Surgical training based on simulation seeks the acquisition of skills in novice participants and ongoing skill development in experts. The aim of this study is to assess the evolution of students in an intensive laparoscopic anastomosis course and to analyze their results depending on their level and previous experience.
MethodsThe students of all the anastomosis courses conducted during 30 months in the Valdecilla virtual hospital (Santander) were analyzed. Manual side-to-side intestinal anastomoses with porcine ‘ex vivo’ viscera were performed in a laparoscopic endotrainer.
The technical and quality differences between the first and the last anastomoses were analyzed and the progression between residents and specialists was compared.
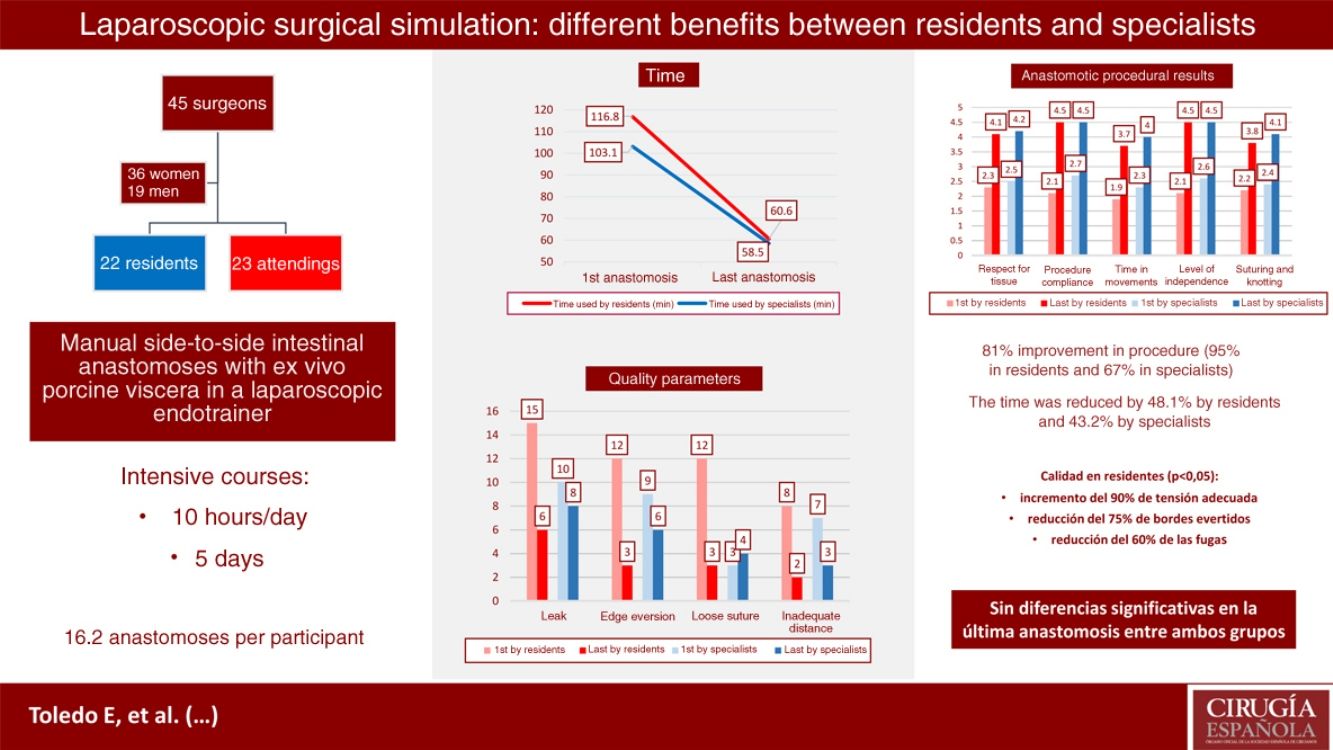
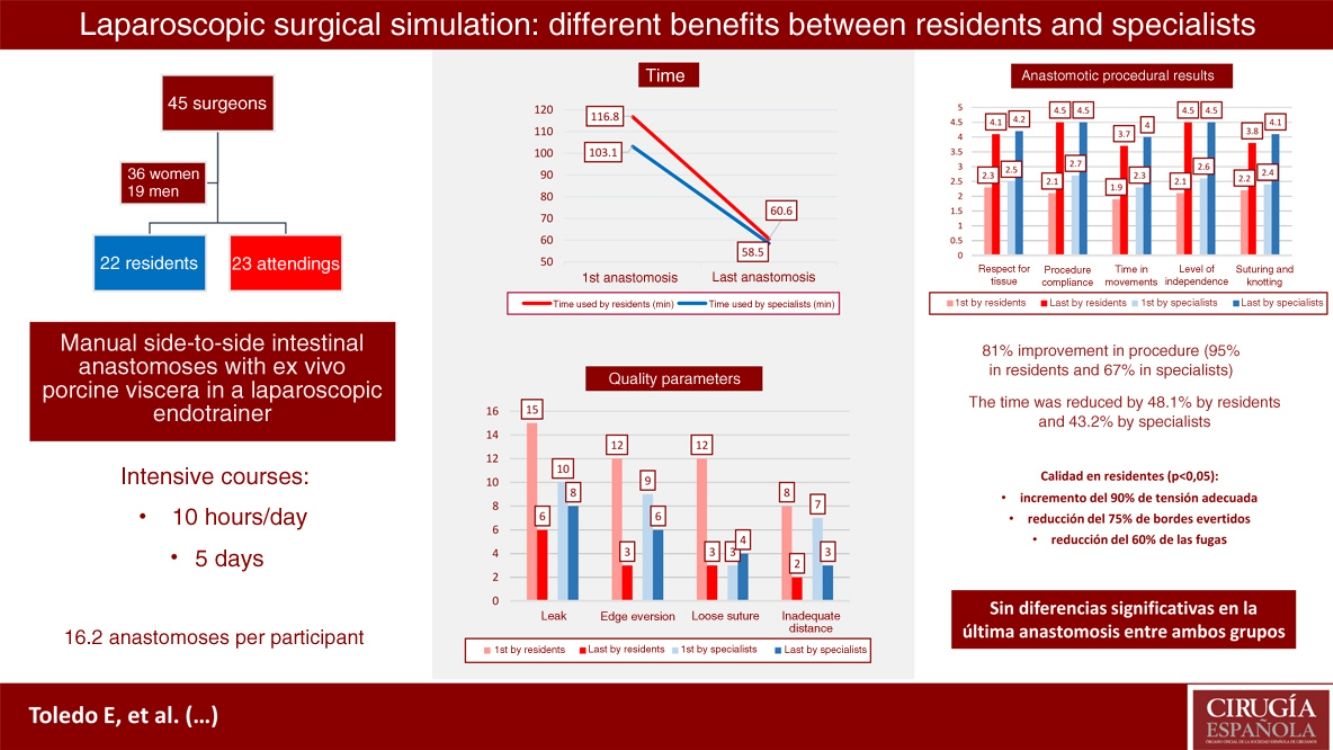
ResultsWe analyzed 45 participants, 22 of them residents and 23 specialists. A statistically significant improvement of 80.5% was observed in all procedural parameters (94.8% residents vs. 67.3% specialists). The time was reduced by 48.1% in the residents and 43.2% in the specialists (P<.001).
In terms of quality, significant improvements were obtained in the group of residents: an increase of 90% in adequate tension, and a reduction of 75% of everted edges and 60% of leaks. In addition, they obtained results comparable to the specialists (27.3% leak in the last anastomosis vs. 34.8% by the specialists, P=.59), which presented improvement without statistical significance.
ConclusionsThe group of residents presented a major and significant improvement in procedural skills and in the quality of the technique, reaching the level of the specialists after completion of the course.
El entrenamiento quirúrgico basado en simulación busca la adquisición de habilidades en los participantes noveles y la capacitación en los expertos. El objetivo de este estudio es valorar la evolución de los alumnos en un curso intensivo de anastomosis laparoscópica y el análisis de sus resultados dependiendo de su nivel y experiencia previa.
MétodosSe analizaron los alumnos de todos los cursos de anastomosis realizados durante 30 meses en el Hospital virtual Valdecilla (Santander). Se realizaron anastomosis intestinales latero-laterales manuales con vísceras «ex vivo» porcinas en un endotrainer laparoscópico.
Se analizaron las diferencias técnicas y de calidad entre la primera y la última anastomosis y se comparó la progresión entre residentes y los facultativos especialistas.
ResultadosSe analizaron 45 participantes, 22 de ellos residentes y 23 especialistas. Se observó una mejoría estadísticamente significativa del 80,5% en todos los parámetros procedimentales (94,8% residentes vs. 67,3% especialistas). El tiempo se redujo un 48,1% en los residentes y un 43,2% en los especialistas (p<0,001).
En cuanto a calidad, se obtuvieron mejorías significativas en el grupo de residentes: incremento del 90% de tensión adecuada, reducción del 75% de bordes evertidos y 60% de las fugas. Además, obtuvieron resultados comparables a los especialistas (27,3% fuga en última anastomosis vs. 34,8% especialistas, p=0,59), los cuales presentaron mejoría sin significación estadística.
ConclusionesEl grupo de residentes presenta una mejora mayor y significativa en habilidades procedimentales y en calidad de la técnica, alcanzando el nivel de los especialistas tras completar el curso.
Surgical training has evolved from the master-apprentice relationship of the 18th century (based on the observation and imitation of surgical techniques) to today's complex training methods using computer simulations and virtual reality. However, a milestone in surgical development was marked by William Stewart Halsted and Franklin P. Mall in Baltimore in 1886, in Baltimore, who began training intestinal sutures in experimental animals.1 Previously in 1847, the American Medical Association (AMA) was created in order to increase ethical standards in the field of medicine. Likewise, in the field of training, the first association was created in 1876 to reform medical education: the Association of American Medical Colleges (AAMC). Since then, ethics and medical training have evolved, making high-quality technical training necessary prior to patient treatment.2
Presently, after the social and technological evolution of recent generations, education is becoming more experiential in content and methodology3 to adapt to this new profile, as current learning methods and motivations differ from those of previous generations.4 Given this situation, simulation stands out as an important tool for acquiring surgical skills, while also responding to the growing demand of surgical skills training.5
The use of simulation as a surgical training tool has proven to be more effective in the integration of complex clinical-surgical knowledge and skills compared to traditional methods.6–9 It has been validated in both behavioral and decision-making techniques.10,11
The objective of this study is to assess the evolution of students participating in an intensive practical course of advanced laparoscopic techniques (intestinal anastomosis) based on simulation. Afterwards, the results will be analyzed according to the training level and the previous clinical experience of the participants to determine the influence of these parameters on skill acquisition and the need for evolution or optimization of training systems.
MethodsAn observational study was conducted to analyze the participants taking anastomosis courses held at the Valdecilla virtual hospital (Santander, Cantabria) between March 2015 and November 2017. All General Surgery and Gastroenterology participants were included in the study if they had completed the course and had taken it for the first time.
The format of the courses was intensive, with long training sessions (10h/day) concentrated into a short period of time (5 days). They were held quarterly, with 4–8 participants per course and one instructor for a maximum of 3 students. During the sessions, manual side-to-side intestinal anastomoses were created with porcine ex vivo viscera in a laparoscopic endotrainer. This device is basically a closed box made of tinted methacrylate with silicone inlets along the upper side, through which laparoscopic trocars are inserted along with a fiber optic cable supported by a metallic arm (Fig. 1). The anastomosis technique used includes interrupted supporting sutures and continuous double suture with Connell sutures at the vertices (Fig. 2).
The teaching methodology involved the following steps: provide participants with literature and videos demonstrating the surgical technique; one previous meeting to introduce participants to the simulation laboratory; discussion of articles and overview of the procedure; critical steps of the technique are then demonstrated by the instructor, including the handling of laparoscopic instruments, constant feedback from the instructor, time and quality control, rigorous reflection at the end of the session (debriefing), and deliberate and repetitive practice.
The variables analyzed were the quality parameters for standardized anastomoses based on a Delphi method12: correct distance between stitches (2.5–3.5mm), suture tension (<1cm of excess thread after cutting and traction), eversion of edges and presence of leakage (air leak testing by manometer).
The technical variables studied were: respect for tissue, suture and knotting technique, time and movement, technique compliance and level of independence. The development of the technique was analyzed with the Objective Structured Assessments of Technical Skills (OSATS), which is a validated tool for basic surgical skills assessment.13 Authors like Reznick have designed an OSATS scale to evaluate intestinal anastomoses in live animals,14 including a task checklist that has been used in our experience, giving a score from 1 to 5.
All the anastomoses performed were analyzed and scored by the same group of instructors, and the results obtained for the first and last anastomoses were compared for each participant.
The results were compared between residents-in-training and specialists. Likewise, for our analysis, a subgroup was created of expert participants who had advanced clinical experience (≥50 anastomosis).
Statistical AnalysisThe statistical analysis was carried out with the 2016 IBM SPSS Statistics for Windows, version 24.0 (Armonk, NY: IBM Corp).
The Kolmogorov–Smirnov test confirmed normal distribution for the time variable alone, for which a bivariate analysis was done with the Student's t test for paired data to compare anastomosis results at the beginning and end of the course. For the rest of the quantitative variables, the Mann–Whitney test was performed, using the Wilcoxon test for related samples. The categorical variables were analyzed by the Chi-squared and McNemar tests in related samples. In situations in which the expected frequencies were less than 5, Fisher's exact test was used.
A P value <.05 was considered statistically significant.
ResultsForty-five participants (36 women and 19 men) were analyzed; 22 of the participants were residents and 23 specialists. Their average clinical experience was 70.8 anastomoses performed in open surgery (a mean of 15.6 for residents and 136.5 for specialists) and 1.4 in laparoscopic procedures (0.5 residents vs. 3.1 specialists). Thirteen participants had performed ≥50 anastomoses in their daily practice (both open and laparoscopic surgery), all of whom were considered specialists. An average of 16.2 anastomoses per participant were completed during the course.
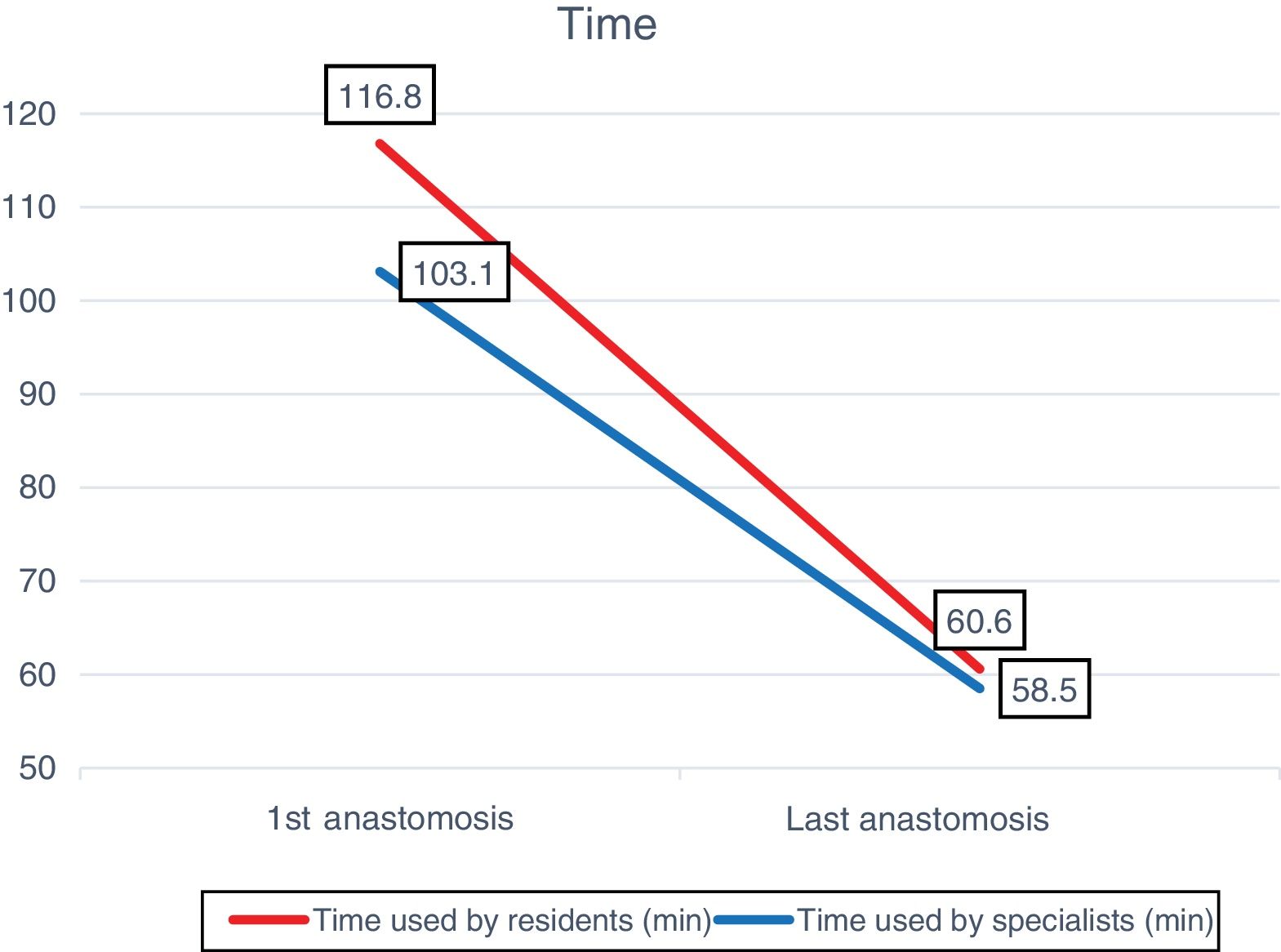
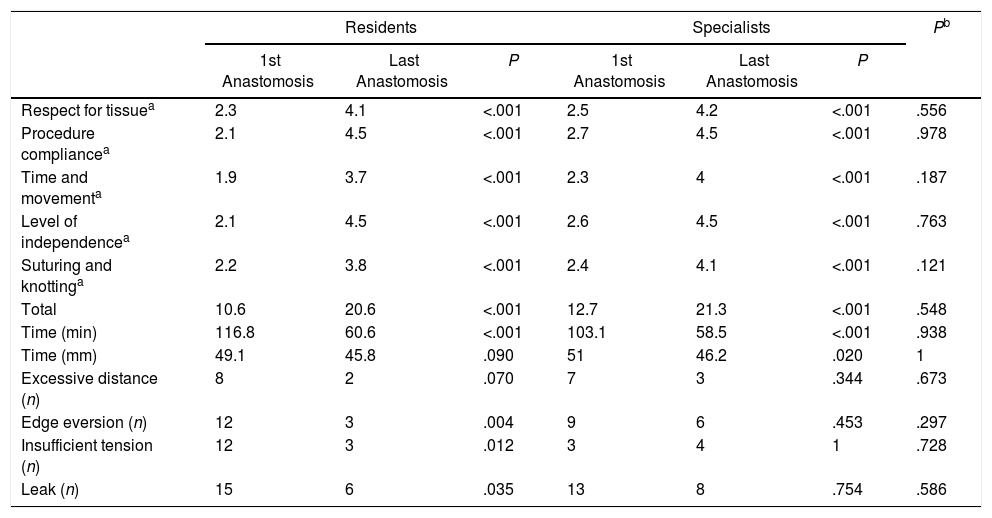
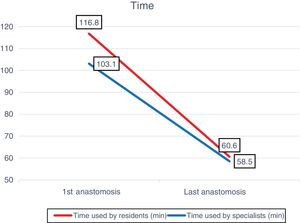
The technique time was reduced from 116.8 to 60.6min (48.1%) for the residents and from 103.1 to 58.5min for the specialists (43.2%), with a P<.001 in both groups. The lengths of the anastomoses decreased from 49mm (first) to 46mm (last) for residents (P=.090), and 51mm (first) to 46mm (last) for specialists (P=.020) (Fig. 3).
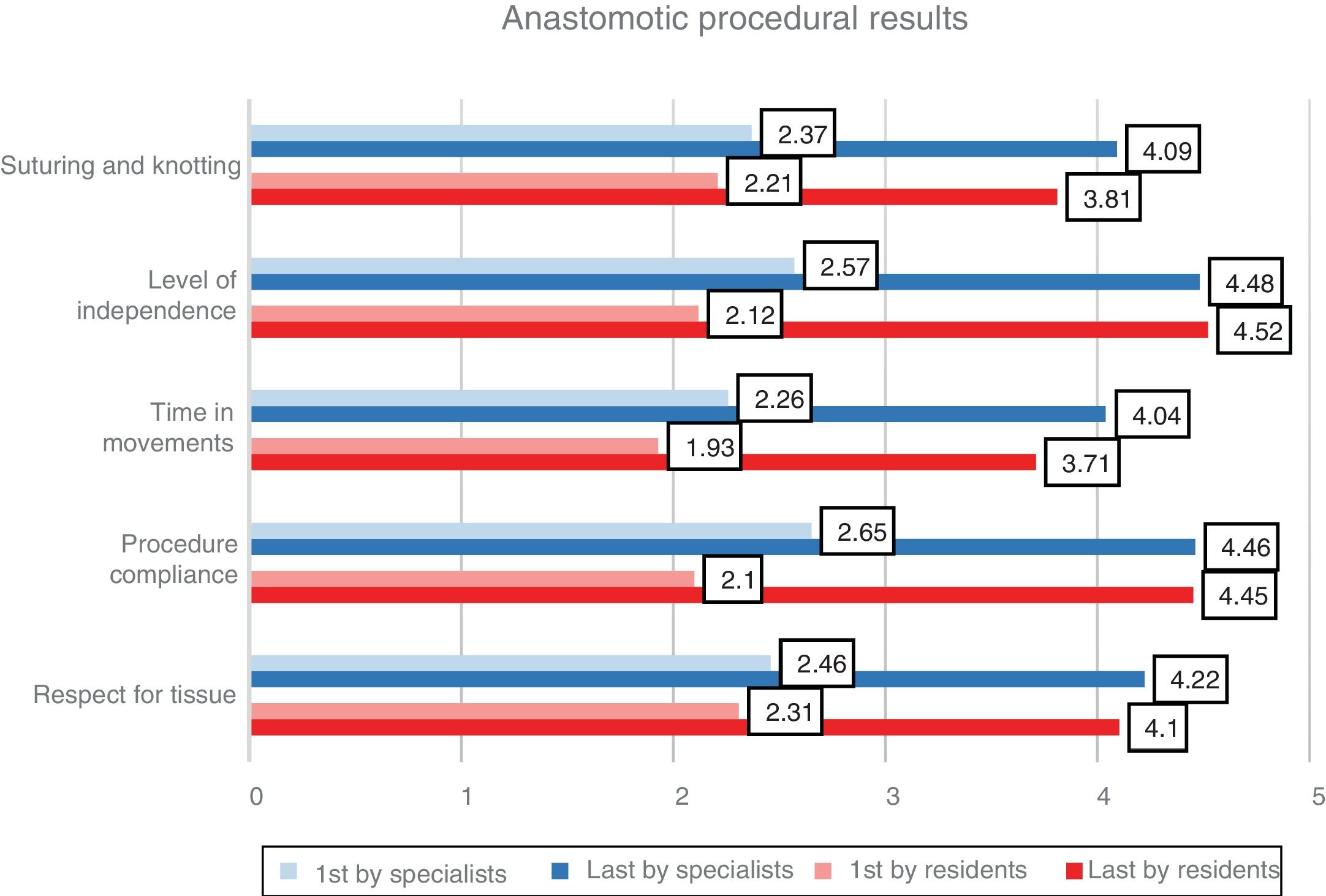
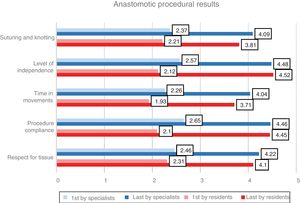
The results are shown in Table 1, with an overall improvement in procedural parameters of 80.5% (67.3% in specialists and 94.8% in residents), with a P<.001. In the last anastomoses, there were no significant differences between residents and specialists in terms of respect for tissue (4.1 and 4.2, respectively), procedure development (4.5 vs. 4.5), time in movements (3.7 vs. 4.0), level of independence (4.5 vs. 4.5) and suture and knotting (3.8 vs. 4.1) (Fig. 4).
Procedural and Quality Results in the First and Last Anastomoses Created.
| Residents | Specialists | Pb | |||||
|---|---|---|---|---|---|---|---|
| 1st Anastomosis | Last Anastomosis | P | 1st Anastomosis | Last Anastomosis | P | ||
| Respect for tissuea | 2.3 | 4.1 | <.001 | 2.5 | 4.2 | <.001 | .556 |
| Procedure compliancea | 2.1 | 4.5 | <.001 | 2.7 | 4.5 | <.001 | .978 |
| Time and movementa | 1.9 | 3.7 | <.001 | 2.3 | 4 | <.001 | .187 |
| Level of independencea | 2.1 | 4.5 | <.001 | 2.6 | 4.5 | <.001 | .763 |
| Suturing and knottinga | 2.2 | 3.8 | <.001 | 2.4 | 4.1 | <.001 | .121 |
| Total | 10.6 | 20.6 | <.001 | 12.7 | 21.3 | <.001 | .548 |
| Time (min) | 116.8 | 60.6 | <.001 | 103.1 | 58.5 | <.001 | .938 |
| Time (mm) | 49.1 | 45.8 | .090 | 51 | 46.2 | .020 | 1 |
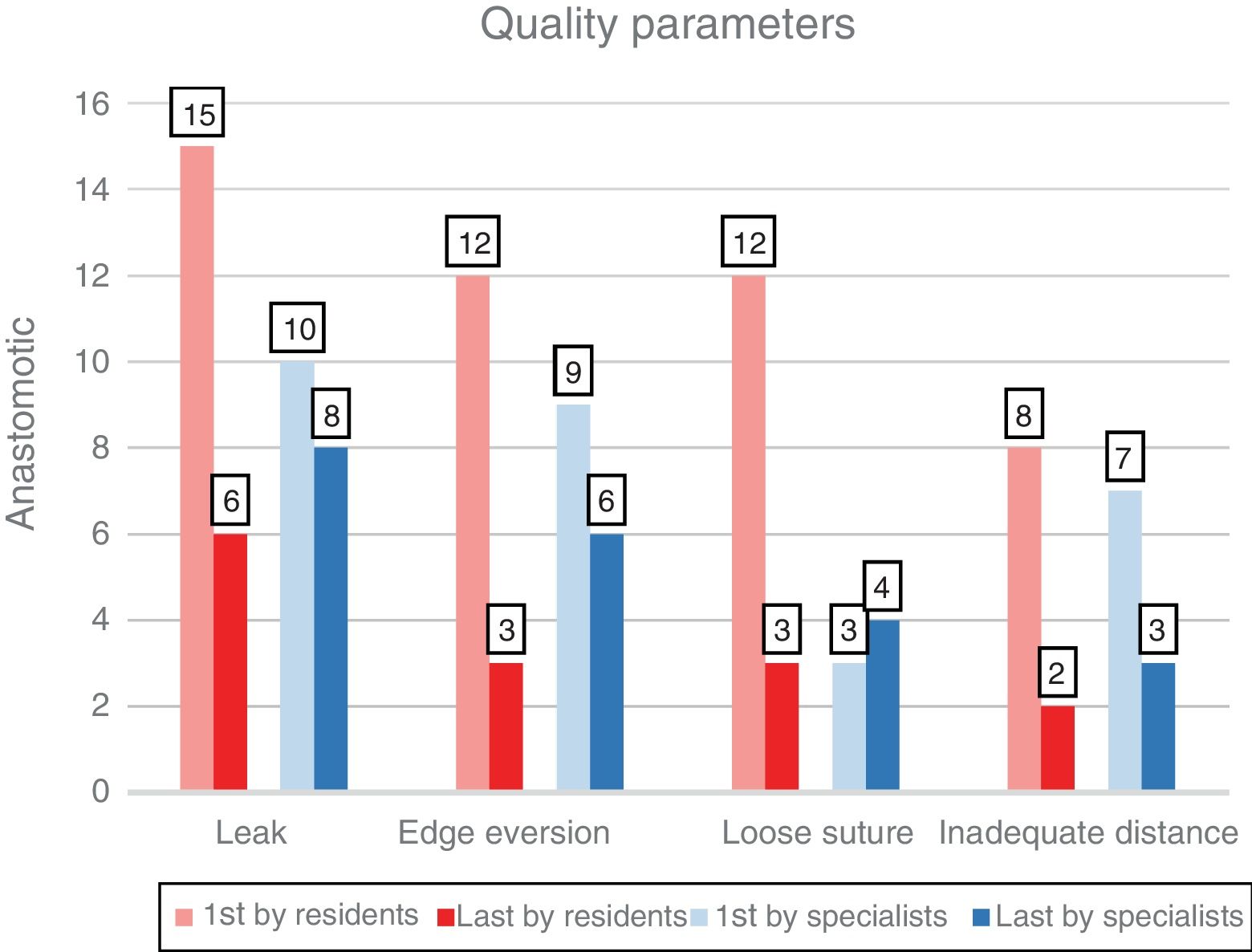
| Excessive distance (n) | 8 | 2 | .070 | 7 | 3 | .344 | .673 |
| Edge eversion (n) | 12 | 3 | .004 | 9 | 6 | .453 | .297 |
| Insufficient tension (n) | 12 | 3 | .012 | 3 | 4 | 1 | .728 |
| Leak (n) | 15 | 6 | .035 | 13 | 8 | .754 | .586 |
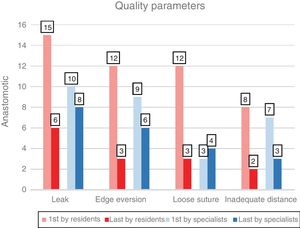
Regarding the quality of the anastomosis, improvements were achieved in the group of residents: 90% increase in adequate tension (P=.012), 75% reduction in everted edges (P=.004) and 60% in leaks (P=.035) (Fig. 5). In addition, the residents obtained final results comparable to the specialists (27.3% leak in the last anastomosis vs. 34.8% specialists, P=.5864).
The specialists reduced leakage by 20% (P=.754), eversion by 33.3% (P=.453) and the excessive distance between stitches by 57.1% (P=.344). The subgroup with greater previous experience (≥50 anastomoses) presented similar results, without reaching statistical significance in its improvement in terms of anastomotic quality.
DiscussionThe unquestionable importance of laparoscopy in current surgery today requires a change in the training of specialists and the teaching of this specialty to residents, as it has been gaining in importance in the formative stage.15 The implementation of simulation as a fundamental part of training is a highly valued, widely accepted resource16,17 with subsequent clinical repercussions.18
Since the Zendejas et al. study19 and a study carried out at our hospital by Ruiz Gómez,12 the utility of simulation seems to have been confirmed, and the need to standardize the teaching methodology has been suggested. Continuing with the basis of this latter study, we have sought to assess the influence of experience on the final results.
In the present study, we are able to confirm that intensive training in laparoscopic simulation leads to a significant improvement in terms of technical skill, procedural development and time in all participants, regardless of their educational level or previous experience.
Regarding the quality parameters, only the group of residents presented better final results in all the parameters analyzed.
In the group of specialists, the improvement of skills did not correlate with the best technical results, which may be a limitation of the sample size of the study.
When we compared the final overall results of the specialists and the residents, we found no differences, with a score of 20.6 and 21.3 respectively (P=.51).
Simulation in laparoscopy seems to be more effective in new participants, those with less clinical experience and residents.20,21 On one hand, students with a lower level of training would have a greater margin for improvement, while surgeons with greater clinical practice and experience may have acquired more rigid skills and theories, which are difficult to modify with simulation. Therefore, the need for a different methodology should be assessed once the technical training has been completed.
It would also be interesting to identify the characteristics of learning and whether the individual style of the participants (Kolb styles22) varies with age or experience. However, neither the Richard group23 with orthopedists nor the Engels group24 with general surgeons found significant differences between the learning styles of attending surgeons and residents.
Despite their demonstrated inferiority to distributed or spaced practice (short sessions with rest periods between them),25,26 we have demonstrated that these intensive courses (similar to the well-known ATLS, for example) provide novice participants (mostly residents) significant immersion in the skills, allowing them to acquire a final level of proficiency that is equal to that of the experts. As for participants with prior experience in these skills (mostly specialists), the course gives them a dose of reinforced training, which plays an important role in skill retention.
However, the exact amount of reinforcement for each surgical skill has not been studied. What we do know is that the simplest tasks require more reinforcement than more complex procedures.27 More studies on this point are needed, but what seems clear is that the concept of training beyond the objectives should be part of any motor skills curriculum in order to optimize the retention of skills acquired through simulation.28,29
Finally, the limitations of the study include the sample size, variability and possible subjectivity of the evaluations. To avoid this measurement bias, we selected the time period in which the same instructors always participated, so the number of participants could not be increased.
For all these reasons, our experience should be extended to more participants in order to expand the demographic, curricular and individual data to assimilate the information presented. In this way, learning patterns could be found in order to optimize and individualize teaching activities.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Toledo Martínez E, Martín Parra JI, Magadán Álvarez C, López Useros A, Fernández Santiago R, Regaño Díez S, et al. Influencia de la experiencia previa en los beneficios del entrenamiento quirúrgico laparoscópico basado en la simulación. Cir Esp. 2019;97:314–319.