Laparoscopic surgery is a successful treatment option offering significant advantages to patients compared with open ventral hernia repair. A cost–benefit analysis was performed to compare the clinical results and economic costs of the open and laparoscopic techniques for anterior abdominal wall hernia repair, in order to determine the more efficient procedure.
Materials and methodsWe performed a prospective study of 140 patients with primary and incisional hernia, and analyzed clinical data, morbidity, costs of surgery and hospital stay costs.
ResultsThe cost of disposable surgical supplies was higher with laparoscopic repair but reduced the average length of stay (P<.001) and patient morbidity (P<.001). The total cost of the laparoscopic procedure was, therefore, less than initially estimated, yielding a savings of 1260€ per patient (2865€ vs 4125€).
ConclusionsLaparoscopic ventral hernia repair is associated with a reduced complication rate, a lower average length of stay and with lower total costs. Laparoscopic repair can save 1260€ for each patient, and so this procedure should be considered a cost-effective approach.
La laparoscopia ofrece importantes ventajas clínicas respecto a la técnica abierta en la reparación de las hernias de pared abdominal. Se realiza un estudio coste-beneficio con el objetivo de analizar los resultados clínicos y los costes económicos comparando la técnica abierta y la laparoscopia en la reparación de la hernia de pared anterior abdominal y así determinar el procedimiento más eficiente.
Material y métodosEstudio prospectivo de cohortes sobre 140 pacientes consecutivos con hernias ventrales, con el objetivo de evaluar el coste de ambas técnicas. Se analizan datos clínicos, morbilidad, estancia hospitalaria, complicaciones y costes.
ResultadosLa vía laparoscópica presentó menor estancia media (p<0,001), menor morbilidad postoperatoria y complicaciones (p<0,001) y reducción en la tasa de reingresos. El coste del material laparoscópico fue más alto, aunque el coste total del procedimiento por paciente fue menor (2.865€) vs reparación abierta (4.125€).
ConclusionesLa reparación laparoscópica de las hernias ventrales de pared abdominal aporta beneficios para los pacientes y presenta, además, un coste final del procedimiento sensiblemente menor, evitándose un gasto de 1.260€ por cada paciente intervenido por esta vía. Además de ser una técnica eficiente, la reparación laparoscópica es coste-efectiva.
Laparoscopy has become an alternative approach for many surgeries. Since its development in 1990, it has brought about a transformation of multiple procedures by progressively demonstrating its advantages over the open approach.
These benefits arise from its less invasive nature on the patient's abdominal wall, which reduces pain during surgery, thus requiring less analgesia during the surgery phase, less postoperative pain, lower morbidity, and a reduction in the rate of ventral hernias.1–4 With regard to work and social aspects, it also has advantages, such as better postoperative recovery, earlier return to usual activity, decrease in the loss of working days,2,5 and therefore, a financial benefit to health systems.
Cholecystectomy was the first procedure to use laparoscopy, and laparoscopic cholecystectomy has become the “gold standard”.2 The open approach has become the exception, used only in complex cases and in conversions. However, ventral hernia repair has been one of the last conditions to incorporate laparoscopic access. This is due mainly to the particular difficulties posed by the separation of adhesions, with the possibility of inadvertent bowel lesion, and it can even cause death without the proper experience.6
LeBlanc7 published a study with long-term results of over 10 years of follow-up, which demonstrates the superiority of laparoscopic ventral hernia repair based on improving patient recovery and reducing the rate of complications and infections by less handling of the mesh. It also discloses a lower recurrence rate than open surgery.8,9
Moreover, from the perspective of sustainability and cost containment, it must be considered that a health system needs to introduce a new public funded technique when cost–benefit studies are available that can demonstrate, not only its efficacy, but also the efficiency of its use. There are some studies on laparoscopy showing clear hospital cost and work2,5 related financial advantages.8,10,11 However, all were performed after it was accepted.
In our setting, studies have been published on cost effectiveness for inguinal hernias12 and primary hernias repaired by an anterior approach by comparing the types of anesthesia.13 No studies were found to assess the level of efficiency of laparoscopic surgery of the anterior abdominal wall, which would be greatly useful to assess the cost of funding that this prevalent condition may represent for the health system.
This work aims to perform a cost–benefit study to compare anterior abdominal wall hernia repair by open surgery with the laparoscopic approach, in order to determine whether the clinical and financial benefits of laparoscopic surgery outweigh those of conventional surgery, thus determining if it is more efficient than the conventional procedure.
Materials and MethodsA controlled non-randomized cohort prospective study was performed on 140 consecutive patients operated at the Servicio de Cirugía General y Digestivo del Hospital Universitario de Getafe de Madrid [Department of General and Digestive Surgery, University Hospital of Getafe in Madrid] (Spain), who were diagnosed with ventral abdominal wall hernia. The study period included from January 2004 to January 2009.
Inclusion CriteriaAdult patients with normal mental capacity, and elective surgical indication for the following hernias, classified according to the EuraHS Working Group14:
- -
Primary midline ventral hernias: umbilical, epigastric, both, or Spiegel, with size at scan greater than 3cm in transverse diameter or less than 3cm in patients with body weight index greater than 30.
- -
Ventral incisional hernias with transverse diameter less than 20cm, which would not require related dermolipectomy or other skin correction techniques.
No additional radiological scans were performed, unless for other indications.
Patients were divided into 2 groups controlled prospectively. Allocation was performed randomly by the attending surgeon during the abdominal wall-specific outpatient clinic of the department. Open surgery was performed by 2 abdominal wall experienced surgeons, and the laparoscopic procedure by 2 who had training in this technique. Resident doctors usually assisted, but were in the operating surgeon of 7 patients who underwent the open approach, and 5 with the laparoscopic procedure.
We considered that 140 patients represented our population statistically, given the incidence of this disease.
Surgical Technique- 1.
Laparoscopic Repair (LAP): 70 patients. The procedure was always performed under general anesthesia and anesthetic infiltration with bupivacaine 0.25% in the incisions. A direct optical trocar was introduced through the left upper quadrant at the subcostal level, except for the first 10 cases, where open access was used with a Hasson trocar. Access to the cavity was verified and the pneumoperitoneum was created. A second 5mm working port was placed, and a third one, if needed in the left abdomen, mid-clavicular line, when adhesions were present. If dissecting adhesions was not required, only the 10mm working channel was used for optical instruments and the 5mm one to introduce grasping instruments. All possible defects were identified, releasing 5–6cm of aponeurosis around them and throughout the circumference. The round ligament was separated for supraumbilical hernias and Retzius space for infraumbilical hernias, if necessary. We used ePTFE DualMesh® (Gore-Tex®, Flagstaff, AZ, USA), adequately sized to facilitate over 5cm of overlap around the defect. For incisional hernias, the entire incision was not covered, but the defect was repaired with 5cm of overlap. For cases with 2 defects within the same anatomical area, only one mesh was used to cover the entire area with the same upper and lower overlap criteria. Four to six transaponeurotic 2/0 Gore-Tex® sutures were used, knotted in the mesh and extracted by contraincision in the abdominal wall through a grommet in the 4 corners knotted subcutaneously, with the dual purpose of centering the mesh correctly over the defect and using it as fixing, besides applying non-absorbable titanium helical staples (Protack®, United States Surgical Co., Norwalk, CT, USA), based on the double crown technique, positioning the clamps 1.5cm apart from each other in the 2 circumferences. No drains were left, except for cases of bleeding or bowel suture.
- 2.
Open repair group (AB): 70 patients. We used the Rives-Stoppa technique, with either general or regional anesthesia. After opening the skin and subcutaneous tissue, the defect is separated without opening the peritoneal sac, unless the need for adhesiolysis was suspected. The rectus sheath was opened 1cm from the midline and the posterior sheath was closed with continuous suture whenever possible with long-lasting 0 polyglycolic acid. The defect was repaired with polypropylene monofilament mesh weighing less than 80g/m2 and macroporous with pore exceeding 1mm, in the prefascial retromuscular location, with overlapping of over 5cm larger than the defect. Fixing was performed with 2–3/0 polypropylene transaponeurotic sutures, 4–6 in number, located in all four corners. The anterior sheath was closed with 0 long-lasting polyglycolic acid absorbable suture in any defect segment allowing it. Suction drains were placed in meshes exceeding 10cm and they were removed at 24–48h or when debit flow was less than 40ml/day.
In both groups, a compressive dressing was placed in the operating room, which was replaced before discharge or at 24h, and an elastic corset was recommended for one month. Antibiotic prophylaxis with 2g of cefazolin IV was administered in a single dose during induction, and antithrombotic prophylaxis with enoxaparin 40mg sc according to hospital protocol, for which a dose is kept every 24h until discharge, confirming the patient's early mobilization and adequate ambulation.
Data collected included age and sex, level of obesity identified according to body mass index, type of hernia (primary or incisional), anatomic location, the transverse diameter of the defect in cm and mesh size used, postoperative morbidity, and readmission, if it occurred.
The cost analysis included the amounts for hospital stay, and materials used directly, divided by the type of procedure. These are the items that are considered to vary significantly depending on whether open or laparoscopic repair is used. Personnel costs are not included, because they are fixed, neither are the costs charged for equipment, because at this point, our facility lacks data for each surgery.
The cost of hospital stay was evaluated considering the DRG 159 (hernia different to inguinal hernia with complications) or DRG 160 (uncomplicated) and their cost through cost accounting analysis in our center, which is €575 and €566/day, respectively. The final cost of the total stay was obtained by multiplying the number of days of stay in each case, by the cost of day depending on whether or not there were any complications. Stay for readmission cases due to complications was calculated using DGR 159.
The costs of the meshes, sutures, drains, laparoscopic trocars and mechanical sutures were obtained from the Supply Department, based on the price for each product at the time of the study (November 2011).
Statistical analysis was performed based on quantitative variables (age, average length of stay, cost, defect diameter) and qualitative variables (sex, complications, obesity [considered as body mass index>30], anatomical location and type of hernia).
The technique used for statistics was based on univariate analysis of data, with the qualitative variables expressed in percentage using SPSS®12.01 (SPSS Inc., Chicago, IL, USA). They were compared with the Chi-square test, applying the Fisher test if n<5 in any of the groups. Quantitative variables are expressed as mean±standard deviation and compared with the Student t test.
P values less than .05 were considered statistically significant.
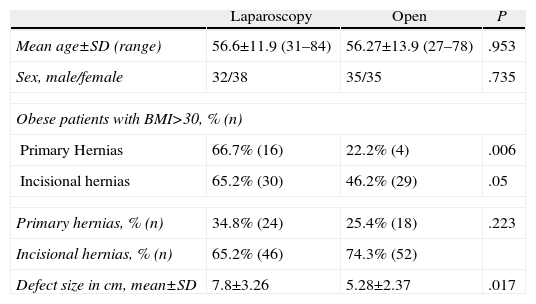
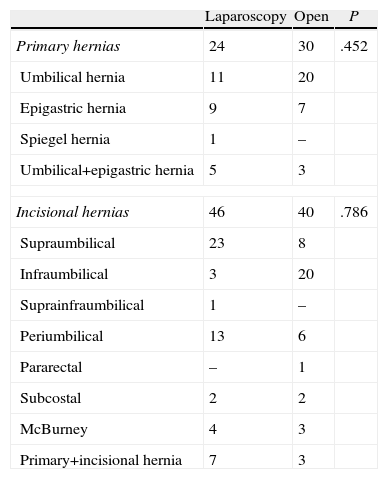
ResultsThe results for demographic and clinical data such as age, sex, degree of obesity, or type of hernia (primary or incisional) are shown in Table 1, resulting in homogeneous groups (P=ns). The size of the defect calculated as transverse diameter in cm was higher in the LAP group than in the AB group (P<.017). The site of the hernia is described in Table 2, with a non-significant difference of a greater number of supraumbilical hernias in the LAP group and infraumbilical hernias in the AB group, not due to any induced selection.
Patient Demographic and Clinical Results.
| Laparoscopy | Open | P | |
| Mean age±SD (range) | 56.6±11.9 (31–84) | 56.27±13.9 (27–78) | .953 |
| Sex, male/female | 32/38 | 35/35 | .735 |
| Obese patients with BMI>30, % (n) | |||
| Primary Hernias | 66.7% (16) | 22.2% (4) | .006 |
| Incisional hernias | 65.2% (30) | 46.2% (29) | .05 |
| Primary hernias, % (n) | 34.8% (24) | 25.4% (18) | .223 |
| Incisional hernias, % (n) | 65.2% (46) | 74.3% (52) | |
| Defect size in cm, mean±SD | 7.8±3.26 | 5.28±2.37 | .017 |
Anatomical Location of Hernia.
| Laparoscopy | Open | P | |
| Primary hernias | 24 | 30 | .452 |
| Umbilical hernia | 11 | 20 | |
| Epigastric hernia | 9 | 7 | |
| Spiegel hernia | 1 | – | |
| Umbilical+epigastric hernia | 5 | 3 | |
| Incisional hernias | 46 | 40 | .786 |
| Supraumbilical | 23 | 8 | |
| Infraumbilical | 3 | 20 | |
| Suprainfraumbilical | 1 | – | |
| Periumbilical | 13 | 6 | |
| Pararectal | – | 1 | |
| Subcostal | 2 | 2 | |
| McBurney | 4 | 3 | |
| Primary+incisional hernia | 7 | 3 | |
Morbidity occurred in 3 patients (4.2%) in the LAP group, and included one prolonged postoperative ileus, another case of local pain caused by helical suture that yielded to analgesics at 3 months, and finally, a tension hematoma in the sack due to the use of anticoagulants. There were no infections. The patient with ileus required readmission. There were no conversions to open surgery in these patients.
In the AB group, there were 13 (18.5%) patients with morbidity: one skin necrosis, 2 pneumonias, 7 abdominal wall infections, 2 hematomas, and one paralytic ileus. Three patients required a hospital readmission, 2 due to infection requiring intravenous antibiotics, and the third one resulting from a major hematoma that required a reoperation to drain and clean the wound.
The risk of complications with open surgery was 4.4 times higher than with laparoscopy (18.5% compared to 4.2%) (OR 4.4), and the difference between the two groups was significant in terms of total morbidity and wall infection (P<.001), which led to a greater number of readmissions and increased hospital stays.
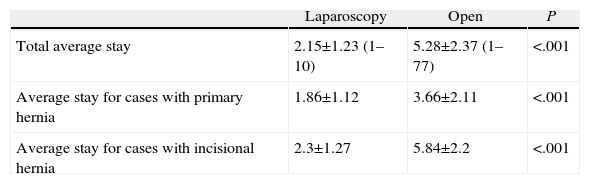
The average stay is shown in Table 3, with a significantly lower total mean stay in the LAP group of 2.15 days, compared to 5.28 days in the AB group, a difference that achieved statistical significance (P<.001). If we analyze the stay in the 2 groups for primary and incisional hernias, the results in both cases are much more positive for the LAP group (P<.001), where hernia defects were larger. Patients with incisional hernias benefited the most, as the reduction in the average stay for these cases is much more relevant for laparoscopic surgery.
Average Stay.
| Laparoscopy | Open | P | |
| Total average stay | 2.15±1.23 (1–10) | 5.28±2.37 (1–77) | <.001 |
| Average stay for cases with primary hernia | 1.86±1.12 | 3.66±2.11 | <.001 |
| Average stay for cases with incisional hernia | 2.3±1.27 | 5.84±2.2 | <.001 |
The average stay is expressed in days±SD, and range, in parentheses.
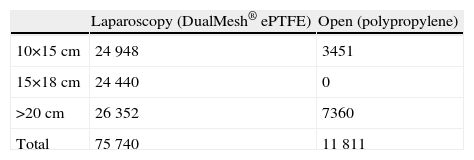
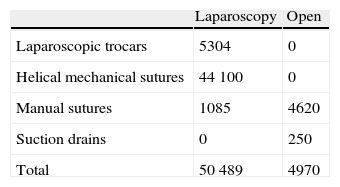
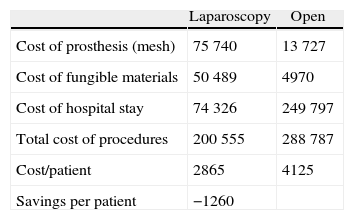
Table 4 shows the cost of the prosthesis (mesh) used by size, and Table 5 lists the amount for all other disposable surgical materials used in the two groups. Compared to open surgery, the higher cost of materials in laparoscopic surgery is remarkable, resulting from the use of helical fixing staplers and the work trocars. The surgical instruments used for the 2 cases were reusable and were not included in the cost calculation.
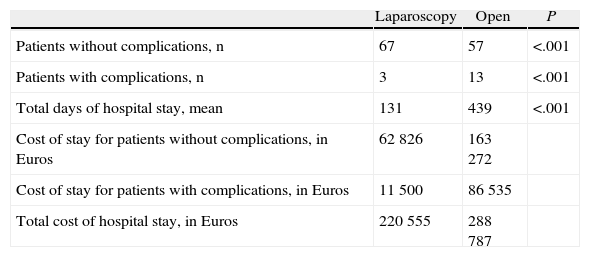
Hospital stay costs were significantly less (P<.001) in the LAP group as a result of the reduction of the average stay and the lower rate of patients with complications (Table 6).
Patients With and Without Complications and Cost Per Hospital Stay.
| Laparoscopy | Open | P | |
| Patients without complications, n | 67 | 57 | <.001 |
| Patients with complications, n | 3 | 13 | <.001 |
| Total days of hospital stay, mean | 131 | 439 | <.001 |
| Cost of stay for patients without complications, in Euros | 62826 | 163272 | |
| Cost of stay for patients with complications, in Euros | 11500 | 86535 | |
| Total cost of hospital stay, in Euros | 220555 | 288787 |
Comparative final data on costs analysis are shown in Table 7, noting that costs for the mesh and disposable materials in the LAP group are higher than in the AB group, but the cost of the whole process per patient operated in the LAP group is lower (€2865) than that in the AB group (€4125).
DiscussionThe introduction of new technologies entails in most cases more expensive health care, and laparoscopy is no exception to this statement. Therefore, the procedure's costs must be taken into account before widely incorporating it into a health system's services portfolio to ensure that it produces results and that it is also practical.2,10,11 It must be considered that using it without checking its financial benefits could lead to an unaffordable increase of health costs, and this would hinder health care sustainability within the historic context of the current financial crisis environment.
There are agencies that analyze different surgical procedures, such as the National Institute of Clinical Excellence in the United Kingdom, which has analyzed the laparoscopy option, among others, comparing it to open surgery for inguinal hernia. This analysis has proven laparoscopy to be cost-effective12,15 when compared with non-mesh repair, when taking into account earlier return to work and reduced recurrences, a fact that reduces the cost by 10%–15%.16 Other revisions, such as Cochrane's,17 fail to provide equally definitive results; however, they evidence the superiority of laparoscopy, although for short-term studies. These experts should shoulder the responsibility of a professionalized study before it is funded by the health system, in order to obtain a rationalization of resources.10,18
The advantages of laparoscopy have been visible since laparoscopic cholecystectomy was introduced in 1993, a technique that has become the “gold standard” for the treatment of cholelithiasis.6,19,20 The cost reduction for laparoscopic colectomy21,22 and bariatric surgery for obesity has also been demonstrated, as well as its greater benefits for recovery of obese patients, due to shorter hospital stay and reduced postoperative complications.23 This is the reason obese patients are the ones benefiting the most from abdominal wall laparoscopic hernia repairs,17 and for using this criteria to include primary hernias under 3cm in our series.
For anterior abdominal wall hernias, and especially, incisional hernias, there is also a possibility of discovering unsuspected hernias, by being able to explore the entire abdominal wall without expanding incisions that increase risk. As with the exploration of the bilateral inguinal region, detecting another defect and correcting it, at the same time, avoids neglected hernias, which are diagnosed subsequently as incisional hernias and require subjecting the patient to a new surgery.3 Some authors have applied the laparoscopic approach to the most difficult cases, such as resurgery patients and those with previous recurrences4,8; therefore, there may be a bias when interpreting the results. In our case series, and in both groups, surgeons who performed the techniques were experts in abdominal wall surgery; therefore, we cannot attribute the existence of any bias in this aspect that has influenced the results.13
The lower requirement of analgesics and morphine, intraoperatively and postoperatively, improves the patient's functional recovery, facilitating an earlier reinstatement to the patient's usual activity and shorter sick leave.5,18
In our series, patients had the same demographic and location characteristics, although the defects were larger in the laparoscopic repair group (P<.001), and also for mesh size. Infectious complications developed at the abdominal wall were lower (P<.001), and so was the total rate of morbidity. Other authors describe these same results,20,24 confirming that this technique provides a lower rate of hematomas, infections and relapses,25 justifying the lower incidence of infection (0%–3%) due to the lower amount of tissue dissection, minimal manipulation of the mesh and the absence of contact with the skin, which prevents its contamination.1,3,7,8,26 The number of patients with complications and readmissions has been higher for open surgery (P<.001), significantly increasing the number of hospital stays in this group (P<.001) in primary hernias and, to a greater extent, for incisional hernias (P<.001).
The reduction in the occurrence of incisional hernias is due to the minimal lesion of the abdominal wall. The described recurrence rate is 2.5% during a 2-year follow-up,4 a very low rate even including the described recurrence compared with the Stoppa technique of 4%–18%,27 which is the lowest of the open techniques. However, studies exceeding 10 years must be continued to determine long-term results.7,28
This study has confirmed that the materials for the laparoscopic procedure are more expensive than for the open approach, as it requires endoscopic technology2 and the use of disposable instruments or disposable materials (trocars, staplers, cautery system, and mesh). This cost can be reduced if surgical instruments such as reusable forceps or scissors are used, as some authors have shown,4,11,13,29 changing from £790 to £170. Champault was able to drop the cost of cholecystectomy30 from €560 to €330 with simple measures.
The mesh we used for endoscopic repair has been double-layer ePTFE, with a peritoneal face that prevents adhesions and an antiseptic that prevents infection. Although its price may be higher than others, the experience to date has shown that it is the safest material for intraperitoneal placement, avoiding bowel fistulas and adhesions, which are the most serious problems related to the placement of a mesh on that site.31–33 Exceptionally, problems have been reported with this type of mesh; therefore, we understand that patient safety compensates for the price difference. Currently, another type, “composite” or “bilamellar” mesh, is being researched, which could provide optimal results in the future.
Laparoscopic surgery time is also important in terms of operating room costs, and depends on the surgeon's experience. Initial cases require longer surgical times; it is reduced proportionally to the learning curve with training and perfecting the technique, which is set on 50 operated patients.2,13,14,31,34 This lower use of operating room time minimizes total costs.
Recurrence also depends on the surgeon's learning curve,34 and with more experience, the rate is lower,7,22 and so is the cost, by avoiding a second surgery.
Studies published to date demonstrate that laparoscopic repair of ventral hernias is safer and more effective than the conventional open repair approach with a lower average length of stay, and lower cost for the entire process,1,3,8,26,35 but none has been published within the Spanish public health system.
For this study, the average stay for the LAP group was significantly lower, and if we distinguish between primary hernias and incisional hernias, the difference reveals a very positive balance in favor of laparoscopic surgery. Likewise, local anesthetic+sedation is confirmed as more efficient (€3180–€3450), when it can be performed instead of general anesthesia (€7228–€7498).13
One major impact is interpreted by its effect, which is the overall savings of €101000 in patients without complications. The reduced stays also make the procedure's total cost less than that of open surgery, i.e., €2865 compared to €4125 (P<.001). Discharge facilitating factors included the absence of drains, better tolerance, and reduced postoperative pain.8,26 Therefore, a cost of €1260 was avoided each time laparoscopy was used for a case, which we consider as a major amount. This reduction of the total cost has also been confirmed in other studies,8,12 with a savings of £606 (£1514 for open surgery compared to £908 for laparoscopy). Based on all the statements above, we can consider it as an efficient technique, and that justifies its inclusion as a routine technique within the general surgery services in the scope of public health financing.
The cost could be reduced to the minimum by using fully reusable material and applying criteria for ambulatory care in selected cases, such as low-risk patients with primary hernias or incisional hernias not suspected of requiring adhesiolysis.3
To use Markov's model35 for cost evaluation, we must not only include direct perioperative costs such as those derived from surgical materials and hospital care, but also those resulting from a recurrence, which is not taken into account in this series. The inclusion of these items, in addition to the costs of conventional surgery, would raise the financial advantages of laparoscopy for this disease.26 According to this model, costs arising from the delay in returning to normal activity, both at home and at work, amount to €100–€300 of daily losses per person. Mesh repair by laparoscopic approach would represent a lower cost than mesh repair with the open approach, and the latter, lower than repair without mesh, based on the lower rate of relapse, the lower average length of stay, and the shorter duration of sick leave.2,5,36 The duration of the work sick leave period changes from 14 days with laparoscopy to 47 days with open surgery; in the US, over one million dollars have been saved between 1988 and 1991 by the incorporation of laparoscopy.19 A Swedish study confirms savings of 2400 SEK ($274) for this reason.2 The analysis in a future study of the financial benefits from the lower recurrence rate and shorter duration of sick leave would provide more financial benefits for laparoscopic repair.37–39
In conclusion, based on the results of this study, we can confirm that laparoscopic repair of ventral hernias has a higher cost for disposable surgical materials than open surgery, but it is superior, as it provides higher quality and safety, with clear advantages for the patient resulting from the reduction in morbidity, infections, abdominal wall complications and recurrence28; therefore, it results in a lower average stay, especially for incisional hernias, and a lower rate of readmission due to complications.
Finally, we consider that this may be the technique of choice for the repair of abdominal hernias by expert surgeons with the appropriate indications, since it is a treatment with a positive cost–benefit ratio that prevents an expense of €1260 per patient compared to the open technique. This should therefore be included in the portfolio of public health services with a full guarantee of efficiency.
Declaration of OriginalityWe declare that the content of this paper is original and it has not been published previously as a paper; furthermore, it has not been sent, in whole or in part, to be considered for any other publication.
Conflict of InterestAuthors declare having no conflict of interest.
Please cite this article as: Fernández Lobato R, Ruiz de Adana Belbel JC, Angulo Morales F, García Septiem J, Marín Lucas FJ, Limones Esteban M. Estudio de coste-beneficio comparando la reparación de la hernia ventral abierta y laparoscópica. Cir Esp. 2014;92:553–560.
This manuscript was presented as an abstract in the EAES Congress in Stockholm, June 2008.