Endoscopic procedures for the treatment of obesity have generated a growing interest in both patients and surgeons in recent years. They have been proposed as a less invasive alternative to conventional bariatric surgery in individuals who prefer not to undergo high-risk surgical interventions and in whom weight loss has failed after lifestyle modifications. The primary obesity surgery endoluminal (POSE) procedure is a technique on the rise. However, even though it is being increasingly implemented by endoscopists, this procedure is not free from potentially serious complications for patients.
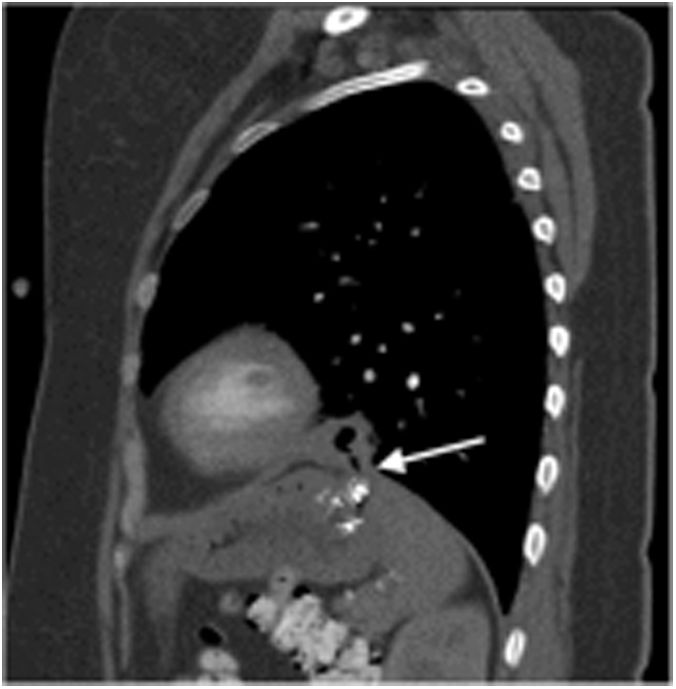
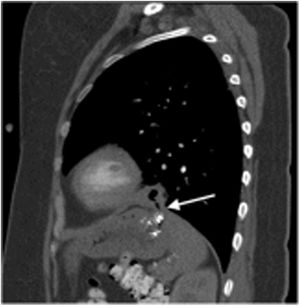
We present the case of a 34-year-old woman with grade I obesity and no history of interest who had undergone an endoscopic procedure for weight loss using the POSE technique. The patient had previously presented some isolated vomiting that had already subsided. Ten days after surgery, she came to the emergency room due to fever and non-productive cough that had been progressing for 2 days. Physical examination was normal, and laboratory tests only identified mild leukocytosis with neutrophilia. A chest X-ray showed left basal condensation. A thoracoabdominal computed tomography (CT) scan revealed a 26 × 30 × 17 mm ground-glass image with inner air bubbles in the anterior basal segment of the left lower lobe (LLL), which was associated with a small break in continuity in the left hemidiaphragm adjacent to the gastric fundus (Fig. 1). The patient was admitted to hospital, and intravenous antibiotic treatment was administered for 10 days. An upper gastrointestinal endoscopy and contrast study were requested; both tests were normal. A new chest CT scan showed a decrease in the size of the abscess in the LLL, and the diaphragmatic break in continuity was no longer observed, so the patient was discharged from the hospital 11 days after admission. She continues to be followed up in the clinic and is asymptomatic, with no signs of recurrence 14 months later.
The POSE procedure involves creating a series of folds in the gastric wall endoscopically with special suture anchors, specifically in 8 to 9 points of the gastric fundus and 3 to 4 of the distal part of the body1. The objective is to reproduce the changes that restrictive bariatric surgery causes in the gastric anatomy and physiology. In addition to reducing the total gastric volume, physiological changes have been demonstrated, such as delayed gastric emptying, which results in early and prolonged satiety2. Espinós et al.1 published a first series of cases in 2013. In a sample of 45 patients, they reported abdominal pain (33.3%) and nausea (13.3%) as the most frequent complications. They also described a single case of postoperative fever that resolved with oral antibiotic treatment, but without specifying the focus or origin.
To date, only two randomized clinical trials have been conducted on POSE2. The MILEPOST3 study was a European multicenter randomized clinical trial published in 2017, in which the only complication was postoperative bleeding (reported in two patients). The ESSENTIAL4 study was also published in 2017, and it was also a randomized clinical trial carried out in the US, in which the reported rate of total adverse effects was 5%, the most frequent being nausea (1.8%) and vomiting (1.8%).
To the best of our knowledge, this is the first description in the literature of pneumonia due to gastro-pleural fistula after the POSE procedure.
‘Minimally invasive’ endoscopic techniques like endoscopic tubular gastroplasty or POSE are proposed as an alternative for those patients with grade I or II obesity who cannot or do not wish to undergo resective surgery. Although these types of procedures are usually performed on an outpatient basis, close and early patient follow-up is necessary after discharge, mainly during the first 7 to 10 days, which is the period in which the main complications of the technique could appear.
A gastro-pleural fistula can cause a serious, life-threatening infection. Nevertheless, we can opt for conservative management with antibiotics and restriction of oral intake in patients who are stable and oligosymptomatic, as in the case described. It is important for surgeons to have knowledge about both the technique and the possible complications, as the definitive treatment of some cases may involve surgical management if conservative therapy fails.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: López-Fernández J, García-Plaza G, García-Quesada SM, Fernández IA, Hernández-Hernández JR. Manejo conservador de fístula gastro-pleural tras procedimiento POSE (primary obesity surgery endoluminal). Cir Esp. 2022;100:381–382.