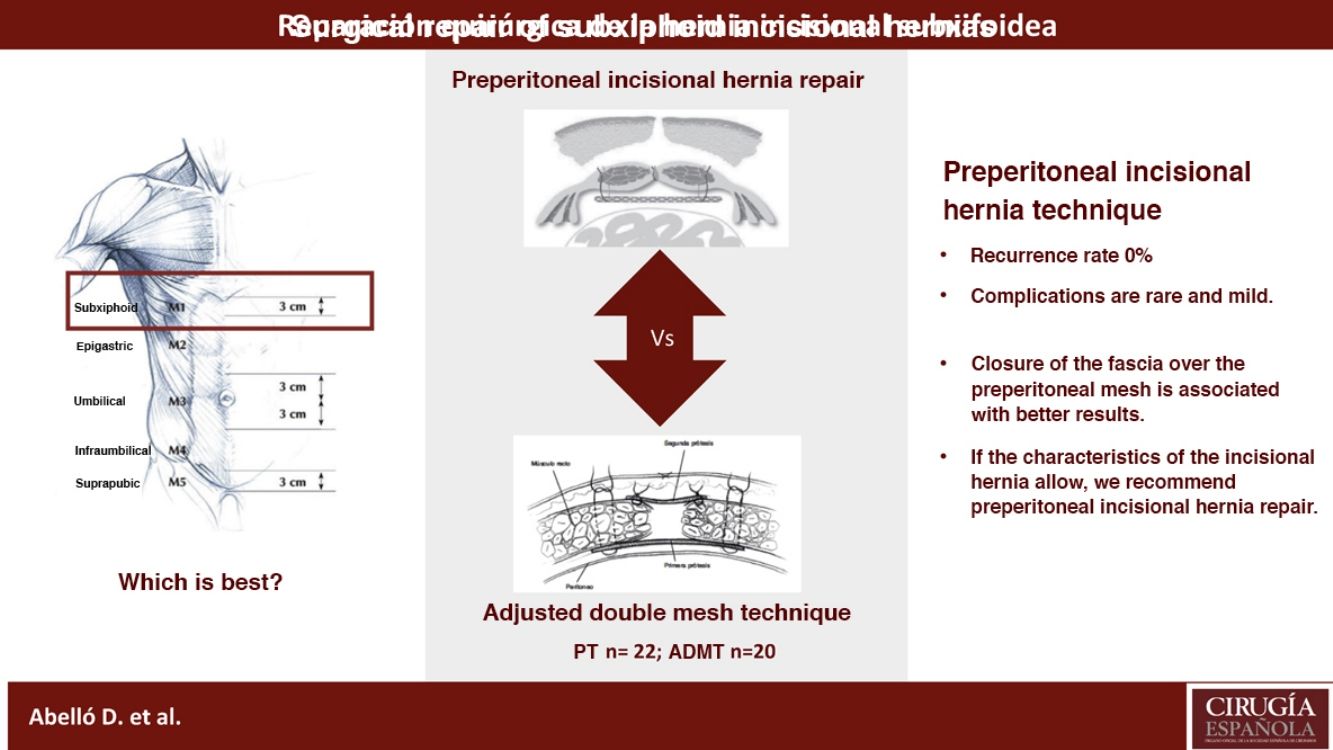
The surgical procedure to repair a subxiphoid incisional hernia is a complex technique due to the anatomical area that it appears. The objective of our study is the analysis of the results obtained with the different surgical techniques performed in our center for 9 years, especially postoperative complications and the recurrence rate.
MethodsIt is an observational, retrospective study from January 2011 to January 2019 of patients operated of subxiphoid incisional hernia in our Unit. We analysed the comorbidities, surgical techniques (preperitoneal hernia repair or TP, and adjusted double mesh technique) and postoperative variable, especially the hernia recurrence. The postoperative complications were summarized flowing the Clavien-Dindo classification.
Results42 patients were operated: 22 (52,4%) TP and 20 (47,6%) adjusted double mesh technique. All the complications registered were minor (grade I) and it appeared mostly in TP group (P = .053). The average follow up was 25.8 ± 15.1 months; there were no statistically significant differences in hernia recurrence comparing two treatment groups (P = .288).
ConclusionsAccording to our results, TP is the ideal technique to repair a subxiphoid incisional hernia. Adjusted double mesh technique may represent an effective approach with a low complication rate, although globally analyzing the recurrence rate, aponeurosis closure over the preperitoneal mesh entails less impact on it.
La hernia incisional subxifoidea presenta complejidad en su solución quirúrgica por las características de la región anatómica donde aparece. El objetivo de nuestro estudio fue el análisis de los resultados obtenidos con las diferentes técnicas realizadas en nuestro centro durante 9 años, incidiendo en las complicaciones postoperatorias y la tasa de recidiva.
MétodosEstudio observacional, retrospectivo desde enero de 2011 hasta enero de 2019 de los pacientes intervenidos de hernia incisional subxifoidea en nuestra Unidad. Se analizaron las comorbilidades, técnicas quirúrgicas empleadas (eventroplastia preperitoneal o TP, y técnica de doble malla ajustada) y variables postoperatorias, incidiendo en la recidiva herniaria. Las complicaciones se recogieron según la clasificación de Clavien-Dindo.
ResultadosSe intervinieron un total de 42 pacientes: 22 (52,4%) mediante una TP, y 20 (47,6%) mediante técnica de doble malla ajustada. Todas las complicaciones registradas fueron leves (grado i) y aparecieron mayoritariamente en el grupo de la TP (p = 0,053). El seguimiento medio postoperatorio fue 25,8 ±15,1 meses; no existieron diferencias estadísticamente significativas en cuanto a recidiva comparando los 2 grupos de tratamiento (p = 0,288).
ConclusionesSegún nuestros resultados, la TP fue la técnica ideal para reparar una hernia incisional subxifoidea. La técnica de doble malla ajustada puede representar un abordaje eficaz con un bajo índice de complicaciones, aunque analizando globalmente la tasa de recidiva, el cierre fascial por encima de la prótesis preperitoneal conlleva un menor impacto en la misma.
Subxiphoid incisional hernias (SIH), or M1 according to the European Hernia Society (EHS) classification1, have an incidence of 1%–4.2% in patients who have undergone sternotomy2,3. Its global incidence varies according to the series, which is due to the fact that SIH are small in size and go unnoticed by the patient and the medical professional. It is also rare for SIH to cause symptoms or episodes of incarceration4.
The only studies that analyze the incidence and risk factors for developing SIH are based on patients who have undergone sternotomies performed during surgeries- involving thoracic or cardiovascular surgeons2,5,6. The main risk factor described for developing SIH is the need for transfusion of packed red blood cells, which can be considered an indirect marker of surgical complexity5. Obesity and postoperative surgical wound infection are also predisposing factors7 and common variables in the development of any incisional hernia. SIH can also occur after subcostal and supraumbilical laparotomies in patients with high comorbidity4, such as, for example, liver transplant recipients or patients with immunosuppressive treatment7.
The surgical solution for SIH is complex8. Primary closure of the defect has been reported to lead to hernia recurrence in up to 80% of cases9, and postoperative complications can appear in 50% of patients10. This difficulty is related to the anatomical region where it occurs (inferior to the costal margin and the xiphoid process), and the bone structures that can hinder fixation and adequate coverage of the mesh over the hernia defect, which may lead to an aponeurotic closure with tension11.
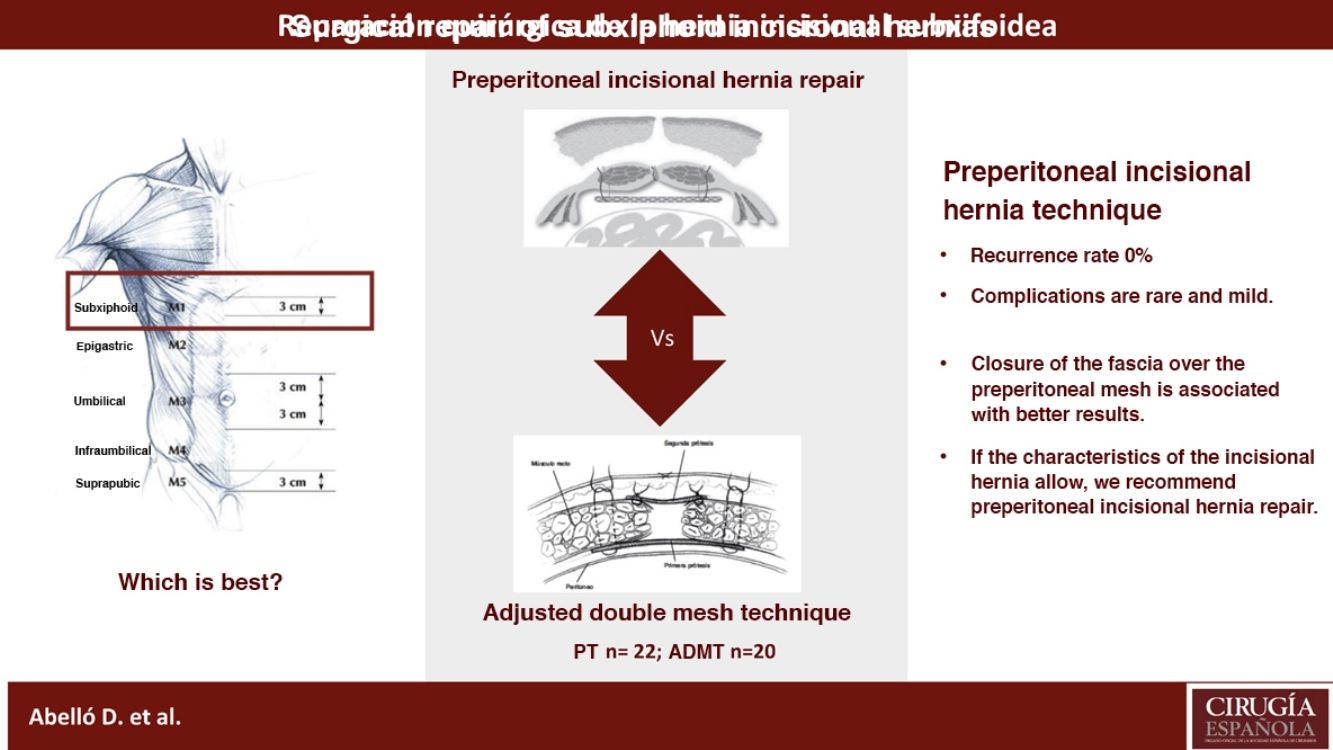
The objective of our study was to retrospectively analyze the rate of recurrence and comorbidity in the surgical repair of SIH using a preperitoneal incisional hernia repair technique (PT) or the adjusted double-mesh technique (ADMT).
MethodsWe have conducted an observational and retrospective study of SIH procedures performed at our Hospital from January 2011 to January 2019.
All patients with SIH were evaluated in outpatient clinics and were studied preoperatively by computed tomography (CT) scan to classify the type of incisional hernia using the EHS classification12. The study inclusion criteria were: patients who underwent elective SIH that included areas M1 or M1-M2. SIH combined with defects also in M3, M4 and M5, as well as repairs performed in the emergency room, were excluded from the study.
All patients were operated on by the same team of 5 specialists in abdominal wall surgery. The main surgeon chose the surgical technique to be performed as well as the type of prosthesis to be used. The surgical repairs performed to address SIH included the preperitoneal technique (PT) and ADMT, as previously described by our group11. In general terms, the surgeon leaned towards performing ADMT when the SIH presented a transverse hernia defect diameter 10 ≥ cm, which seriously hindered suprafascial closure over the prosthesis.
The patients were administered antibiotic prophylaxis one hour before the skin incision, as well as thromboembolic prophylaxis with low-molecular-weight heparin, which was initiated 6 h after surgery. The skin antiseptic used was alcoholic chlorhexidine or povidone iodine. In PT, the hernia sac was dissected up to its neck, progressing in the dissection along the subxiphoid and substernal preperitoneal plane, surpassing the defect by 5 cm on all axes, where we finally positioned the prosthetic mesh. The most widely used type of mesh was wide-pore polypropylene (PPL), which was affixed with interrupted sutures of PPL or extra–long-term absorption monofilament sutures (Monomax®), using AbsorbaTack® at the ribs and sternum. Subsequently, the primary closure of the rectus aponeurosis was attempted above the prosthesis with continuous slow absorption monofilament suture (Monomax loop®).
Unlike the previous technique, in ADMT, once the PPL mesh was positioned in the preperitoneal position, the rectus sheath was not closed, but rather a second PPL inlay mesh was positioned and adjusted to the edge of the defect by means of a continuous PPL monofilament suture11.
For all patients, we used wide preperitoneal overlap of the mesh prosthesis in the retroxiphoid area with fixation to the xiphoid and ribs. In all cases, redon drains were placed in the preperitoneal dissection area where the mesh was located. These drains were removed when the daily discharge was less than 50 cc. At the end of the procedure, a compression bandage was applied, and an abdominal girdle was placed in the hospital room, which the patients used for the first 2 postoperative months.
The following epidemiological data were reviewed respectively: age, sex, and comorbidities (obesity, smoking, arterial hypertension, diabetes mellitus, bronchopathy, use of anticoagulants, and organ transplant recipient). In addition, we analyzed intraoperative variables (surgical time, surgical incidents, concomitant surgeries, etc.) and postoperative variables (complications according to the Clavien–Dindo13 classification, length of hospital stay, readmission rate, recurrence rate). Hernia recurrence was defined clinically by physical examination of the patient, and we requested an abdominal computed tomography scan in Valsalva for confirmation. Finally, we carried out a comparative analysis of the 2 surgical techniques performed, focusing on the rate of recurrence and perioperative complications.
The patients were monitored in the outpatient clinical with postoperative follow-up visits at 15 days, 30 days, 6 months and 1 year, followed by annual appointments until completing a 3-year follow-up period, which we tried to complete in most patients.
The statistical analysis was conducted with IBM SPSS® Statistics version 25.0 software (IBM, USA), using the means with standard deviation as the main descriptive measures for the quantitative variables, and frequencies with percentages for the qualitative variables. The chi-squared test was used for the qualitative variables and the Student’s t test for the quantitative variables. Differences were considered significant when the P value was less than .05.
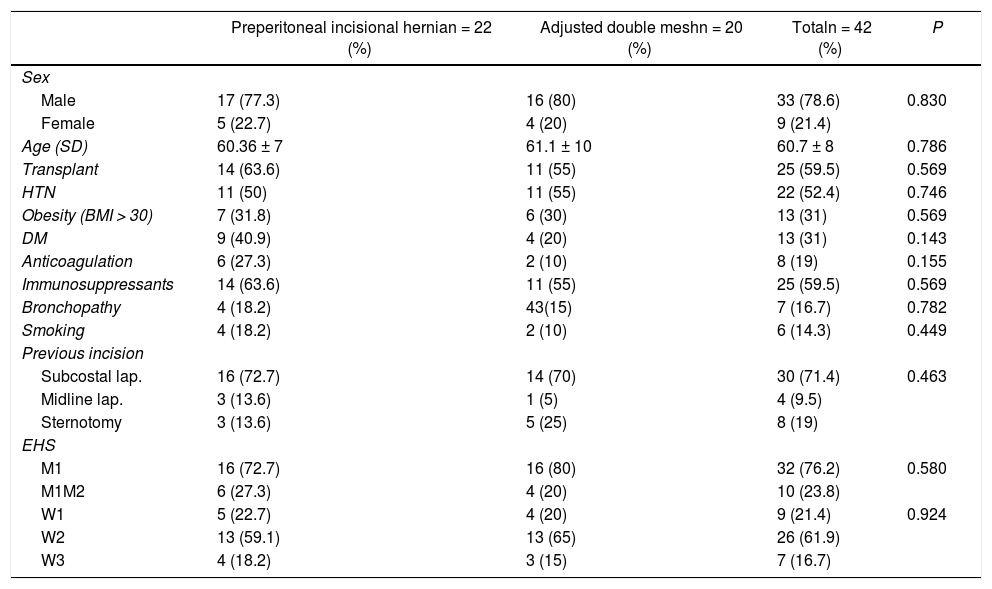
ResultsWe analyzed a total of 42 patients who underwent surgical repair of an SIH between January 2011 and January 2019. Table 1 shows the patient demographic variables and comorbidities as well as characteristics of the SIH according to the EHS classification.
Demographic and surgery technique variables used with SIH.
| Preperitoneal incisional hernian = 22 (%) | Adjusted double meshn = 20 (%) | Totaln = 42 (%) | P | |
|---|---|---|---|---|
| Sex | ||||
| Male | 17 (77.3) | 16 (80) | 33 (78.6) | 0.830 |
| Female | 5 (22.7) | 4 (20) | 9 (21.4) | |
| Age (SD) | 60.36 ± 7 | 61.1 ± 10 | 60.7 ± 8 | 0.786 |
| Transplant | 14 (63.6) | 11 (55) | 25 (59.5) | 0.569 |
| HTN | 11 (50) | 11 (55) | 22 (52.4) | 0.746 |
| Obesity (BMI > 30) | 7 (31.8) | 6 (30) | 13 (31) | 0.569 |
| DM | 9 (40.9) | 4 (20) | 13 (31) | 0.143 |
| Anticoagulation | 6 (27.3) | 2 (10) | 8 (19) | 0.155 |
| Immunosuppressants | 14 (63.6) | 11 (55) | 25 (59.5) | 0.569 |
| Bronchopathy | 4 (18.2) | 43(15) | 7 (16.7) | 0.782 |
| Smoking | 4 (18.2) | 2 (10) | 6 (14.3) | 0.449 |
| Previous incision | ||||
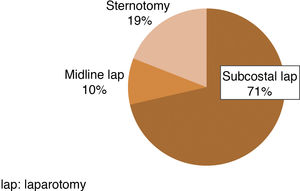
| Subcostal lap. | 16 (72.7) | 14 (70) | 30 (71.4) | 0.463 |
| Midline lap. | 3 (13.6) | 1 (5) | 4 (9.5) | |
| Sternotomy | 3 (13.6) | 5 (25) | 8 (19) | |
| EHS | ||||
| M1 | 16 (72.7) | 16 (80) | 32 (76.2) | 0.580 |
| M1M2 | 6 (27.3) | 4 (20) | 10 (23.8) | |
| W1 | 5 (22.7) | 4 (20) | 9 (21.4) | 0.924 |
| W2 | 13 (59.1) | 13 (65) | 26 (61.9) | |
| W3 | 4 (18.2) | 3 (15) | 7 (16.7) |
SD: standard deviation; DM: diabetes mellitus; EHS: European Hernia Society; HTN: hypertension; BMI: body max index; lap: laparotomy.
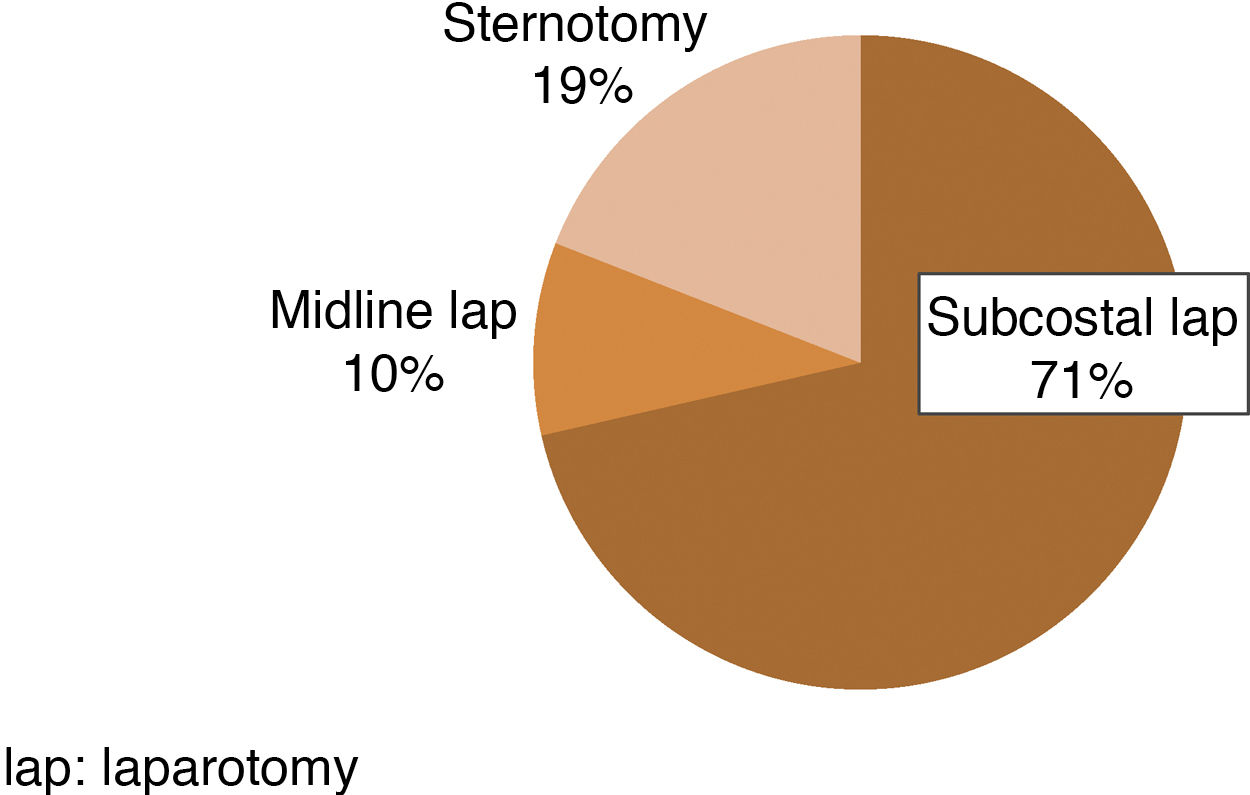
Most of the patients were operated on with a SIH M1W2. Subcostal laparotomy was the most frequent previously performed herniated incision in our series (71%) (Fig. 1). PT was the most frequent surgical option, performed in 22 patients (52.4%), while ADMT was performed in 20 patients (47.6%). There were no significant differences between the 2 treatment groups in terms of comorbidity and SIH characteristics.
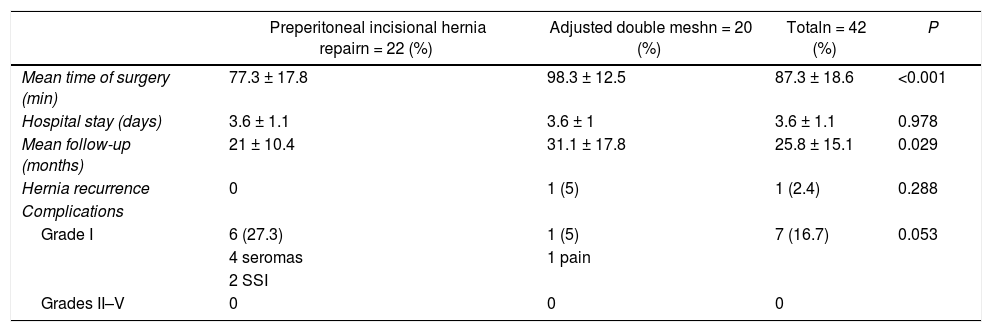
Table 2 shows the perioperative results of both surgical techniques. The surgical time required for the PT was lower than that of the ADMT (77.3 ± 17.8 min vs 98.3 ± 12.5 min; P < .001); however, there were no differences in terms of hospital stay (3.6 ± 1.1 days vs 3.6 ± 1.1 days; P = .978). In neither of the 2 techniques were intraoperative complications recorded. All postoperative complications that were recorded (seroma, wound infection, and pain) were mild (Clavien–Dindo grade I) and resolved with conservative treatment. ADMT presented better results than PT in terms of its appearance.
Perioperative variables, follow-up, hernia recurrence and surgical complications according to the Clavien-Dindo classification.
| Preperitoneal incisional hernia repairn = 22 (%) | Adjusted double meshn = 20 (%) | Totaln = 42 (%) | P | |
|---|---|---|---|---|
| Mean time of surgery (min) | 77.3 ± 17.8 | 98.3 ± 12.5 | 87.3 ± 18.6 | <0.001 |
| Hospital stay (days) | 3.6 ± 1.1 | 3.6 ± 1 | 3.6 ± 1.1 | 0.978 |
| Mean follow-up (months) | 21 ± 10.4 | 31.1 ± 17.8 | 25.8 ± 15.1 | 0.029 |
| Hernia recurrence | 0 | 1 (5) | 1 (2.4) | 0.288 |
| Complications | ||||
| Grade I | 6 (27.3) | 1 (5) | 7 (16.7) | 0.053 |
| 4 seromas | 1 pain | |||
| 2 SSI | ||||
| Grades II–V | 0 | 0 | 0 |
SSI: surgical site infection.
The mean postoperative follow-up was 25.8 ± 15.1 months, finding a hernia recurrence rate of 2.4%. Although there were no significant differences in terms of recurrence, it should be noted that the only registered case is from the ADMT group. This appeared one year after follow-up in a patient with multiple risk factors (obesity, smoking, high blood pressure, and liver transplantation). The characteristics of the recurrence were a new symptomatic incisional hernia in the lower part of the prosthesis placed during the ADMT, in M2-M3 position. Anterior separation of components was selected for the repair, with good results and with no new recurrence in the subsequent follow-up.
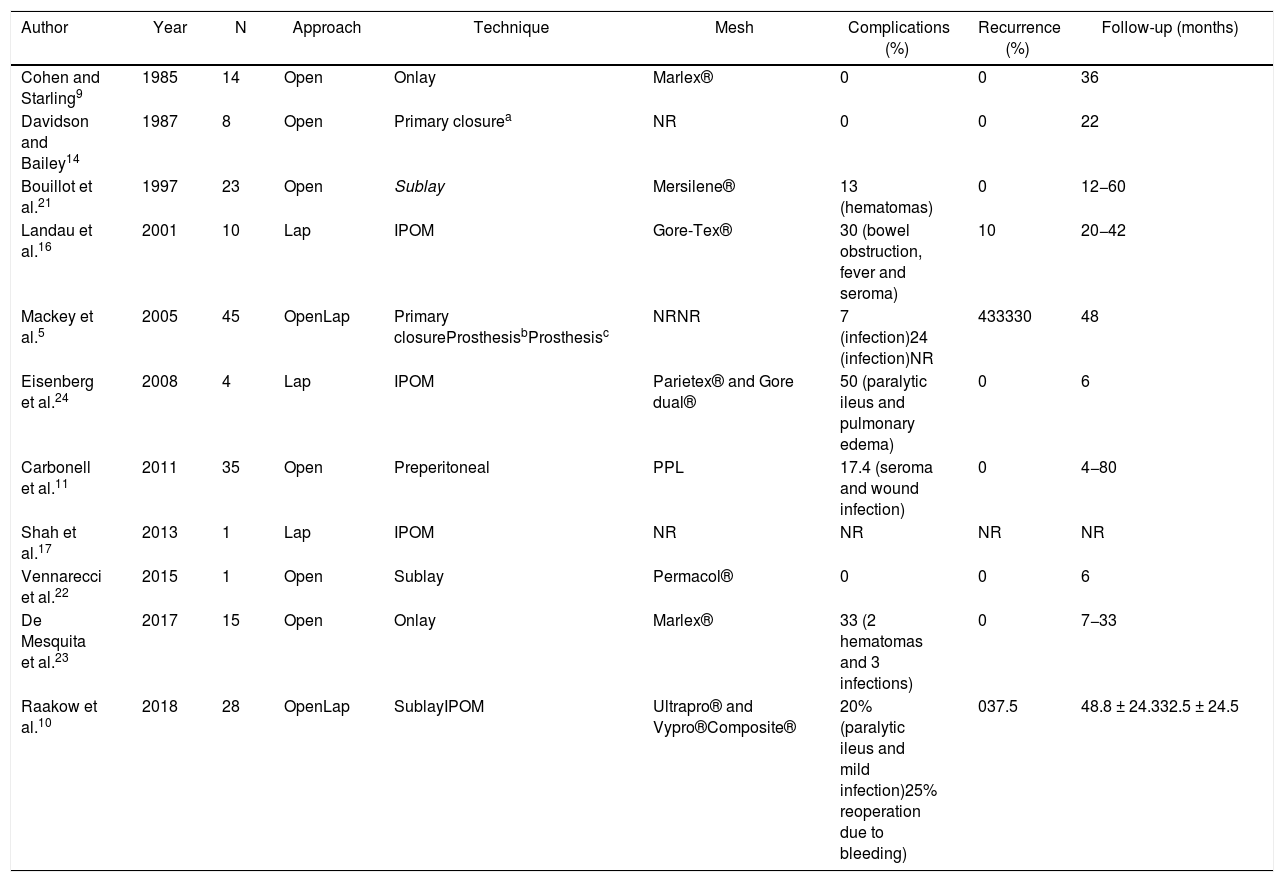
DiscussionSeveral surgical techniques have been described in the scientific literature to treat SIH. The first to be described was the primary closure of the defect associated with a supra-aponeurotic mesh, which provided results that were less than acceptable9,14. Subsequently, the preperitoneal approaches (PT and ADMT) were described11,15, and more recently, the placement of intra-abdominal mesh via laparoscopy10,16,17. Table 3 summarizes the results of the most representative series published in the scientific literature to date.
Series about SIH published in the literature from 1985 until today using intraabdominal mesh (IPOM).
| Author | Year | N | Approach | Technique | Mesh | Complications (%) | Recurrence (%) | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|
| Cohen and Starling9 | 1985 | 14 | Open | Onlay | Marlex® | 0 | 0 | 36 |
| Davidson and Bailey14 | 1987 | 8 | Open | Primary closurea | NR | 0 | 0 | 22 |
| Bouillot et al.21 | 1997 | 23 | Open | Sublay | Mersilene® | 13 (hematomas) | 0 | 12−60 |
| Landau et al.16 | 2001 | 10 | Lap | IPOM | Gore-Tex® | 30 (bowel obstruction, fever and seroma) | 10 | 20−42 |
| Mackey et al.5 | 2005 | 45 | OpenLap | Primary closureProsthesisbProsthesisc | NRNR | 7 (infection)24 (infection)NR | 433330 | 48 |
| Eisenberg et al.24 | 2008 | 4 | Lap | IPOM | Parietex® and Gore dual® | 50 (paralytic ileus and pulmonary edema) | 0 | 6 |
| Carbonell et al.11 | 2011 | 35 | Open | Preperitoneal | PPL | 17.4 (seroma and wound infection) | 0 | 4−80 |
| Shah et al.17 | 2013 | 1 | Lap | IPOM | NR | NR | NR | NR |
| Vennarecci et al.22 | 2015 | 1 | Open | Sublay | Permacol® | 0 | 0 | 6 |
| De Mesquita et al.23 | 2017 | 15 | Open | Onlay | Marlex® | 33 (2 hematomas and 3 infections) | 0 | 7−33 |
| Raakow et al.10 | 2018 | 28 | OpenLap | SublayIPOM | Ultrapro® and Vypro®Composite® | 20% (paralytic ileus and mild infection)25% reoperation due to bleeding) | 037.5 | 48.8 ± 24.332.5 ± 24.5 |
Lap: laparoscopic; NR: not recorded; PPL: polypropylene.
Hernia recurrence after SIH repair is high5,10. Possible influencing factors include the location of the defect, which contributes to the complexity of the repair as it is in an area of tension. Furthermore, there is little room for maneuverability during the fascia approximation and closure of the hernia defect. The proximity of bone structures also influences mesh fixation, making extensive retrosternal dissection necessary in order to achieve a large area of overlap under the bone to accommodate the prosthesis.
Holihan et al.18,19 published 2 meta-analyses where they demonstrated that positioning the mesh in a preperitoneal instead of a suprafascial position reduces the rates of recurrence and surgical site infection18,19. Even so, the supra-aponeurotic position of the mesh is an approach that continues to be widely used in our country20. An extensive plane of retrosternal preperitoneal dissection is essential for wide mesh coverage, going several centimeters beyond the entire hernia defect. Hence, the technique of choice for SIH repair is the preperitoneal technique10,21,22.
Raakow et al.10 and Mackey et al.5 are the only groups that have published the results of a comparative study on SIH repair techniques, which found that hernia recurrence after repair is influenced by the positioning of the mesh. Mackey observed a 43% incidence of hernia recurrence at primary closure, which decreased to 30% when he used mesh. Raakow showed that the recurrence rate can reach 0% with the use of PT.
However, published data regarding the appearance of complications, the surgical approach and the plane to position the mesh are very diverse5.
It is important to note that the choice of surgical technique is also influenced by the characteristics of the incisional hernia. Our group tries to position the mesh in the preperitoneal plane, widely surpassing the defect, and subsequently performing a tension-free primary closure of the anterior defect of the rectus sheath. In cases where this primary closure is not possible, a second mesh is positioned following the double-mesh technique, which, by positioning a second inlay mesh, allows for the edges of the anterior fascia to be connected without tension to protect the preperitoneal mesh. Even so, our results regarding hernia recurrence showed that there are no significant differences between the two options. We found one case of recurrence in the ADMT group influenced by the lack of closure of the suprafascial defect with SIH and a transverse diameter greater than 10 cm.
Postoperative complications associated with SIH repair are multiple and diverse. The most frequent are those related to the surgical wound (such as hematomas, seromas or surgical site infections) that can be resolved with conservative management11,16,23. However, in the series by Raakow et al10, it is striking that the laparoscopic approach subgroup had a 25% rate of surgical reoperations due to bleeding (grade IIIb), although the cause of this high incidence was not explained. Despite negative factors, such as the existence of immunosuppression or comorbidity associated with these patients, the results of our series regarding postoperative morbidity seem correct to us. All the postoperative complications recorded were mild (grade I). The incidence of these was more frequent in the PT group (27.3%) compared to the ADMT group (5%). This was possibly due to the fact that patients with complications are part of a subgroup with abundant comorbidity (HTN, obesity, bronchopathy, diabetes, etc.). Even so, this complication rate is at the lower limit of what has been published in the literature5,10,11,21,24.
Regarding the demographic characteristics and comorbidity of the patients, there was a large volume of patients whose medical History included a transplantation (59.5%). This fact is partially explained by their being long and complex surgeries that often require the transfusion of blood products, which are elements that can affect tissue quality5. In addition, immunosuppressive medication, especially steroids, alter the healing process and predispose patients to the formation of hernias25,26. Therefore, it is interesting to consider the possibility of preventing SIH by placing a prophylactic mesh during subcostal laparotomy. In patients undergoing bilateral subcostal laparotomy, Blazquez et al.27 have shown a reduction in the incidence of incisional hernia of 1.7% in the group with the prophylactic mesh placed in the suprafascial position compared to 17.5% in the group without mesh (P = .0006). Likewise, in patients with midline laparotomy, Borab et al.28 and Argudo et al.29 also reported a reduction in the risk of incisional hernia of 85% and 78%, respectively, through the use of suprafascial mesh. Lastly, we should mention a multicenter clinical trial, PRIMA, which concludes that there is a significant reduction in the risk of incisional hernia with the positioning of a suprafascial mesh in midline laparotomies compared to the retromuscular position in high-risk patients30. Although it is not the objective for this study and along the same line as what was published by the previous groups, in patients with high comorbidity and a high probability of developing SIH, the placement of a prophylactic mesh could be useful.
Our study has limitations. On the one hand, the retrospective analysis of the series is limited by the information found in the clinical history of each patient as well as the bias of the observer. Thus, 42 cases could represent a small number of cases to draw conclusions, but we must not forget that these numbers are similar to (and even greater than) the other series analyzed. The most interesting part of this study may lie in the comparison of 2 SIH surgical techniques, as well as the acceptable results when analyzing hernia complications and recurrence during a mean follow-up period of more than 25 months. We hope that this article lays the foundation for being able to conduct a prospective multicenter study with a larger sample size that would allow us to reach more solid conclusions regarding the efficacy of surgical techniques to treat SIH.
As conclusions, and according to our results, preperitoneal hernia repair is the ideal technique to repair subxiphoid incisional hernias. The adjusted double-mesh technique may be an effective approach with a low complication rate, but when the recurrence rates are analyzed globally, fascial closure over the preperitoneal prosthetic mesh has a lesser impact.
Conflict of interestsThe authors have no conflict of interests to declare. This study has received no specific funding from public, commercial or non-profit organizations.
Please cite this article as: Abelló D, Martínez-Hoed J, Menéndez M, Cholewa H, Avelino L, Bonafé S, et al. Análisis comparativo de 2 técnicas quirúrgicas en el tratamiento de la hernia incisional subxifoidea. Estudio observacional. Cir Esp. 2021;99:578–584.