Popliteal aneurysms (PA) are the most common peripheral arterial aneurysms. They can be unilateral or bilateral and are usually associated with abdominal aortic aneurysm (40%–50%). They are usually asymptomatic and are diagnosed as a chance finding. When symptoms are present, the most common are intermittent claudication and acute ischaemia due to embolisation distal to the aneurysm or complete thrombosis of the aneurysm. Rupture of the aneurysm and associated compressive symptoms are less common.1–3 The risk of thromboembolic complications in asymptomatic PA is 39%. On the other hand, the risk of limb amputation despite urgent revascularisation is more than 40%.4
Asymptomatic PAs will be treated as long as they are larger than 2 cm and all symptomatic PAs will be treated. The classical treatment of PA is exclusion of the aneurysm followed by revascularisation of the limb by bypass, autogenous vein or prosthesis.5,6 On the other hand, endovascular treatment of PAs has been little recommended because of the anatomical area involved (knee flexure), as it increases the risk of kinking and rupture, thrombosis or graft migration. However, with the growth and development of the endovascular technique, new grafts and optimisation of antiplatelet therapy, increasingly better results are being achieved.5,7
Despite this, there is yet to be any consensus over which of the 2 techniques is appropriate for the treatment of PA, although open surgery still presents better outcomes regarding long-term patency.8
Eighty-nine-year-old male, ASA IV, with right transfemoral amputation in 2014 due to acute irreversible arterial thrombosis by PA, autonomous, who walks with prosthesis. He came to the emergency department with cyanosis and pain in the first 3 toes of the left foot. Examination revealed an expansive popliteal pulse and absence of distal pulses. Continuous Doppler showed distal flow in the posterior tibial focus.
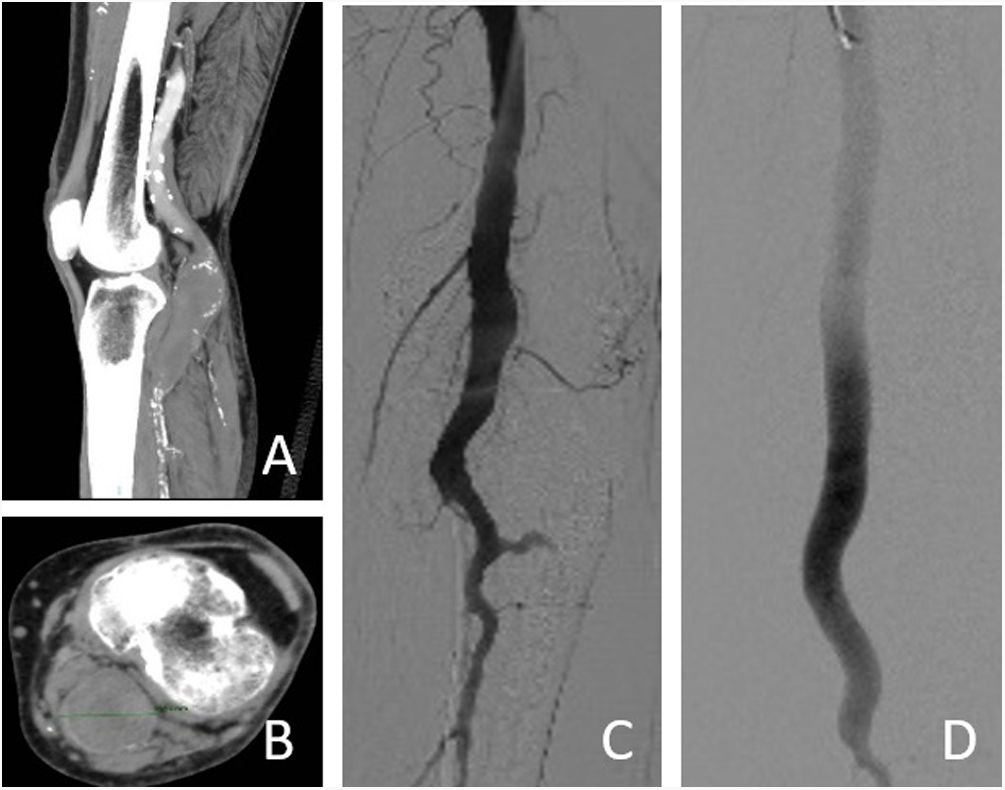
CT angiography revealed a PA of 3.6 cm in diameter (Fig. 1). Given the patient's stability, preferential surgical intervention was decided. After dissection and control of the superficial femoral artery, an antegrade arterial puncture and arteriography were performed, which revealed PA and tibioperoneal trunk with occlusion of the anterior tibial artery and peroneal artery as the only permeable sural vessel. Three coated stents are implanted (Gore® Viabahn®, one 11 mm × 50 cm graft and two 13 mm × 10 cm grafts, with 2 cm overlap between grafts) with proximal anchoring in first popliteal portion and distal anchoring in tibioperoneal trunk, securing healthy artery for proximal and distal anchoring due to the extension of the aneurysm. The patient was discharged 3 days after the intervention after a satisfactory evolution and with double antiplatelet therapy. After 2 months and the delimitation of the lesions, amputation of the first, second and third fingers was performed under local anaesthesia due to pain refractory to analgesic treatment.
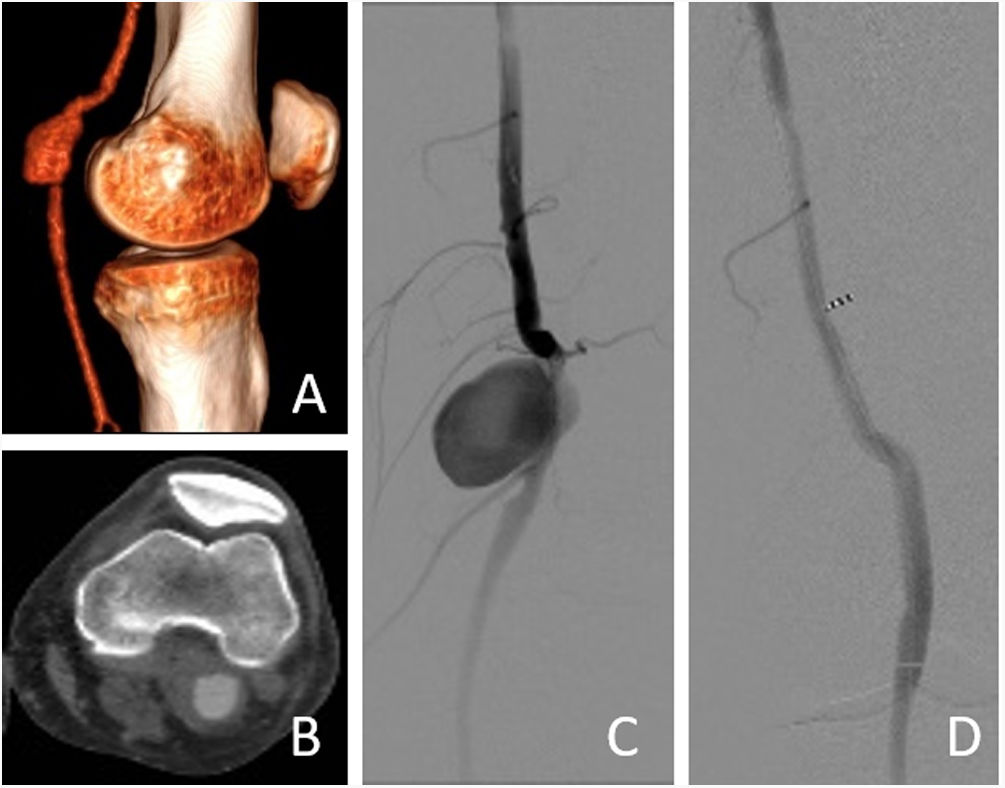
Sixty-five-year-old male, ASA IV, obese and with a history of deep vein thrombosis in the right lower limb and left saphenous vein not valid for bypass, with a chance diagnosis of left PA by Doppler ultrasound. The angio-CT scan showed a PA with a maximum diameter of 2.3 cm with permeability of the third sural vessels (Fig. 2). Elective surgical intervention was indicated. After dissection and control of the superficial femoral artery, an antegrade arterial puncture and arteriography were performed, which revealed a saccular aneurysm in the first portion of the popliteal artery with permeability of the 3 distal vessels. A coated stent (Gore® Viabahn® 9 mm × 10 cm) was implanted. He had a good evolution in the immediate postoperative period and was discharged 2 days after the operation, with double antiplatelet treatment for 3 months.
Although the gold standard continues to be surgical treatment (aneurysm exclusion and bypass), with the improvement of available grafts, endovascular treatment of PA is becoming a safe and valid technique9 that shows advantages over open surgery in older patients with many comorbidities and in patients with saphenous vein of inadequate quality, as in the cases we have presented.
The advantages of endovascular treatment are less invasive compared with conventional surgery. There is no need for general anaesthesia, there is less bleeding of the limb and a shorter procedure and hospitalisation time. However, its use is limited to patients with adequate anatomy (at least 2 cm of healthy artery proximal and distal to the aneurysm for anchoring the prosthesis).10 For these reasons it was the technique of choice in our cases: the first, an elderly patient with comorbidities and a history of acute thrombosis of the contralateral PA with a poor outcome, who presented thromboembolism distal to the PA with a high risk of limb loss; and the second, an obese patient with a poor quality vein for bypass. Both patients had a favourable anatomy for endovascular treatment.
With the improvement of available grafts, the implementation of temporary dual antiplatelet therapy and improved technique development, endovascular treatment of PA is becoming a safe and valid technique in older patients at high surgical risk.
Please cite this article as: Quintero-Pérez C, Manresa-Manresa F, García-de Vargas A, Mengíbar-Fuentes L, Bataller-de Juan E. Tratamiento endovascular del aneurisma poplíteo en pacientes de alto riesgo quirúrgico. Cir Esp. 2022;100:448–450.