The iliac wing is frequently used as a donor area for autogenous bone tissue for grafts in orthopedic surgery due to the quality and quantity of bone available and its easy accessibility. Herniation of the intra-abdominal viscera through the created bone defect is a potentially serious complication.
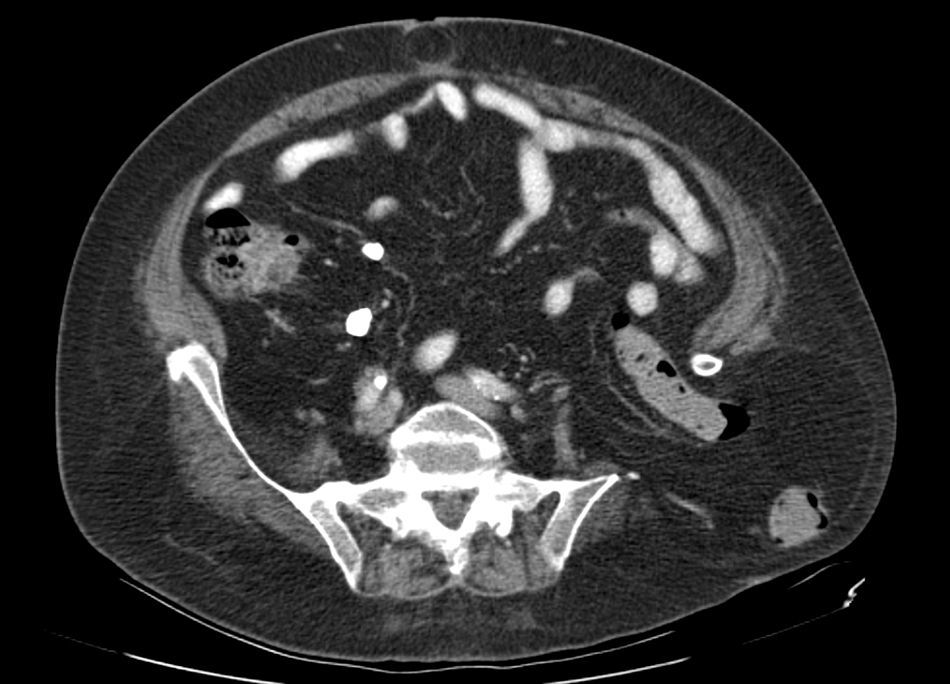
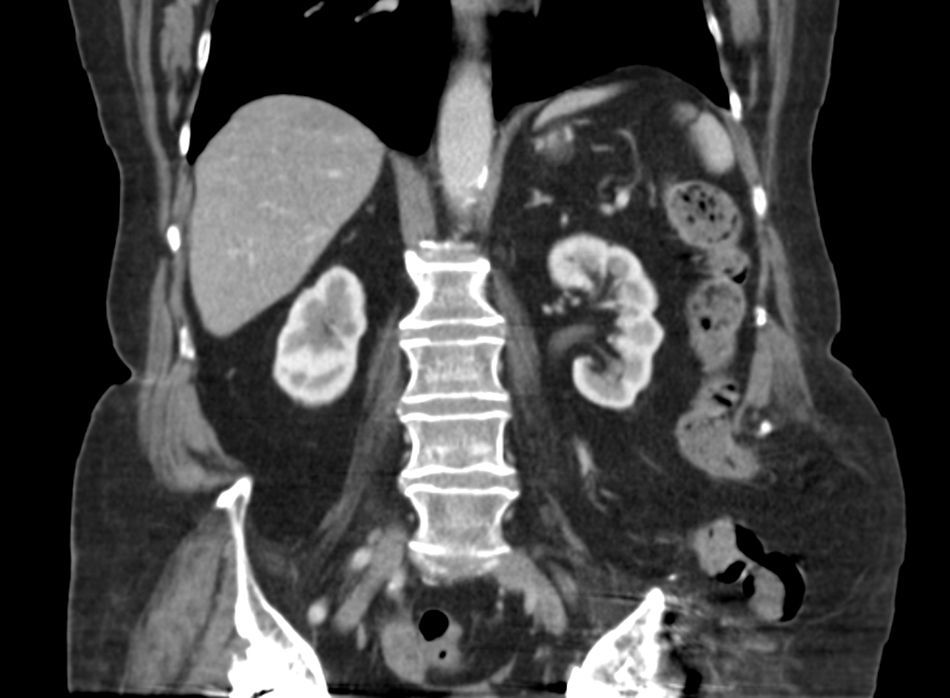
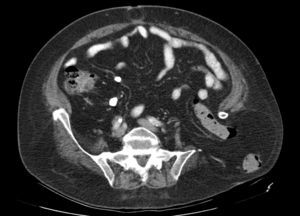
We present the case of a 76-year-old patient with metabolic syndrome (body mass index 36), who had been treated for bilateral coxarthrosis secondary to congenital dislocation of the left hip using a Müller-type bilateral prostheses at the age of 36. The patient required replacement of the left prosthetic socket due to de-cementation and replacement of the left prosthesis with autogenous bone graft of the iliac wing in the acetabular fundus at the ages of 48 and 53, respectively. The patient reported episodes of colic abdominal pain for several months, and physical examination revealed an irreducible swollen mass in the left gluteal region. Abdominal computed tomography showed a transiliac hernia and an umbilical hernia (Figs. 1 and 2). The surgical intervention consisted of: subumbilical midline laparotomy; incision of the left parietal peritoneum to mobilize and introduce into the abdominal cavity the segments of the descending and sigmoid colon that were herniated and incarcerated; access to the retroperitoneal space and implantation of a 20×20cm polypropylene mesh, extended in retroperitoneal position to widely cover the hernia orifice and the adjacent musculoskeletal structures, without being in contact with the visceral peritoneum; the mesh was affixed with several cardinal non-absorbable stitches and maintained in its correct position by the intra-abdominal pressure itself. The laparotomy was closed with a double continuous suture of slowly absorbable material and repair of the umbilical hernia. There were no postoperative complications. After one year of follow-up, physical examination has shown no hernia recurrence.
Obtaining autogenous bone graft from the wing of the ilium has a morbidity rate between 12% and 20%, which is even higher if the donor area is the anterior part of the iliac crest and not the posterior (23% vs 2%, respectively). Among the various postoperative complications,1 the most important is “iliac hernia”, which is a term used in the literature to describe this condition, although it is occasionally classified as a lumbar hernia. This condition, described by Oldfield in 1945, is a poorly documented entity that is probably underestimated because fewer than 40 cases have been reported since its first publication2,3; however, its incidence is estimated from 5% to 9%.1,4
Its etiopathogenesis is a consequence of the surgical defect in the coxal bone, almost always related with having obtained a bone graft or, less frequently, after fractures,5 debridement due to osteomyelitis, and on rare occasion due to a congenital bone defect.
Its appearance has been reported between the first days following the operation and up to 15 years after the bone defect.6 This complication seems to be more frequent in women. The small intestine is the most commonly herniated organ, and there are reports of strangulation and torsion. Other organs, such as the liver, have also been reported.7
The diagnosis is suspected when a mass is confirmed in the gluteal scar, which may be difficult to assess in cases of obesity and more posterior locations. Differential diagnosis should include hematoma2 or abscess and other less probable ailments, such as intra-abdominal neoplasms, renal cancer, muscle hernia, soft-tissue tumors and lumbosacral panniculitis. It is confirmed with abdominal computed tomography, which is the complementary test of choice as it demonstrates the herniated anatomy and contents.
Surgical treatment, which can be difficult, should be done with some urgency to avoid potential complications (risk of incarceration and strangulation are 25% and 10%, respectively8), although in one selected case that had emerged after bone resection due to chondrosarcoma, the approach was “wait and see”.9 Among the surgical options, the following have been proposed3,8:
- •
Repair with the adjacent soft tissue, mobilizing the iliac muscle, lumbar fascias and gluteus maximus (Dowd and Koontz techniques) or abdominal fascias, which are reinserted over the remaining bone.
- •
Bosworth technique: creation of an iliac “neocrest” by transposition of the anterior area of the iliac crest to the posterior, where the abdominal fascia is reimplanted.
- •
Closure of the defect with bone allografts or grafts with synthetic mesh, done laparoscopically in favorable situations.10
In the case described, surgical difficulty was expected due to the obesity of the patient and the large length of colon stuck through a ring of mainly bone. These factors led us to select a laparotomic approach, although laparoscopy can be indicated in less complex circumstances due to its lower early and late morbidity. Placement of a mesh directly over the hernia orifice by an extraperitoneal lateral approach could have a higher percentage of recurrence. To avoid this, we considered it best to use a large mesh of polypropylene or polyester (polytetrafluoroethylene or mixed if there is contact with hollow viscera) that, from the inside of the abdominal cavity and held by the intra-abdominal pressure, covered the hernia orifice.
Despite the curative intent of the various repair techniques mentioned above, the recurrence rate is high.
To prevent transiliac hernia, it is advisable to obtain a bicortical bone graft instead of tricortical, and large grafts should be avoided.7 Some authors have assessed the possibility of placing a prophylactic mesh in the bone defect.1
Please cite this article as: Martínez Rodenas F, Torres Soberano G, Hernández Borlan R, Moreno Solórzano JE, Llopart López JR. «Hernia transilíaca». Una original modalidad de eventración probablemente no tan infrecuente. Cir Esp. 2017;95:618–620.