Priapism is an uncommon pathological condition causing prolonged erection of the penis that is generated or persists beyond sexual stimulation.1 Recent studies have determined the incidence of priapism to be between 1.5% and 2.9% per 100 000 inhabitants/year.1 In 1983, Hauri et al.2 created a physiopathological classification of two different types: veno-occlusive or low-flow priapism, and arterial or high-flow priapism (HFP). HFP is generally caused by a trauma injury to a cavernous artery, that gives rise to an arteriovenous fistula or an associated pseudoaneurysm,3 causing a prolonged, non-ischemic and non-painful erection.
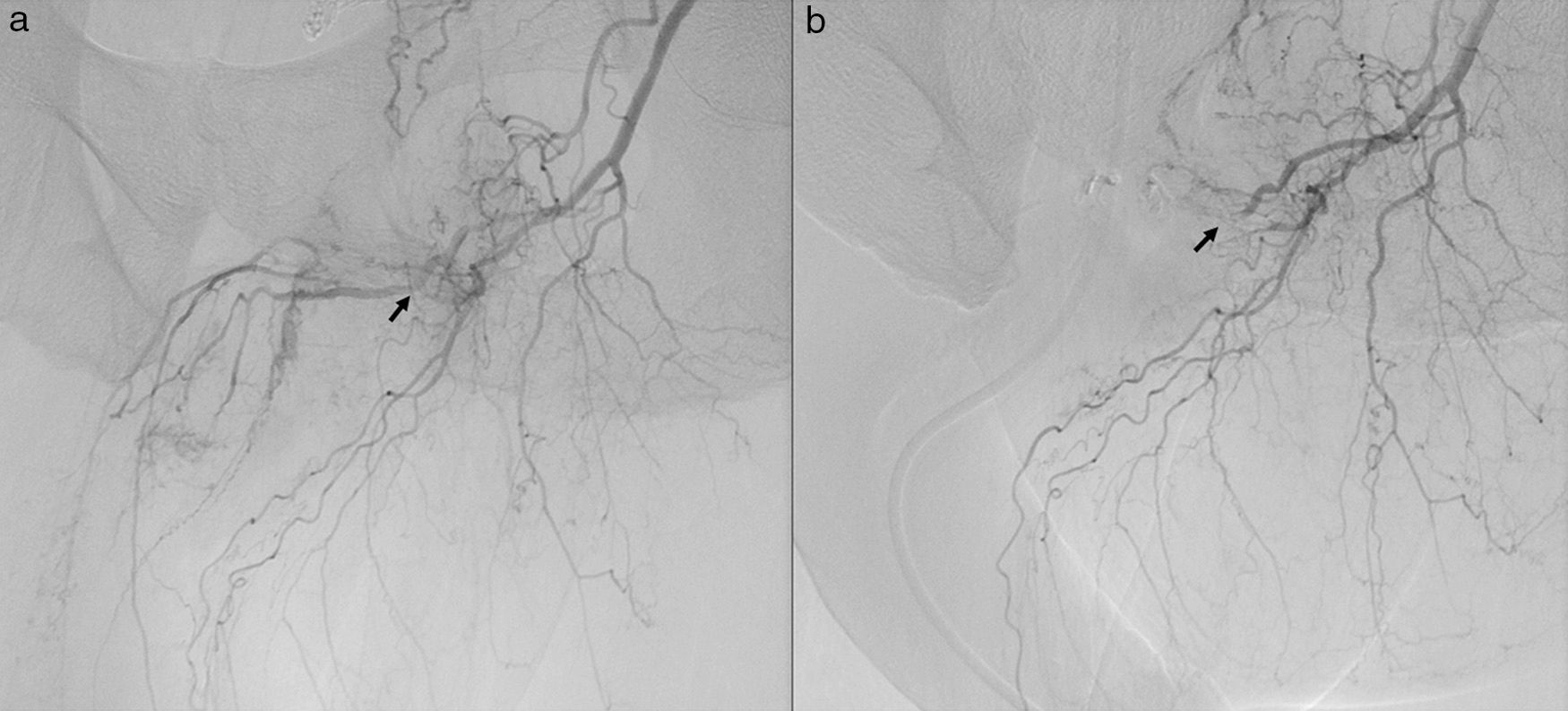
We present the case of a 50-year-old patient who underwent elective surgery for rectal adenocarcinoma, stage iiib (T3dN1M0). Colonoscopy revealed a stenosing mass located 8cm from the anal margin. Computed tomography scan of the thorax–abdomen–pelvis and magnetic resonance imaging detected important wall thickening of the rectum 8cm from the anal margin. The patient received neoadjuvant treatment with radiochemotherapy (in total 50.4Gy). As the tumour was bulky, anterior resection of the rectum was performed using laparotomy access. Twenty-four hours after the procedure, the patient presented a complete, maintained and non-painful erection. Arteriography showed an arteriovenous fistula (AVF) between the right internal pudendal artery and the corpora cavernosa, which caused rapid, constant filling (Fig. 1). This was treated with superselective arterial embolisation with sponges (Spongostan®) until the symptoms improved. Several sessions were necessary until the AVF was completely obliterated (Fig. 1b). Afterwards, the patient remained impotent until 4 months after surgery, after which time his condition progressively improved, and he is now currently asymptomatic.
HFP was described for the first time in 1960 by Burt et al.4 as a pathological increase in the arterial flow to the corpora cavernosa. This has been commonly described in small series of cases as secondary to blunt perineal trauma affecting the artery of the penis. It is less frequently due to reactions to medications, valve pathologies, metastatic disease of the penis, acute medullary injury and intracavernosal suction or injections.5 Thus, its presentation is exceptional after surgery in the pelvic-perineal region, and there are currently only 2 cases of HFP with no previous history of trauma: after orthopaedic hip surgery, and after endoscopic urethrotomy. This case is currently the first description of HFP after abdominal surgery.5–7
Unlike other types of priapism, HFP does not have a risk of ischaemia, so its treatment is not considered urgent. Treatment of HFP has been based on conservative management: wait for the spontaneous closure of the fistula, or apply ice and compression to the perineal region, the latter of which is widely used in children. Surgical treatment, which is rarely utilised, involves selective ligation of the fistula. This technique is difficult and carries risks, such as erectile dysfunction due to the accidental ligation of the cavernous artery. The current treatment of choice is selective arterial embolisation with absorbable material using autologous coagulation, gel foams or sponges. These guarantee a transitory interruption of the arterial flow through the lacerated vessels, while allowing for the reestablishment of the arterial flow in the cavernous artery and the preservation of erectile function after the dissolution of the embolising material.8,9 Occasionally, non-resorbable material can be used, such as metallic spirals or acrylic adhesive, which cause the permanent blockage of the artery and can have adverse effects on spontaneous sexual function. Selective arterial embolisation has a success rate of up to 89%, with a recurrence rate after embolisation of 7%–27%.5 Sexual function can be affected after embolisation, although complete restoration of sexual function occurs over time in approximately 80% of these patients. Other possible associated complications include gangrene of the penis, persistent impotence, gluteal ischaemia, purulent cavernositis and perineal abscess.5
In the case of our patient, we see a possible correlation between the appearance of this uncommon condition and excessive mechanical tissue retraction of the abdominal wall utilised in this intervention, which is a method that is commonly used during open surgery. Thus, this case shows evidence that these abdominal wall retraction methods are not innocuous and should be used prudently. Surgery of the pelvic area is widely known as having, in deep fields, a certain difficulty for visualisation, which is also related with the small operative field involved. Especially in lower sections of the rectum, this phenomenon occasionally requires excessive traction of the surrounding tissues, which can consequently injure other structures.
In short, the case we have described demonstrates that the use of tissue retraction methods during open surgery in the pelvic area is not a manoeuvre that is free of risks and can lead to the development of exceptional complications, as seen in our patient.
Conflict of InterestsThere are no relationships, conditions or circumstances that could lead to a potential conflict of interests.
Please cite this article as: Mon Martín F, Guil Ortiz B, Delgado Plasencia L, Medina Arana V, Bravo Gutiérrez AF. Priapismo de alto flujo: una complicación excepcional de la cirugía del cáncer de recto. Cir Esp. 2016;94:116–118.