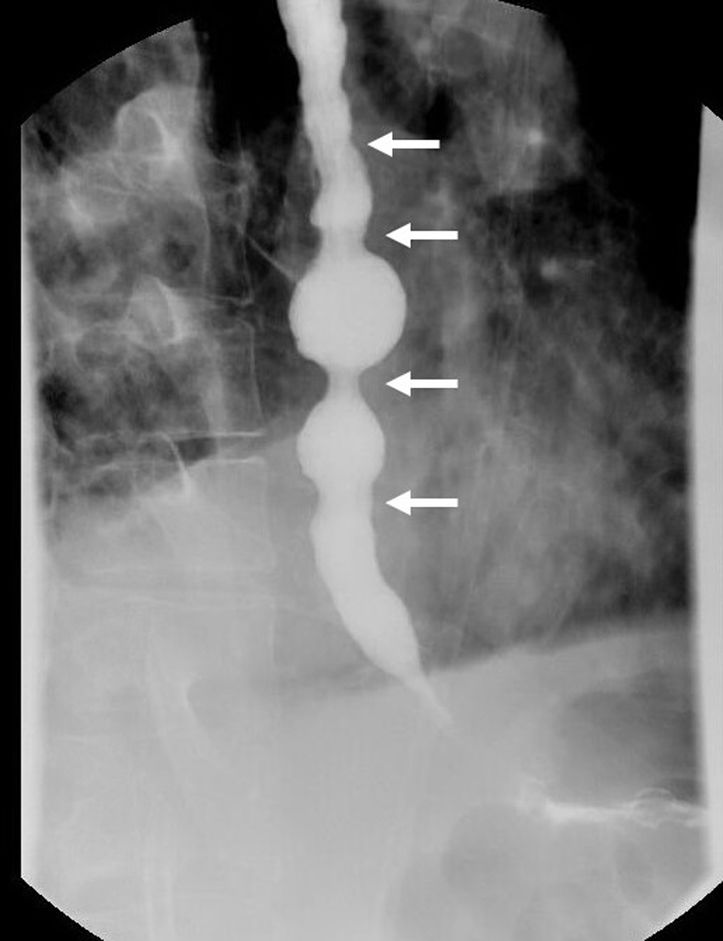
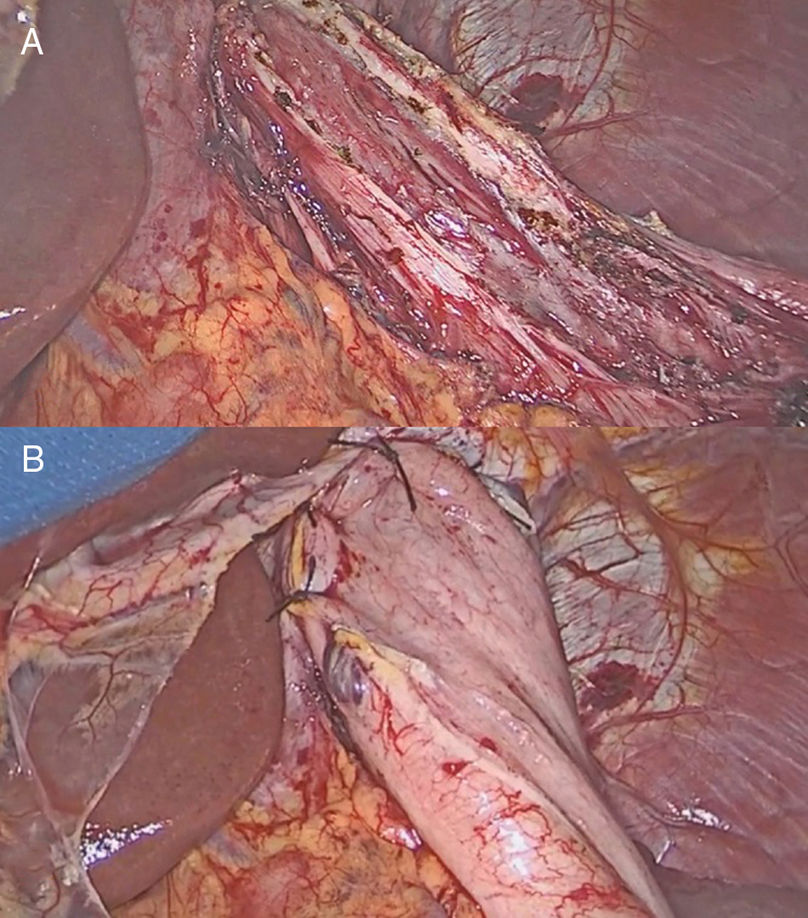
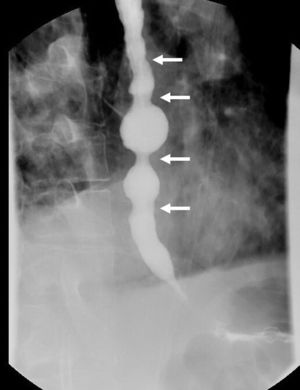
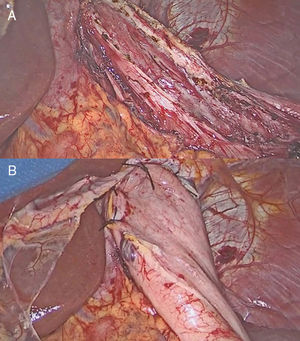
A 68-year-old man was evaluated in our clinic for intermittent dysphagia, regurgitation of liquids and solids, and chest pain. Esophagogastroduodenoscopy revealed a slightly dilated esophagus with retained food. Barium swallow showed esophageal indentations, with the characteristic “corkscrew” appearance (Fig. 1 arrows). High-resolution manometry confirmed the diagnosis of diffuse esophageal spasm (DES), with a hypertensive and non-relaxing lower esophageal sphincter. The ambulatory pH monitoring was normal. Because of the patient's progressive symptoms, which did not respond to calcium channel blocking agents and pneumatic dilatation, we performed a long laparoscopic Heller myotomy with Dor fundoplication (Fig. 2). Postoperative course was uneventful, and the patient was discharged after 24h on a soft diet. DES is a rare primary esophageal motility disorder characterized by dysphagia and intermittent chest pain. In these patients, the surgical myotomy should be extended more proximally than in patients with achalasia to obtain better relief of symptoms.
Please cite this article as: Schlottmann F, Patti MG. Espasmo esofágico difuso. Cir Esp. 2019;97:533.