Phytobezoars are hard masses of undigested plant material that accumulate in the stomach and small intestine. Although they may develop due to a fiber-rich diet in patients with poor teeth and insufficient chewing, and poor digestion due to gastric hypomotility and hypochlorhydria almost always present, with gastric stasis and vegetable fiber retention. This can occur as a consequence of previous gastrointestinal surgery, in cases of vagotomy with pyloroplasty or partial gastrectomy, and more rarely in other gastric motility disorders, such as diabetic gastroparesis, hypothyroidism or muscular dystrophy.
These masses can cause dyspeptic symptoms and can lead to complications, including digestive hemorrhage or gastric perforation. If they pass into the small intestine, a circumstance that is made easier when the pylorus is absent, an intestinal obstruction may occur.
Conventional treatment of bowel obstruction due to phytobezoar is surgical, by means of enterotomy and extraction. We present a case of complete intestinal obstruction due to a phytobezoar lodged in the distal ileum, which was successfully treated conservatively with the administration of cellulase through a nasogastric tube.
The patient was a 58-year-old male with a history of type 2 diabetes mellitus, HTN, hyperuricemia, previous vagotomy and pyloroplasty due to a bleeding peptic ulcer, appendectomy, septoplasty and arthroscopic meniscectomy. He had had bowel obstruction on 2 previous occasions due to phytobezoar impaction in the small intestine and had undergone surgical extraction of the bezoar by enterotomy. He was being treated with metformin, valsartan, allopurinol, pantoprazole, tetrazepam and metoclopramide.
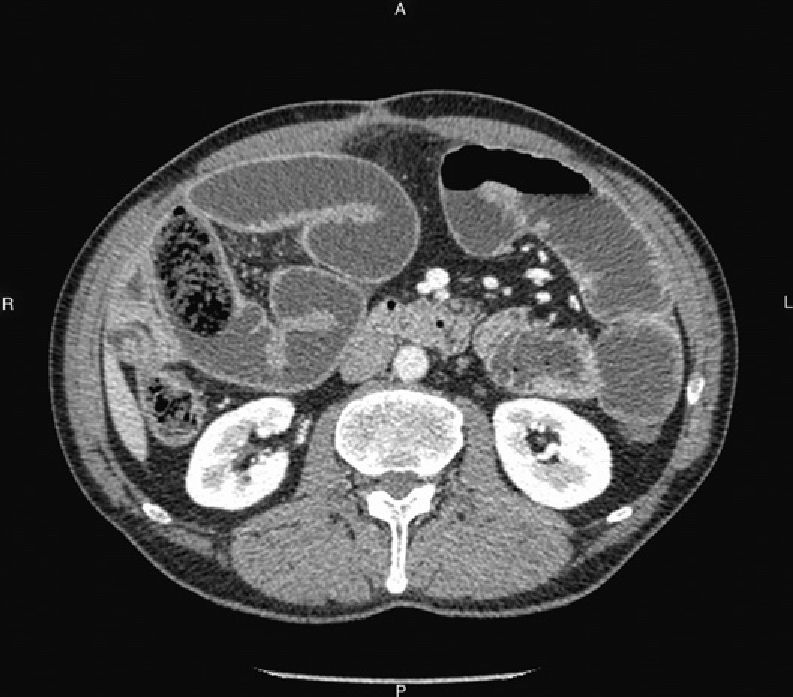
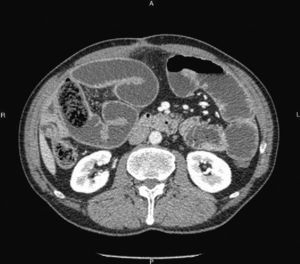
He came to our Emergency Department due to symptoms during the previous 36h that included pain, abdominal distension, nausea, vomiting and no bowel movements. Simple abdominal x-ray showed dilation of the loops of the small intestine with absence of distal gas, suggestive of intestinal obstruction. Abdominal CT (Fig. 1) showed intestinal obstruction due to a voluminous bezoar impacted in the distal ileum, accompanied by important distension of the intestinal loops. He was in good general condition and the work-up showed normal leukocyte count, mild neutrophilia and hyperglycemia, with the remaining parameters at normal levels.
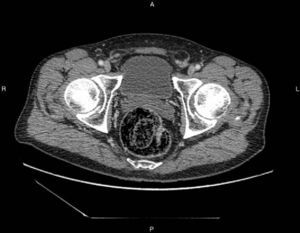
We decided to take a conservative approach and to try to dissolve the bezoar with cellulase. While waiting for the cellulase, treatment was initiated with bowel rest, nasogastric tube suction and total parenteral nutrition. The symptoms were tolerated by the patient, but there was complete intestinal closure. Intestinal suction was applied through the nasogastric tube, with clear worsening of the obstruction seen on radiological tests. On the 7th day of hospitalization, we began the administration of 5g of cellulase in 500cc of water per day through the nasogastric tube, which was clamped for 6h, in association with 10mg of intravenous metoclopramide. After the second day of treatment, the patient began to present multiple liquid stools and progressive normalization of the digestive transit, with resolution of the bowel obstruction symptoms. The treatment with cellulase was maintained for 5 days, after which oral intake was re-instated, with good tolerance. Simple abdominal radiograph showed a normal image and the CT scan (Fig. 2) demonstrated the disappearance of the signs of obstruction, with abundant feces in the colon and rectum and the bezoar in the rectal ampulla. During the rectal exam, the partially degraded bezoar was palpable; it was completely fragmented digitally and eliminated using enemas. The patient was discharged from the hospital.
In order to prevent new bezoars, we recommended a diet that was either very well chewed or puréed in a blender, especially the vegetables, along with metoclopramide before each meal and a Diet Coke each day. Two years later, the patient has had no new bezoars.
The composition of phytobezoars, whatever their plant origin, is basically made up of cellulose and hemicellulose adhered with proteinaceous cement. Attempts have been made at dissolving phytobezoars using different substances, either alone or in combination with endoscopic procedures. Coca-Cola has been used successfully,1–4 as has Diet Coke,1,2 which have likewise been recommended for preventing the formation of new phytobezoars in predisposed patients.3 Among the products with enzymatic effect, the most widely used has been cellulase, which has been proven effective in multiple studies with no adverse effects.5–8 Papain has also been used,5,9 although complications have been reported, such as gastric ulcers, esophageal perforation and hypernatremia.5
Cellulase is a specialized complex enzyme used for the hydrolysis of cellulose, breaking the leucoanthocyanidin-hemicellulose-cellulose links and transforming it into glucose. It is widely used in the food, textile and biofuel industries. It is not commercialized as a medication in Spain, so we acquired it from Fagron Ibérica (Terrassa, Barcelona; www.fagron.es).
Conservative treatment of phytobezoars, either endoscopic or with dissolution, has been used in gastric bezoars or in proximal portions of the small intestine, such as the efferent loop of a Billroth II gastrectomy.7 We have not found references about its use as a dissolvent in distal bezoars in the small intestine with bowel obstruction.
Although the treatment of bowel obstruction due to a bezoar is surgical, in selected cases with a firm diagnosis, good clinical tolerance, where decompression is possible through a nasogastric tube and in the absence of criteria of intestinal ischemia, the administration of cellulase could be an alternative.
Please cite this article as: Carreira Delgado M, Fernández Rodríguez E, Nuño Vázquez-Garza JM, Gil Llorens C, Vázquez López C. Oclusión intestinal por fitobezoar recidivante: resolución con tratamiento no operatorio mediante celulasa. Cir Esp. 2014;92(6):434–435.