The presence of pancreatic tissue in an aberrant position, with no communication with the normal pancreas through either vessels or ducts, is defined as ectopic pancreas.1 In a review of the literature, only 28 published cases were found of its appearance in the gall bladder.2,3 A review of the Mayo Clinic that included a total of 212 cases with ectopic pancreatic tissue found that the gall bladder was affected in only one case. We present a case that was confirmed histologically after laparoscopic cholecystectomy.
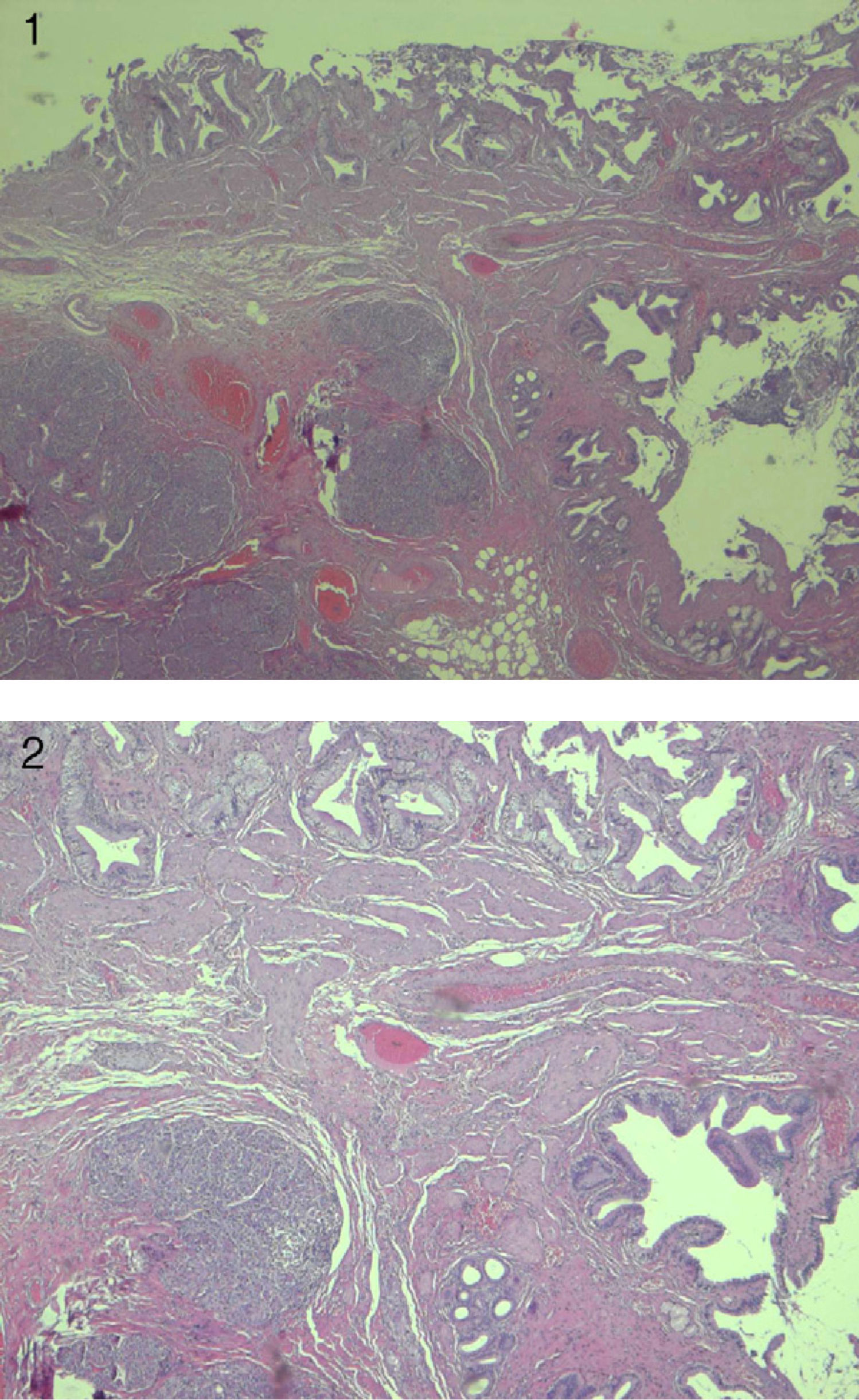
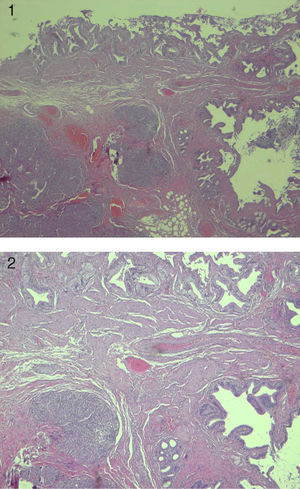
A 36-year-old male patient presented to the General Surgery outpatient clinic complaining of dyspepsia and repeated biliary colics. Complete blood tests showed a GGT 71IU/L and GPT 44IU/L, while the remaining parameters were within normal levels. Complementary tests included abdominal ultrasound, which reported a gall bladder with normal parietal thickness and a small calculus. Intra- and extra-hepatic bile ducts were not dilated and showed no calculi. The patient was diagnosed with gallstones, and laparoscopic cholecystectomy was performed. The patient was discharged 24h later without incident. The pathology report described the specimen as a cholecystectomy measuring 9cm×2cm that presented a wall thickness of 0.1cm. When opened, the mucosa was velvety green (Figs. 1 and 2). The diagnosis was gallstones and ectopic pancreas in the neck of the gallbladder.
The first case of ectopic pancreas was described by Jean Schultz in 1729, but it was not until 1859 when Klob provided histological confirmation.4 After pancreas divisum, it is considered the most common anomaly.1
Its incidence in the gastrointestinal tract is 2%. It is two to five times more common in men than in women, and 50% of cases appear between the 4th and 6th decades of life.2,5 Its location is variable, although it is predominantly found in the greater curvature and prepyloric region of the stomach (25%-35%) as well as in the second portion of the duodenum (25%-30%). Other less frequent locations are the jejunum, Meckel's diverticulum, mesentery, and there have even been cases described of its presence in the mediastinum.5,6
There are two theories that try to explain the occurrence of ectopic pancreatic tissue from an embryological standpoint. The first proposes that there would be an anomalous differentiation of pluripotent epithelial cells in the endodermal covering of the primitive digestive tube, leading to the formation of pancreatic tissue in these locations. The second theory is that some cells of the pancreatic bud can migrate and settle in a different region.2,5
Ectopic pancreatic tissue is generally intramural and in 75% of cases its location is submucosal. It usually presents as a single node that is firm and round, varying in size from a few millimeters to five centimeters. Although generally an asymptomatic anomaly, it may become clinically evident when complicated by pathological changes such as inflammation, bleeding, obstruction and malignant transformation with the appearance of nonspecific signs. The most frequent clinical symptoms include epigastric pain (77%), abdominal distension and nausea (30%), melena (24%) and vomiting (18%).5–7 The most important factors that determine the presence of symptoms are size greater than 1.5cm and the relationship with the mucosal surface.4
Ectopic pancreas commonly coexists with gallstones, polyps or pancreatitis and with anatomical anomalies of the bile duct.5,6,8
Pre-operative diagnosis may be extremely difficult due to the non-specific symptoms and the submucosal location. Endoscopic ultrasound has become the best method for evaluating submucosal lesions. Contrast CT can aid in the diagnosis and provide information that could be useful for surgical resection. Nonetheless, the definitive diagnosis is histological. We must also keep in mind that in the case of the gallbladder none of these complementary tests are useful.5,6,8
Malignant degeneration is exceptional, and most commonly occurs in the stomach.9 The treatment of choice is complete resection.1,5,6 In cases with stomach affectation, endoscopic ablation has been performed successfully.10 In our case, we consider that cholecystectomy is the correct treatment. The recurrence of aberrant pancreatic tissue has not been described in the literature.
Please cite this article as: González Callejas C, et al. Páncreas ectópico en la vesícula biliar. Cir Esp. 2013;91:130–1.