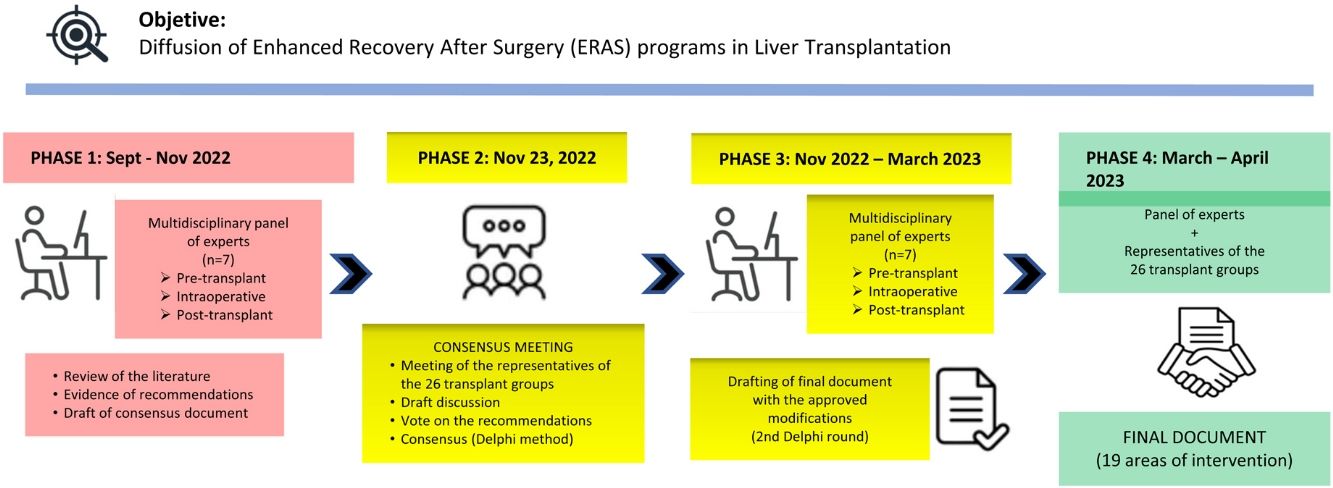
The goal of the Spanish Society for Liver Transplantation (La Sociedad Española de Trasplante Hepático) is to promote and create consensus documents about current topics in liver transplantation with a multidisciplinary approach. To this end, in November 2022, the 10th Consensus Document Meeting was held, with the participation of experts from the 26 authorized Spanish liver transplantation programs. This edition discusses Enhanced Recovery After Liver Transplantation, dividing needed actions into three periods: preoperative, intraoperative and postoperative. The evaluated evidence and the consensus conclusions for each of these topics are described.
La Sociedad Española de Trasplante Hepático tiene como objetivo la promoción y elaboración de documentos de consenso sobre temas de actualidad en trasplante hepático de abordaje multidisciplinario. Para ello, en noviembre 2022 se celebró la X Reunión de consenso con participación de representantes de los 26 programas de trasplante hepático españoles autorizados. En esta edición se abordó la Recuperación Intensificada tras el Trasplante Hepático, dividiendo las acciones a realizar en tres periodos, preoperatorio, intraoperatorio y postoperatorio. Se expone a continuación las evidencias evaluadas, y las consecuentes recomendaciones consensuadas.
The 2021 ERAS (Enhanced Recovery After Surgery) guidelines define the general measures designed to optimize rehabilitation or postoperative recovery by reducing surgical complications and improving the perceived quality of life of patients undergoing abdominal surgery.1
The implementation of ERAS programs in the context of liver transplantation (LT) has not been widely developed. In Spain, it is the intention of the Spanish Society of Liver Transplantation (Sociedad Española de Trasplante Hepático, or SETH) to promote these protocols, and the initial step is to reach a consensus on the measures to be implemented in LT programs.
Material and methodsIn September 2022, the SETH created a multidisciplinary working group that included surgeons, hepatologists and anesthesiologists who specialize in LT. Our aim was to review the current evidence regarding elements that favor better, faster patient recovery after LT and criteria for early and safe discharge, while guaranteeing maximum safety. Three periods were established— pre-transplantation, intraoperative, and post-transplantation — following the same criteria as other consensus documents from the same society.2
The review of the literature provided the points to be debated, which were compiled in a draft and distributed among the 26 representatives of the national LT groups.
We followed the modified Delphi method3 and consulted the following sources: MEDLINE, PubMed, and sources from different scientific societies involved in transplantation and hepatology, using the terms [“liver transplantation” or “cirrhosis” ] AND [“education”, “safe discharge”, “nutrition”, “sarcopenia”, “prehabilitation”, “fast-track”, “ERAS”]. The preliminary list of recommendations was submitted to all groups for debate; if 75% agreement was not reached, the recommendation was again discussed. The final version of the document only included recommendations that reached a consensus of 75%, which was then redistributed among the group representatives for final comments and approval (second Delphi round).
The scientific evidence and grade of recommendation were established following the 2 dimensions of the GRADE system4 — Quality of the evidence: (A) high; (B) moderate; (C) low; and Strength of the recommendation: (1) strong; (2) weak.
This document contains the conclusions reached at the 10th SETH Consensus Meeting in November 2022, with representatives from all LT groups in Spain.
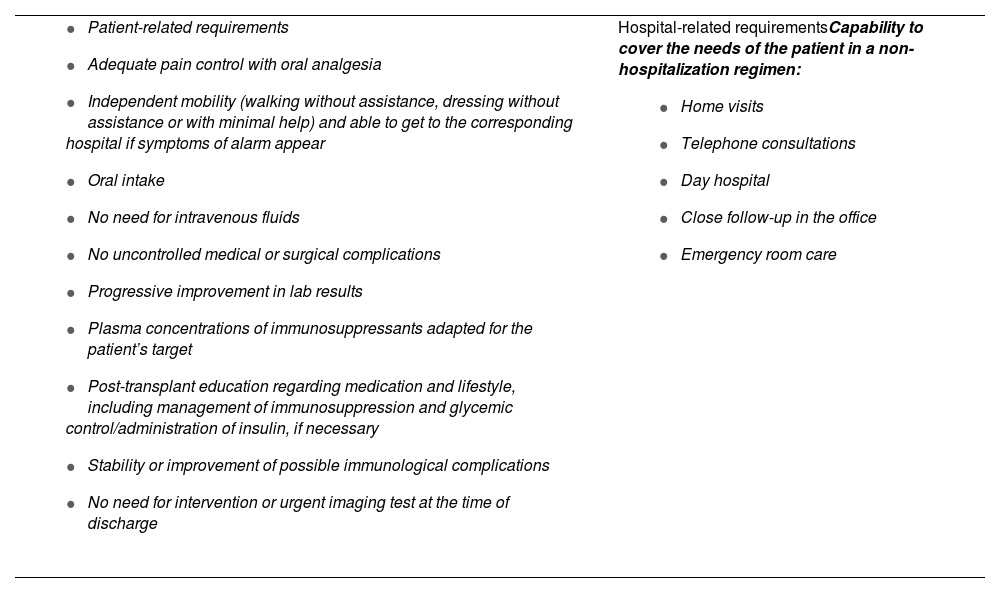
Prior to describing the evidence evaluated and the consequent recommendations, it was necessary to agree on the objectives and criteria for safe, early discharge5 (Table 1), as well as the indicators of the ERAS program.
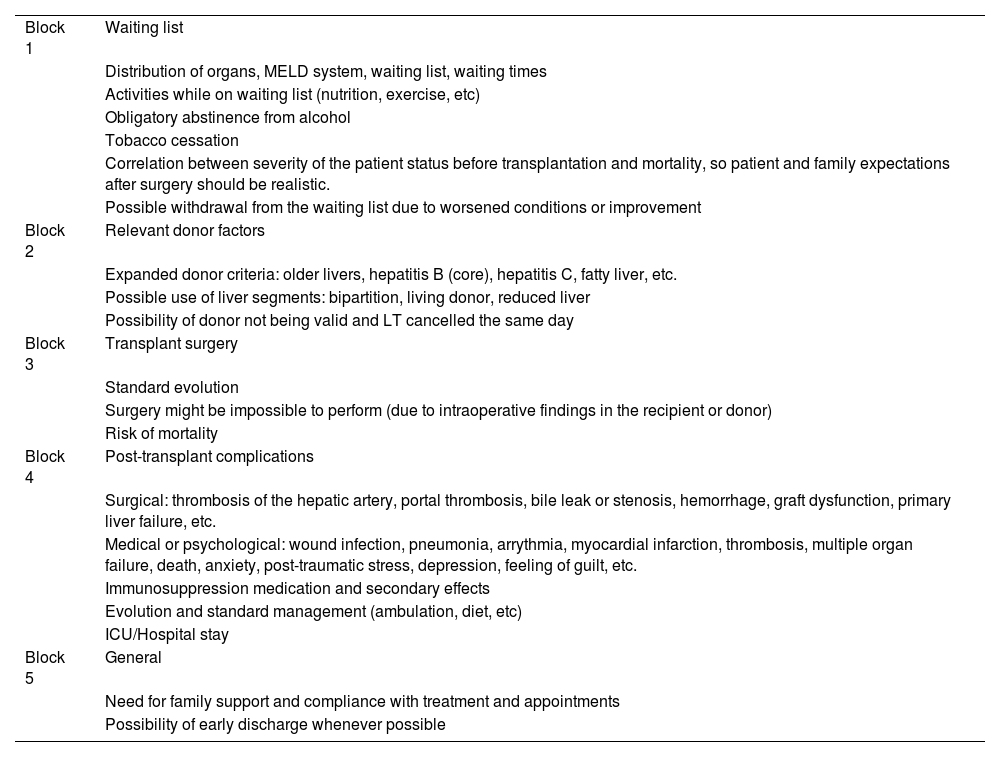
Information checklist for when the patient is added to the waitlist.
| Block 1 | Waiting list |
| Distribution of organs, MELD system, waiting list, waiting times | |
| Activities while on waiting list (nutrition, exercise, etc) | |
| Obligatory abstinence from alcohol | |
| Tobacco cessation | |
| Correlation between severity of the patient status before transplantation and mortality, so patient and family expectations after surgery should be realistic. | |
| Possible withdrawal from the waiting list due to worsened conditions or improvement | |
| Block 2 | Relevant donor factors |
| Expanded donor criteria: older livers, hepatitis B (core), hepatitis C, fatty liver, etc. | |
| Possible use of liver segments: bipartition, living donor, reduced liver | |
| Possibility of donor not being valid and LT cancelled the same day | |
| Block 3 | Transplant surgery |
| Standard evolution | |
| Surgery might be impossible to perform (due to intraoperative findings in the recipient or donor) | |
| Risk of mortality | |
| Block 4 | Post-transplant complications |
| Surgical: thrombosis of the hepatic artery, portal thrombosis, bile leak or stenosis, hemorrhage, graft dysfunction, primary liver failure, etc. | |
| Medical or psychological: wound infection, pneumonia, arrythmia, myocardial infarction, thrombosis, multiple organ failure, death, anxiety, post-traumatic stress, depression, feeling of guilt, etc. | |
| Immunosuppression medication and secondary effects | |
| Evolution and standard management (ambulation, diet, etc) | |
| ICU/Hospital stay | |
| Block 5 | General |
| Need for family support and compliance with treatment and appointments | |
| Possibility of early discharge whenever possible |
The working group identified the following basic indicators to evaluate the results and compare the different pre-, intra- and postoperative elements: length of hospital stay and Intensive Care Unit (ICU) stay, rate of complications, intrahospital mortality, ICU readmission rate, hospital readmission rate, and ERAS protocol compliance rate.
Evidence and recommendations for the implementation of the ERAS program in LTPre-operative period (Prehabilitation)Prehabilitation: pre-transplant educationDoes pre-transplant education influence postoperative evolution?There are no consensus guidelines about the instructions and information that should be given to patients who are candidates for LT. However, factors like nutrition, immunosuppression, and glycemic control must be discussed before adding the patient to the transplant list. To facilitate compliance with the objectives, the 2021 ERAS clinical guidelines recommend that this information be addressed not only to the patient but also their immediate family or caretakers.1,5,6
RecommendationAll patients who are candidates for LT must receive information and instructions before/upon being added to the waiting list in order to actively participate in their recovery process. Evidence/Recommendation: C1
Intervention proposalsThe patient is provided detailed information by specialized staff before being added to the waiting list. To this end, a “check-list” could be prepared previously and then reviewed with the patient and family members/caretaker (example in Table 2).
Criteria for safe discharge.
| Hospital-related requirementsCapability to cover the needs of the patient in a non-hospitalization regimen:
|
Informative workshops should be created for patients with recent transplants or those on the waiting list, which would be taught by former transplant recipients and medical staff who work in the LT program.
Prehabilitation: physical exerciseCan a physical prehabilitation program help improve immediate recovery after LT surgery?Any improvement in the functional capacity of patients awaiting LT using training and physical exercise programs could influence the postoperative period in the short and medium term, while also improving the recovery of patients after surgery.7 However, there is no scientific evidence regarding the possible impact of physical prehabilitation on short-term benefits after transplantation.8
RecommendationAlthough there is no evidence regarding the benefits of a physical exercise program, it is considered non-detrimental and safe. Evidence/Recommendation: C2
Proposed interventionIn previously selected patients, schedule physical prehabilitation before transplantation in an individualized manner, using nutritional assessment and the application of indices to assess the frailty of these patients. These activities should be proposed and directed by specialists in rehabilitation and physiotherapy.
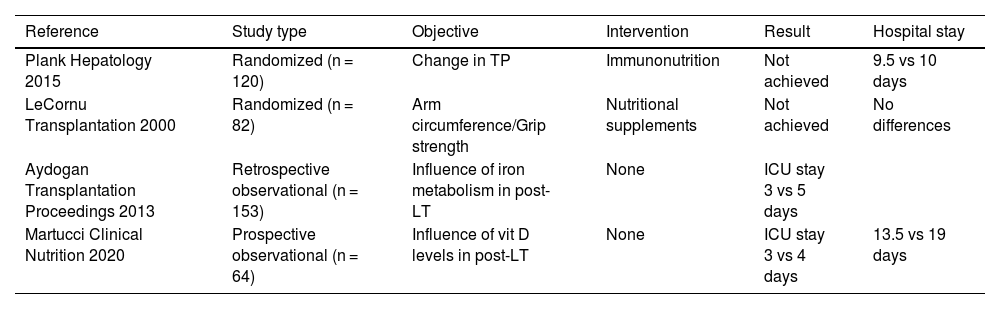
Prehabilitation: nutritionCan systematic nutritional assessment help improve immediate recovery after LT surgery? Could a nutritional intervention in selected patients improve/accelerate recovery after LT surgery?The revision of the ILTS consensus was not conclusive in establishing the role of nutritional support before transplantation in the short-term results after surgery.9 The studies analyzed demonstrated no influence on mortality or the rate of complications (Table 3).10–13
Studies about the assessment and/or nutritional intervention before transplantation.
| Reference | Study type | Objective | Intervention | Result | Hospital stay |
|---|---|---|---|---|---|
| Plank Hepatology 2015 | Randomized (n = 120) | Change in TP | Immunonutrition | Not achieved | 9.5 vs 10 days |
| LeCornu Transplantation 2000 | Randomized (n = 82) | Arm circumference/Grip strength | Nutritional supplements | Not achieved | No differences |
| Aydogan Transplantation Proceedings 2013 | Retrospective observational (n = 153) | Influence of iron metabolism in post-LT | None | ICU stay 3 vs 5 days | |
| Martucci Clinical Nutrition 2020 | Prospective observational (n = 64) | Influence of vit D levels in post-LT | None | ICU stay 3 vs 4 days | 13.5 vs 19 days |
ICU, intensive care unit; TP, total proteins.
The benefits of a supplemental nutritional intervention have not been demonstrated in standard patients. Vitamin D supplements should follow the recommendations given for the general population. The intervention is considered non-detrimental. Evidence/Recommendation: C2
Proposed interventionNutritional assessment is proposed in all patients who are candidates for LT, and the intervention should be considered in patients whose parameters indicate they are either malnourished or overweight. These activities should be proposed and directed by specialists in endocrinology and nutrition.
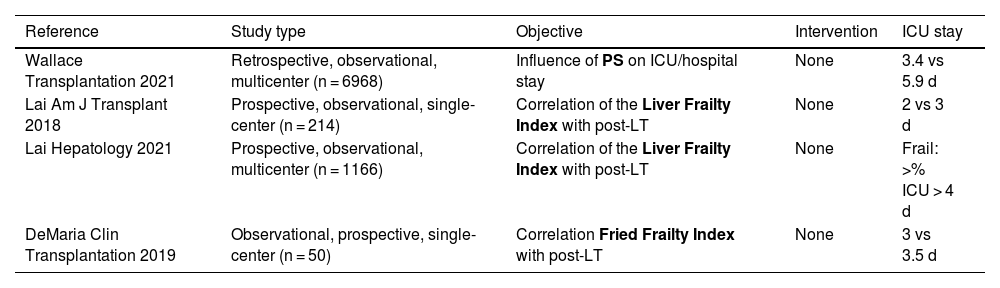
Assessment of patients at riskAre there validated scores that allow us to predict better, faster recovery after LT surgery?There are no validated scores that make it possible to reliably predict the probability of post-LT complications.14 The scores that present some relationship with outcome parameters (such as ICU/hospital stay) are those that evaluate factors like physical function (frailty and performance status) and sarcopenia (Tables 4 and 5).15–23
Summary of fragility/PS studies.
| Reference | Study type | Objective | Intervention | ICU stay |
|---|---|---|---|---|
| Wallace Transplantation 2021 | Retrospective, observational, multicenter (n = 6968) | Influence of PS on ICU/hospital stay | None | 3.4 vs 5.9 d |
| Lai Am J Transplant 2018 | Prospective, observational, single-center (n = 214) | Correlation of the Liver Frailty Index with post-LT | None | 2 vs 3 d |
| Lai Hepatology 2021 | Prospective, observational, multicenter (n = 1166) | Correlation of the Liver Frailty Index with post-LT | None | Frail: >% ICU > 4 d |
| DeMaria Clin Transplantation 2019 | Observational, prospective, single-center (n = 50) | Correlation Fried Frailty Index with post-LT | None | 3 vs 3.5 d |
PS, performance status.
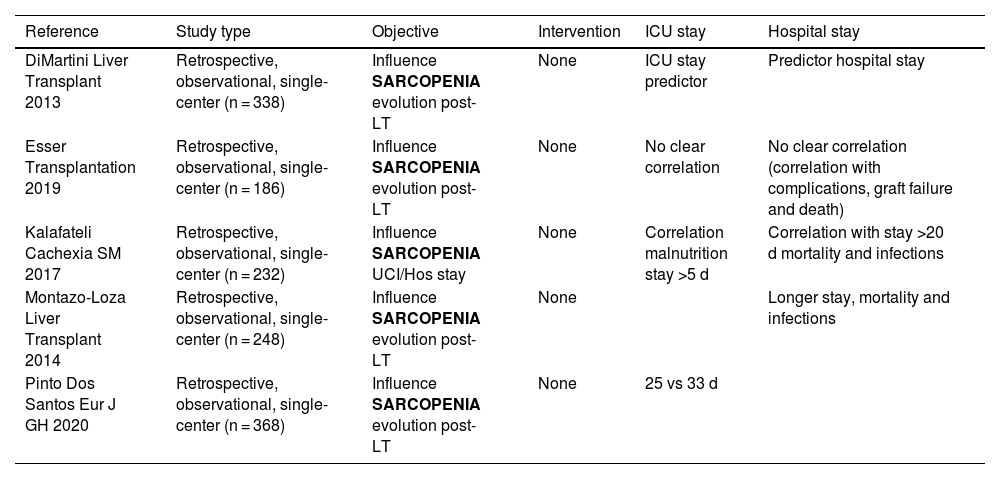
Summary of studies evaluating sarcopenia.
| Reference | Study type | Objective | Intervention | ICU stay | Hospital stay |
|---|---|---|---|---|---|
| DiMartini Liver Transplant 2013 | Retrospective, observational, single-center (n = 338) | Influence SARCOPENIA evolution post-LT | None | ICU stay predictor | Predictor hospital stay |
| Esser Transplantation 2019 | Retrospective, observational, single-center (n = 186) | Influence SARCOPENIA evolution post-LT | None | No clear correlation | No clear correlation (correlation with complications, graft failure and death) |
| Kalafateli Cachexia SM 2017 | Retrospective, observational, single-center (n = 232) | Influence SARCOPENIA UCI/Hos stay | None | Correlation malnutrition stay >5 d | Correlation with stay >20 d mortality and infections |
| Montazo-Loza Liver Transplant 2014 | Retrospective, observational, single-center (n = 248) | Influence SARCOPENIA evolution post-LT | None | Longer stay, mortality and infections | |
| Pinto Dos Santos Eur J GH 2020 | Retrospective, observational, single-center (n = 368) | Influence SARCOPENIA evolution post-LT | None | 25 vs 33 d |
Levels of evidence of pre-LT assessment scores:
Karnofsky Performance Status — Evidence/Recommendation: B2
Liver Frailty Index — Evidence/Recommendation: B1
Fried Frailty Index — Evidence/Recommendation: C2
Measurement of muscle mass using the psoas muscle mass index/total skeletal muscle mass index on L3-L4 computed tomography — Evidence/Recommendation: B1
RecommendationThe evaluation of frailty is mandatory for the assessment of patients who are candidates for LT — Evidence/Recommendation: B1
Proposed interventionA frailty evaluation should be included in the initial assessment of patients who are candidates for LT, and appropriate measures should be adopted based on the results. The recommended scores are those that have a higher degree of evidence in the literature (Karnofsky Performance Status, Liver Frailty Index [in outpatients] and sarcopenia [in hospitalized patients]).
Prehabilitation: pre-transplant anemia controlDoes preoperative anemia control influence recovery after LT?The diverse nature of liver disease, the frequently associated portal hypertension, and the unpredictability of waiting list times are obstacles in the control of pre-transplant anemia.1,2,24–27
RecommendationAn attempt should be made to obtain/maintain adequate hemoglobin (Hb) levels during the waiting list period before the day of the transplant. Hb levels of no less than 10 g/dL are considered optimal. Evidence/Recommendation: B1
Proposed interventionA preoperative patient blood-management program should be developed, and a periodic screening system should be established; target figures should never be less than 10 g/dL, regardless of gender, and anemia treatment measures should be programmed.
Intraoperative periodAnesthetic managementWhat is the optimal anesthesia that manages to improve the immediate and short-term results after LT?Propofol is associated with faster awakening time and less ischemia-reperfusion injury. Some studies show a greater risk of atelectasis, cardiac injury markers and mortality with the use of high O2 concentrations. Low tidal volume ventilation in abdominal surgery is associated with reduced mortality. A specific range of positive end-expiratory pressure (PEEP) cannot be recommended, but recruitment maneuvers improve oxygenation and lung function.28 The benefit/risk ratio of antiemetic prophylaxis is favorable.29
RecommendationsThe use of volatile hypnotic agents is recommended, except in patients at risk of intracranial hypertension. Evidence/Recommendation: C2
The use of the minimum alveolar concentration (MAC) is recommended to measure the depth of anesthesia. Evidence/Recommendation: C2
It is recommended to use inspiratory oxygen concentrations (FiO2) aimed at maintaining PO2 in the range of 70−110 mmHg, tidal volumes between 6−8 mL/kg, and recruitment maneuvers. Evidence/Recommendation: C1
The routine use of antiemetics is recommended. Evidence/Recommendation: C1
Proposed interventionAnesthetic measures that have been reported to improve results after anesthesia (with lower morbidity and mortality rates) should be standardized.
What is the optimal method of anesthetic monitoring that improves immediate and short-term results after LT?Insertion of a transesophageal echocardiogram probe is considered safe in patients with esophageal varices under treatment, as long as variceal ligation has not been performed within the previous 30 days. Hemodynamic monitoring systems based on pulse wave analysis are not useful in patients with advanced liver disease.30
RecommendationsRoutine monitoring of invasive blood pressure and central venous pressure is recommended. Evidence/Recommendation: C1
Systematic ultrasound-guided placement of a high-flow central or peripheral venous catheter under sterile conditions is recommended. Evidence/Recommendation: C1
Monitoring with a pulmonary artery catheter and/or transesophageal echocardiography is recommended in unstable patients and those with high surgical risk and/or known pulmonary hypertension or ventricular dysfunction. Evidence/Recommendation: C1
Transesophageal echocardiography should not be used in patients with a history of variceal ligation in the 30 days prior to transplantation. Evidence/Recommendation: C1
Maintained normothermia is recommended during surgery. Evidence/Recommendation: C1
Proposed interventionSystematic use of a transesophageal echocardiography probe in all patients who do not have contraindications in order to acquire a level of knowledge appropriate for this clinical context.
How do intraoperative transfusion management, antifibrinolytic therapy, and coagulation monitoring influence immediate and short-term results after LT?Hypervolemia temporarily increases the degree of portal hypertension, which increases the risk of bleeding. Patients with chronic liver disease are at a higher risk of developing acute renal failure with the administration of colloids. Viscoelastic tests have been shown to reduce transfusion requirements in the context of bleeding compared to standard coagulation tests. Prophylactic transfusion of blood products has not been shown to be effective to reduce bleeding.31,32
RecommendationsA moderately restrictive fluid administration regimen is recommended. Evidence/Recommendation: C1
The use of 6% 130/0.44 HES is not recommended in patients with chronic liver disease.
Evidence/Recommendation: C1
It is recommended to maintain mean blood pressure values above 60−65 mmHg Evidence/Recommendation: C1
In the case of active bleeding (not massive bleeding), there is no evidence to recommend a specific ratio of blood products. Evidence/Recommendation: B1
The use of a cell saver is recommended. Evidence/Recommendation: B1
Proposed interventionPursue a moderately restrictive fluid approach during the perioperative period, strictly monitoring renal function and peripheral perfusion markers.
What is the role of early extubation in the immediate and short-term results after liver transplantation?There is no consensus on the definition of early extubation. The definitions used in studies range from extubation in the operating room to the first 24 h post-transplant.33
RecommendationsEarly extubation is recommended in all patients where this is possible, given the lower incidence of reintubation, pulmonary complications, shorter ICU stay, and shorter hospital stay. Evidence/Recommendation: C1
Proposed interventionStandardize the definition of early extubation to demonstrate causality and to validate and compare short-term results.
What is the role of perioperative analgesia in the immediate and short-term results after LT?Non-opioid analgesics have been shown to be superior to conventional opioid analgesia for the outcomes of postoperative pain, extubation time, intensive care unit stay, hospital stay, and mortality.34
RecommendationsIt is recommended to minimize the use of opioids in postoperative analgesia. Evidence/Recommendation: B2
The use of acetaminophen (paracetamol), gabapentin, ketamine, and local anesthetics is recommended instead of (or to complement) opioids for postoperative analgesia. Evidence/Recommendation: B2
Proposed interventionStandardize opioid-free multimodal analgesic regimens, which can be evaluated and compared with conventional opioid analgesia.
Surgical techniqueWhat type of surgical technique manages to improve immediate and short-term results after LT?The choice of a certain surgical technique can provide patient benefits, depending on their hemodynamic clinical situation, in terms of intraoperative management and early postoperative recovery. In general, the level of evidence to evaluate these factors is low or very low.
- 1
Hepatectomy technique (cava replacement vs piggy-back technique): The piggy-back technique shortens the duration of the operation and entails less intraoperative transfusion. There are no differences for other parameters.35
- 2
Use of veno-venous by-pass: Even though veno-venous bypass prolongs the surgical intervention and increases transfusion, its use entails reduced cardiovascular instability in patients without collateral portosystemic circulation. However, to minimize technical complications, it is recommended that the anesthetic and surgical team be familiar with its use.2
- 3
Portacaval shunting: Portacaval shunting has shown beneficial intraoperative effects in cases of elevated basal portal flow (≥1000 mL/min) and/or portacaval pressure gradient ≥16 mmHg, with fewer transfused blood units and shorter operation times.36
The surgical technique chosen for the type of cava anastomosis (cava substitution vs piggy-back) should be based on the preferences of each hospital and surgical team. One technique cannot be recommended over another in a systematic manner. Evidence/Recommendation: C1
Veno-venous bypass may be considered in certain situations. It is recommended that the anesthesia/surgery team and the organization be familiar with the technique. Evidence/Recommendation: C1
The temporary portacaval shunt is recommended in cases of severe portal hypertension. Evidence/Recommendation: B1
Proposed interventionIdentify the hemodynamic and anatomical situation of each recipient (portal flow and degree of portal hypertension, presence of portosystemic circulation, inferior vena cava gradient, hepatomegaly) to indicate the surgical technique that benefits intraoperative anesthetic-surgical management.
Do immediate and short-term results after LT improve with the placement of abdominal drain tubes, T-tube in the bile duct, NG tube, skin preparation or incision type?It is recommended to avoid the routine use of drain tubes and catheters. When used, early removal is recommended. The level of evidence is very low due to the lack of randomized prospective studies with sufficient sample size.37–42
RecommendationsThe use of the surgical checklist is recommended for the prevention of adverse events and mortality related to the intervention. Evidence/Recommendation: B1
Routine nasogastric tube placement is not recommended. Evidence/Recommendation: A1
There is insufficient evidence to recommend the routine use of abdominal drain tubes. Open drain systems should be avoided due to the greater risk of infection. Evidence/Recommendation: C2
Early removal of drain tubes is recommended (before the 5th postoperative day), depending on the amount and appearance of the drained fluid. Evidence/Recommendation: B1
Routine/systematic placement of a T-tube is not recommended. Its use could be beneficial in cases of high risk of biliary stenosis. Evidence/Recommendation: C1
Early removal of the central line and urinary catheter is recommended to reduce catheter infections. Evidence/Recommendation: C1
The type of incision used is left to the discretion of the surgeon. Evidence/Recommendation: B1
Proposed interventionIn all cases, systematic collection of these variables is recommended to establish in the future the actual influence of their application on postoperative morbidity, mortality and hospital stay.
What is the role of perfusion machines in improving the immediate and short-term results of the liver graft and recipient?- a)
Regional normothermic perfusion in non–heart-beating donation reduces ischemia time, provides for evaluation of the grafts, and decreases the rates of post-transplant ischemic biliary complications.43
- b)
Both hypothermic (HMP) and normothermic (NMP) perfusion machines have been shown to be beneficial in the prevention of post-reperfusion syndrome and primary graft dysfunction, specifically for suboptimal grafts.44
- a)
The use of regional normothermic perfusion is recommended during extraction in non–heart-beating donation due to its beneficial effect on the initial graft function. Evidence/Recommendation: C1
- b)
It is recommended to assess the role of dynamic preservation with ex situ perfusion machines in suboptimal grafts. Evidence/Recommendation: C1
In the extraction of donors in cardiorespiratory arrest, the use of regional normothermic perfusion (RNP) is recommended instead of super rapid extraction.
Assessment of the progressive implementation of dynamic preservation with perfusion machines is recommended in order to define in which cases their use will provide benefits compared to standard perfusion.
Postoperative periodPost-transplant nutritionDoes early postoperative nutrition influence the recovery of patients undergoing LT?The European Society for Clinical Nutrition and Metabolism (ESPEN) and the European Association for the Study of the Liver (EASL) recommend starting nutritional intake 12−24 h after surgery to reduce the risk of complications and hospital stay after transplantation.37,45–50
The ESPEN guidelines recommend the intake of 1.2–1.5 g protein/kg of body weight in within 24 h of liver transplantation.51
Recommended interventionOral and/or enteral nutrition should be started 12−24 h after liver transplantation, depending on patient tolerance. The nutritional objective should emphasize achieving adequate protein intake as part of the overall energy needs. Evidence/Recommendation: C1
There is no clear evidence of the benefit of nutritional supplements after LT. Evidence/Recommendation: C1
Proposed interventionOral and/or enteral nutritional support is started within hours of transplantation.
Parenteral nutrition will be reserved for patients in whom the calorie and protein intake necessary to maintain adequate nutritional status is not sufficient.
Postoperative rehabilitationHow does early mobilization and respiratory rehabilitation influence the recovery of patients undergoing LT?A recent study has shown a decrease in muscle strength and exercise tolerance at discharge after LT.52 The benefits of physical and respiratory rehabilitation after surgery have been demonstrated and influence factors of postoperative recovery, such as pain reduction, prevention of deep vein thrombosis and pulmonary thromboembolism, reduction in the incidence of atelectasis and respiratory complications, in addition to improvement in the psychological status of the patient.6,37,53–55
RecommendationEarly mobilization should be started as soon as possible after LT.
Evidence/Recommendation: B1
Respiratory rehabilitation is recommended because it is safe and effective, reduces postoperative complications and improves functional results.
Evidence/Recommendation: B1
Proposed interventionEstablish a protocol for early mobilization and directed respiratory rehabilitation with the help of incentive spirometry in the immediate postoperative period.
The patient will begin walking while hospitalized and later start physical rehabilitation after hospital discharge.
Vascular monitoring and thromboprophylaxis managementA previous SETH2 consensus document has established recommendations for this management.
Immunosuppression managementWhich immunosuppressive strategy achieves better short-term results in patients undergoing LT?The implementation of an intensive pharmacokinetic monitoring program and the dose calculation based on the Bayesian estimation provide for individualized immunosuppression adjustments.6,54 Several studies have evaluated the delayed start of calcineurin inhibitors (CI) associated with induction therapies aimed at preserving renal function, with no associated increase in episodes of acute rejection.18,56
RecommendationIntensive pharmacokinetic monitoring and its adjustment by Bayesian estimation allow for early optimization of immunosuppression, favor enhanced recovery, and enable early discharge. Evidence/Recommendation: B1
Immunosuppression strategies should be aimed at reducing its adverse effects. Evidence/Recommendation: B1
Delayed start of immunosuppression with IC (+/− ARIL-2) can help reduce minimize its adverse effects (especially nephrotoxicity). Evidence/Recommendation: C1
Proposed interventionsThe use of immunosuppression regimens based on low doses or delayed introduction of tacrolimus associated with ARIL-2 induction is recommended in patients at risk of kidney injury and in combination with dual or triple therapy with corticosteroids and/or MMF.
Antimicrobial prophylaxisWhat is the optimal antimicrobial prophylaxis to prevent postoperative infectious complications after liver transplantation?When selecting the appropriate antimicrobial to prevent bacterial infections, it is necessary to consider the clinical conditions of each patient, local epidemiology, and resistance patterns.57
RecommendationAntibiotic prophylaxis against bacterial infections must be protocolized, and its duration should not routinely exceed 24 h. Evidence/Recommendation: B1
The choice of antimicrobial should be individualized according to the microbiota and specific characteristics of each transplant center. Evidence/Recommendation: B1
Proposed interventionsAntibiotic prophylaxis for the first 24 h after transplantation against bacterial infections with choice of antimicrobial based on local epidemiology and the presence of colonization by multi-resistant germs in the donor and/or recipient.
Other factors will be considered in order to individualize the therapy regarding surgical technique and/or clinical status of the transplanted patient.
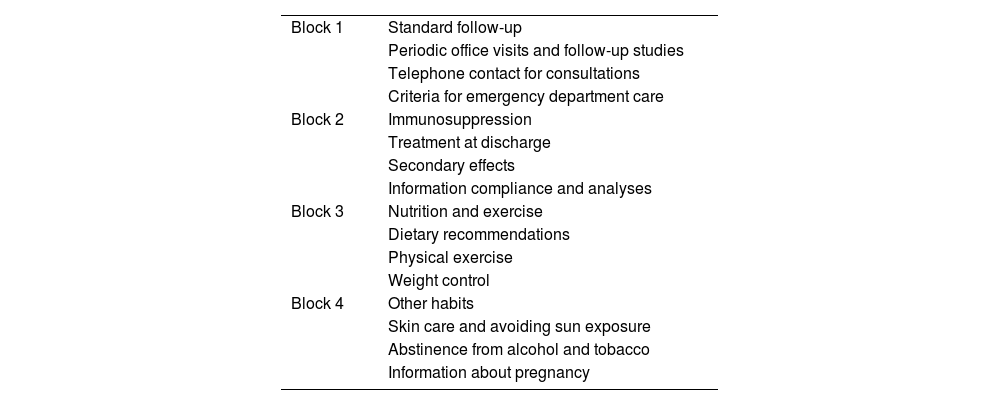
Post-transplant educationDoes post-transplant education influence the clinical evolution of patients undergoing LT?Systematic education programs in the postoperative period after liver transplantation can help increase or reinforce the knowledge of patients and family members in terms of their new transplant condition. These programs should be multidisciplinary.6,37
RecommendationSystematic education in the postoperative period after liver transplantation helps reinforce the patient's knowledge of their new transplant condition. These programs continue the educational process that was begun in the preoperative period and should continue during long-term post-transplantation follow-up. Evidence/Recommendation: C1
Proposed interventionsDetailed information should be offered to the patient and caregiver(s) during hospital discharge by multidisciplinary specialists (surgeon, rehabilitator, home hospitalization, advanced practical nursing). Establish a check-list model for home compliance with pharmacological treatment (especially immunosuppressants), diet and rehabilitation. (Example in Table 6)
- -
Mobile application for warning / resolution of unforeseen events
- -
Workshops for transplant patients given by long-term transplant patients and staff members of the LT program
Information checklist for post-transplant hospital discharge.
| Block 1 | Standard follow-up |
| Periodic office visits and follow-up studies | |
| Telephone contact for consultations | |
| Criteria for emergency department care | |
| Block 2 | Immunosuppression |
| Treatment at discharge | |
| Secondary effects | |
| Information compliance and analyses | |
| Block 3 | Nutrition and exercise |
| Dietary recommendations | |
| Physical exercise | |
| Weight control | |
| Block 4 | Other habits |
| Skin care and avoiding sun exposure | |
| Abstinence from alcohol and tobacco | |
| Information about pregnancy |
The recommendations of this consensus document are based on a multidisciplinary approach and the available scientific evidence, which is very limited. The recommendations are linked to a series of proposed interventions to facilitate their application. The implementation of these recommendations inescapably requires the commitment of all the members of the LT teams, as well as each institution.
Each group at each transplant center will manage the options, possibilities and factors that may facilitate its implementation:
- 1
Restructure resources and/or acquire new resources, if necessary.
- 2
Establish a registry for this activity, preferably integrated into the hospital computer system. To this end, checklists can be particularly useful.
- 3
Establish an auditing system of indicators to determine compliance with the protocol and results.
L.L.L., M.A., A.B., R.G, E.M, S.P., G.R. han contribuido en la concepción y diseño de la revisión, han participado en la redacción del trabajo y su revisión crítica y han aprobado el contenido final. Por otra parte han actuado como coordinadores del panel de la reunión de consenso de la Sociedad Española de Trasplante Hepático.
FundingThis research has not received specific support from public sector agencies, commercial sector or non-profit entities.
Conflict of interestsThe authors declare that they have no conflict of interest in relation to this work.
AcknowledgmentThe consensus group thanks Paloma Bellés of AOPC for her contribution with secretarial work and technical support.
Félix Alegre (Clínica Universitaria de Navarra), Carolina Almohalla (H. U. Río Hortega), Pablo Bellot (H. Gral. U. de Alicante), Gerardo Blanco (H. U. Badajoz), Rubén Ciria (H. U. Reina Sofía), Gonzalo Crespo (H. U. Clínic i Provincial), Juan Echeverri (H. U. Marqués de Valdecilla), Carmen García Bernardo (H. U. Central de Asturias), Marta García Guix (H. U. de Bellvitge), Miguel Angel Gómez Bravo (H. U. Virgen del Rocío), Ernest Hidalgo (H. U. Vall d'Hebrón), Loreto Hierro (H. U. La Paz), Carmelo Loinaz (H. U. 12 de Octubre), Víctor López (H. U. Virgen de la Arrixaca), José Luis Lucena (H. U. Puerta de Hierro Majadahonda), José M. Morón (H. U. Son Espases), Javier Nuño (H. U. Ramón y Cajal), Elena Otón (H. U. Nuestra Sra. de la Candelaria), Pilar Palacios (H. Clínico U. Lozano Blesa), Mikel Prieto (H. U. de Cruces), Mario Romero (H. Gral. U. Gregorio Marañón), Julio Santoyo Villalba (H. Reg. U. de Málaga), Evaristo Varo (H. Clínico U. de Santiago), Maria Angeles Vázquez (H. U. A Coruña), Juan José Vila (H. U. La Fe Infantil), Trinidad Villegas (H. U. Virgen de la Nieves), Carmen Vinaixa (H. U. La Fe).
El listado completo del panel de participantes representantes de los grupos nacionales de Trasplante Hepático se incluyen en la sección de agradecimientos.
Please cite this article as: L Lladó, Usera MA, Blasi A, Gutiérrez R, Montalvá E, Pascual S, et al. Documento de consenso de la Sociedad Española de Trasplante Hepático. Recuperación intensificada en trasplante hepático. Cir Esp. 2024;102:104–115.
This article has been copublished with permission in Gastroenterología y Hepatología and Cirugía Española.