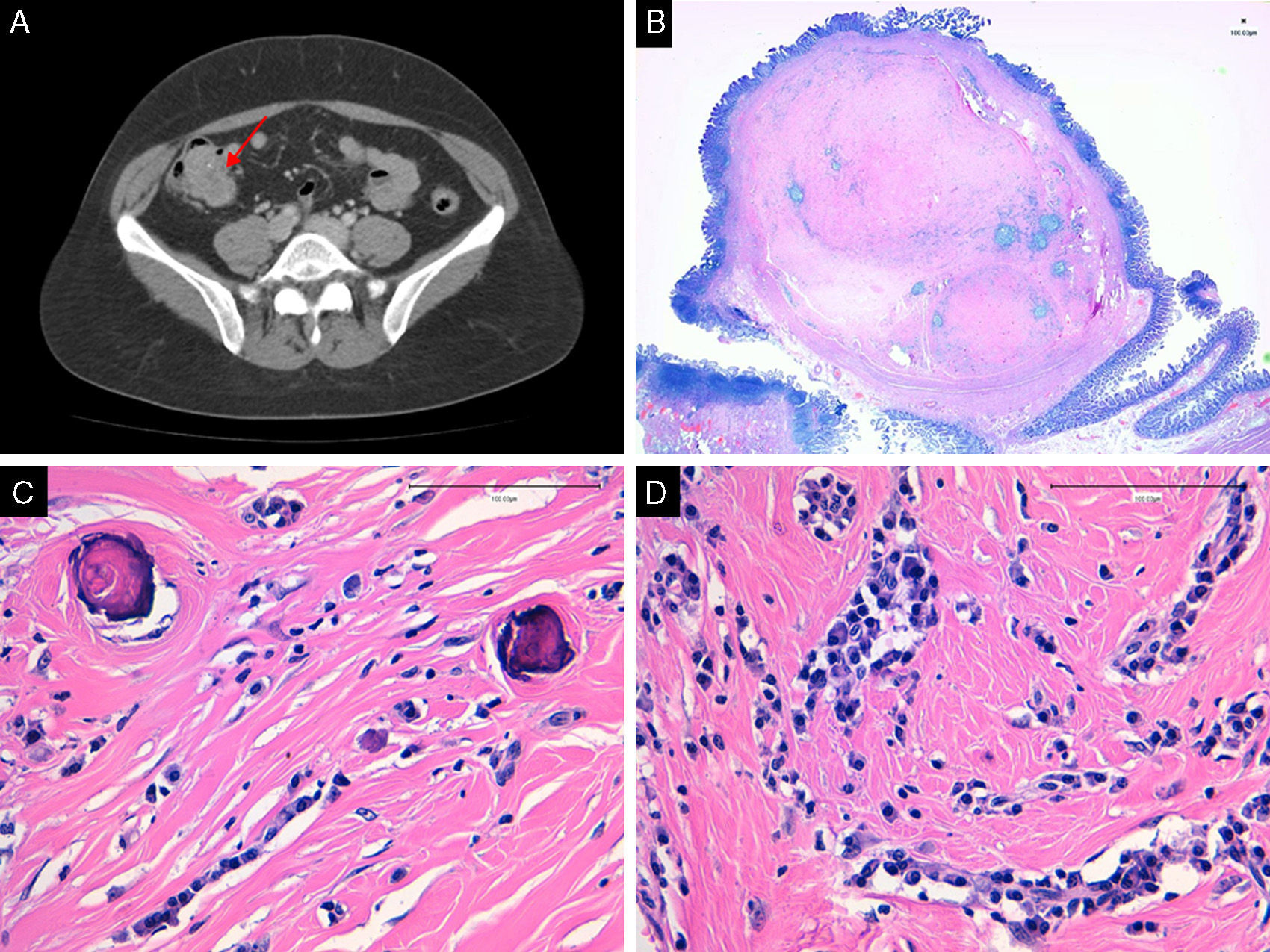
We present the case of a 46-year-old woman who was in treatment for hypertension and had no other history of interest. She consulted with her primary care physician due to recurring abdominal pain and nausea. The patient underwent abdominal ultrasound for suspected gallstones. The study detected thickening of a loop proximal to the terminal ileum, with a wall that was 5mm thick and non-painful; there was also a moderate quantity of fluid in the pelvis, interloop spaces and pouch of Douglas. Colonoscopy showed evidence of a submucosal lesion measuring 2.5×3cm situated in the terminal ileum, whose biopsy was very superficial and not diagnostic. Subsequently, computed tomography with contrast revealed a soft-tissue density mass measuring 4.5cm×2.8cm×2.6cm located in the region of the terminal ileum and ileocecal valve. The tumor protruded towards the interior of the cecum and was well defined, with point-like hyperdensities that were compatible with calcifications. No dilatation of the bowel loops, locoregional lymphadenopathies, or hepatic or pulmonary involvement were observed (Fig. 1). With the clinical suspicion of ileal GIST, laparoscopic ileocolic resection was proposed. The patient developed no complications and was discharged 3 days after the procedure.
The pathology study of the surgical specimen reported a well-defined, non-encapsulated mass measuring 2.5cm at its maximum dimension that was comprised of a hypocellular fibroblastic proliferation growing within a dense matrix with abundant collagen. Inside, there was limited inflammatory infiltrate of plasma cells and lymphocytes as well as areas of dystrophic calcification and psammoma bodies (Fig. 1B–D). With immunohistochemistry techniques, the cells presented positive immunoreaction in occasional cells to CD34 and negative immunoreaction to CD117, DOG1, S100 and AML. Given these findings, the diagnosis of ileal calcifying fibrous tumor (CFT) was reached.
CFT is a soft tissue tumor that is benign and uncommon. It was originally described in girls aged 2–11 by Rosenthal and Abdul-Karim in 1988 as a childhood fibrous tumor with psammoma bodies.3 Initially, these tumors were thought to represent a reactive process resulting from abnormal healing, thus the name “calcifying fibrous pseudotumor”.4 The name was finally changed to CFT in the consensus classification document by the World Health Organisation in 2002.
Cases of CFT have been reported in multiple locations, such as the peritoneum, pleurae, mediastinum, lungs, testicles, suprarenal glands, etc.5–8 Nonetheless, the gastrointestinal location of CFT is especially uncommon, and only around 10 cases have been reported.9
Histopathologically, CFT are circumscribed, non-encapsulated tumors that are comprised of hyalinised collagen, spindle cells without atypia, lymphoplasmacytic infiltrate and psammoma bodies or dystrophic calcifications.10 They are usually incidental findings that are presented as well-outlined nodular formations, both on imaging tests as well as in their later histopathology study, and they show no metastatic capability. Generally, symptoms are very nonspecific, including abdominal pain and altered bowel habit, as in the case we have presented. The differential diagnosis, like submucosal spindle cell tumors, includes GIST, leiomyomas or leiomyosarcomas, schwannomas, desmoid tumors and inflammatory myofibroblastic tumors, etc.9 Diagnosis is easily resolved with an immunohistochemistry study.
The rarity of CFT in the gastrointestinal tract makes its natural history difficult to outline, although there have been no cases of recurrence or metastasis to date. This differs greatly from cases described in other locations, where occasional recurrences have been reported.4 Therefore, treatment of gastrointestinal CFT should be conservative and involve radiological follow-up, especially for lesions removed by enucleation.
In short, our intention is to call attention to this peculiar entity that has easily been confused with GIST or an evolved inflammatory process.
Please cite this article as: Rodríguez Zarco E, Vallejo Benítez A, de Soto Cardenal B, Mora Cabezas M, Pereira Gallardo S. Tumor fibroso calcificante de intestino delgado. Cir Esp. 2016;94:245–247.