Fusion of the cervical spine using an anterior approach is common in the treatment of trauma or degenerative injuries in this region.1 We present the case of an uncommon late-onset oesophageal complication after anterior cervical arthrodesis surgery.
The patient is a 43-year-old woman with diabetes and hypertension. After a car accident that had caused a cervical injury and spinal cord involvement with tetraparesis, she was treated surgically with discectomy (C5–C6) and plate arthrodesis. The patient recovered mobility and had few after effects. One year later, she began to experience progressive dysphagia to both solids and liquids, non-acid regurgitation, a feeling of fullness in the pharynx, air/fluid sounds while swallowing and a 10kg weight loss in 6 months.
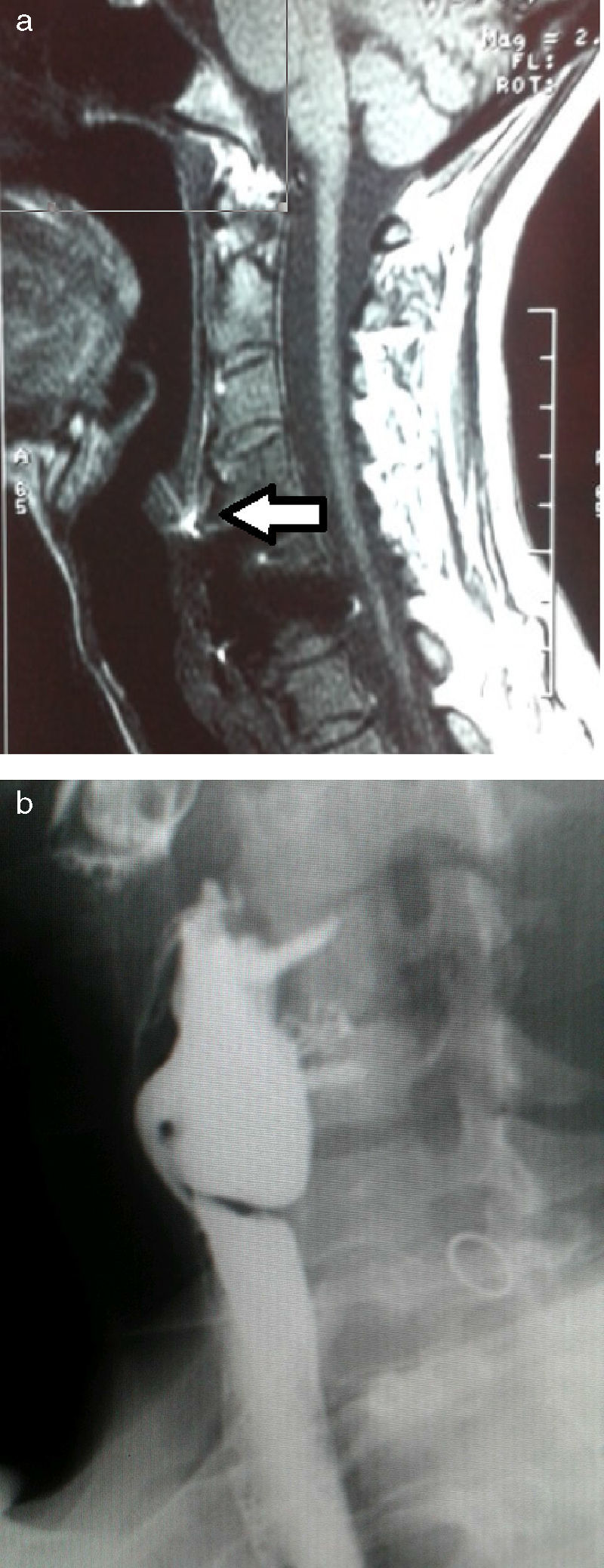
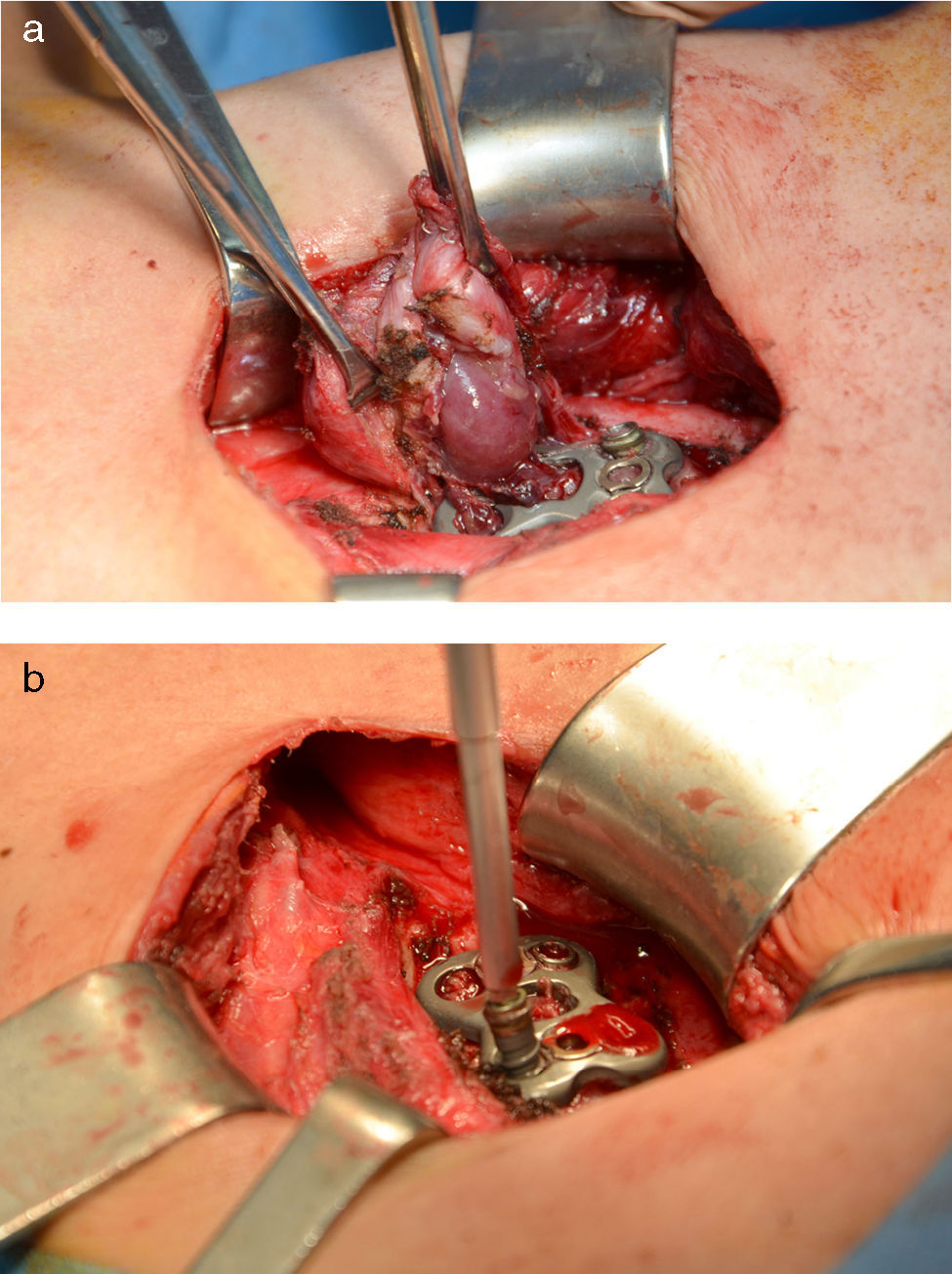
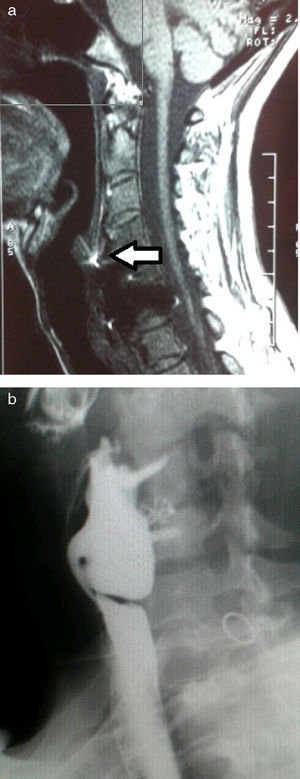
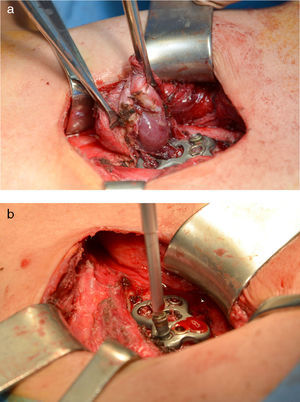
Cervical computed tomography (CT) and magnetic resonance imaging (MRI) (Fig. 1A) showed detachment and migration of the arthrodesis plate, which was in contact with the posterior oesophageal wall. Barium oesophagogram (EGD) revealed a protrusion of the metallic plate on a pharyngo-oesophageal saccular formation measuring 3–4cm (Fig. 1B). The study was completed with upper gastrointestinal (UGI) endoscopy, where the osteosynthetic piece was seen to be completely included in the posterior wall of a large pharyngo-oesophageal diverticulum. With these findings, we decided to surgically treat the patient with left cervicotomy, observing a wide-based pharyngo-oesophageal diverticulum in whose posterior wall the metallic arthrodesis plate was entirely included. This was dissected and followed by cricopharyngeal myotomy with reinforcement sutures. The diverticulum and plate were completely removed after the fixation screws had been withdrawn (Fig. 2A and B). Last of all, bone stability was analysed. The study of the surgical specimen showed a sac formation measuring 3.5cm×2.5cm with congestive mucous and histology compatible with Zenker diverticulum. The patient had an uneventful recovery and was discharged on the 10th day post-op after radiologic confirmation of proper passage of contrast and no signs of leakage.
Preoperative images: (a) sagittal view of cervical MRI showing the arthrodesis plate in close contact with the posterior oesophageal wall (arrow); (b) oesophagogram with barium contrast showing the imprint left by the metal prosthesis with screws over a cervical oesophageal sac formation.
The incidence of dysphagia after spinal surgery with the anterior cervical approach is close to 12%,2 although this percentage is probably underestimated; its aetiology is very varied. In the immediate postoperative period, oesophageal compression, which is normally mild and transitory, is usually related to oedema secondary to the intraoperative tissue manipulation, although it can be due to more severe and uncommon causes, such as oesophageal perforation. Oesophageal injuries after this type of surgery can occur in 0%–1.6% of cases. They are habitually associated with anterior instrumentation procedures in the region of C5–C7, but they can also be associated with orotracheal intubation or the insertion of a nasogastric tube. Symptoms include cervical pain, odynophagia, dysphagia, dysphonia, crackles, cervical abscess and fever, although these may progress to potentially fatal complications like mediastinitis and/or sepsis.3
Late-onset oesophageal perforations, as in our patient, are usually insidious and present with fever, dysphagia, signs of local inflammation and, occasionally, cervical abscess with cutaneous fistulisation.4 Their incidence ranges from 0.2% to 1.5%3 and, normally, they are complications derived from the migration, breakage or poor positioning of spinal fusion devices.5 Another mechanism could be chronic ischaemia due to the pressure exerted by the migrating plate.6 There are even cases of extrusion, especially of screws, through the oesophageal wall, with either regurgitation or asymptomatic passage to the gastrointestinal tract.7
EGD, CT and MRI are useful for diagnosis.6 UGI endoscopy provides direct visualisation of the pharyngo-oesophageal region and protrusion of the prosthetic material.
Treatment of this complication has still not been entirely defined. When oesophageal perforation is diagnosed during surgery, simple suture is the treatment of choice.8 However, during the postoperative period, other factors can have an influence, such as the time of diagnosis, size of the perforation or symptoms. Although there are registries of patients with small perforations (<1cm) that are contained, or inclusions without open perforation that are asymptomatic and have no cervical abscess or signs of sepsis that have been treated with drainage, antibiotics and parenteral nutrition, the disparate results seem to advise against this approach.3,4,9 Surgery, including debridement, drainage, and closure of the perforation using simple sutures or flaps,3–5,8 is the treatment of choice.9 The withdrawal of the implant is usually necessary and will depend on the time transpired since the intervention, bone fixation, displacement, exposure to contamination, symptomatology and functional repercussions.4,5,8 In our case, we opted for surgical treatment: diverticulectomy and extraction of the plate, including its wall, and bone stability was confirmed by intraoperative radioscopy.
These diverticula could be pre-existing and generated, as in the general population, by a peristaltic mechanism,1 as we believe happened in our case based on the histology. Its presence would increase the risk for oesophageal perforation during spinal surgery. But, for some authors,10 these would not be true Zenker diverticula but instead traction diverticula secondary to the fibrosis of the paraoesophageal tissues after the spinal approach and could be considered sequelae of the spinal surgery, as suggested by their atypical location.4,10 In this case, endoscopic therapy for Zenker diverticula would not be indicated, and surgery would be necessary. Furthermore, cricopharyngeal myotomy should not be used.
Oesophageal perforation after cervical spinal surgery with anterior approach is uncommon, and even more exceptional is its association with pharyngo-oesophageal diverticula. Diagnosis requires a high degree of suspicion and treatment has not been clearly established.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Acosta-Mérida MA, Medina-Velázquez R, Marchena-Gómez J, Alonso-Gómez J, Mhaildli H. Disfagia tras artrodesis cervical por migración del material protésico. Cir Esp. 2015;93:537–539.